J Korean Med Sci.
2022 Mar;37(9):e72. 10.3346/jkms.2022.37.e72.
Potential Utility of Fecal Calprotectin in Discriminating Colorectal Polyps From Other Major Etiologies in Children Presenting With Isolated Hematochezia
- Affiliations
-
- 1Department of Pediatrics, Ajou University Medical Center, Suwon, Korea
- 2Department of Pediatrics, Eulji University Hospital, Daejeon, Korea
- 3Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 4Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 5Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 6Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 7Department of Pediatrics, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 8Department of Pediatrics, Nowon Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea
- 9Department of Pediatrics, Hallym University College of Medicine, Chuncheon, Korea
- 10Department of Pediatrics, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- 11Department of Pediatrics, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 12Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 13Department of Pediatrics, Chung-Ang University Hospital, College of Medicine, Chung-Ang University, Seoul, Korea
- 14Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea
- KMID: 2526970
- DOI: http://doi.org/10.3346/jkms.2022.37.e72
Abstract
- Background
Colorectal polyps are the most common cause of isolated hematochezia in children, which requires a colonoscopy for diagnosis. We aimed to investigate the potential utility of fecal calprotectin (FC) in assessing colorectal polyps detected by colonoscopy among children presenting with isolated hematochezia.
Methods
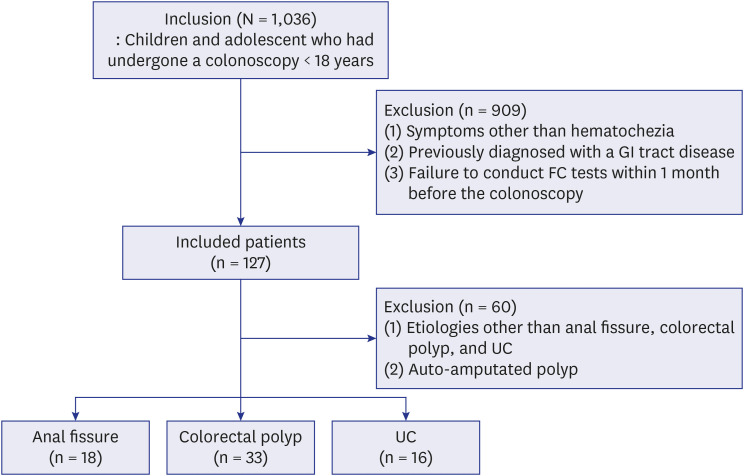
Pediatric patients of the age of < 18 years who had undergone both colonoscopy and FC tests for isolated hematochezia from June 2016 to May 2020 were included in the present multicenter, retrospective, cross-sectional study. Comparative analysis was conducted between major causes of isolated hematochezia and FC cut-offs for discriminating colorectal polyps were explored.
Results
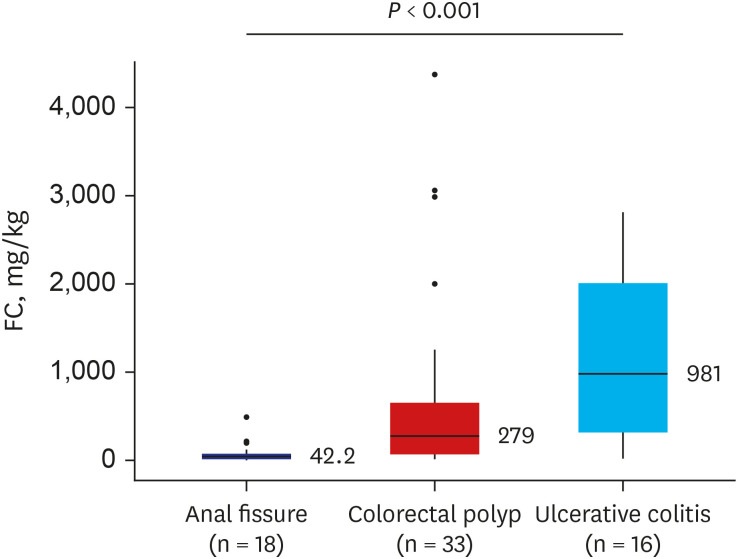
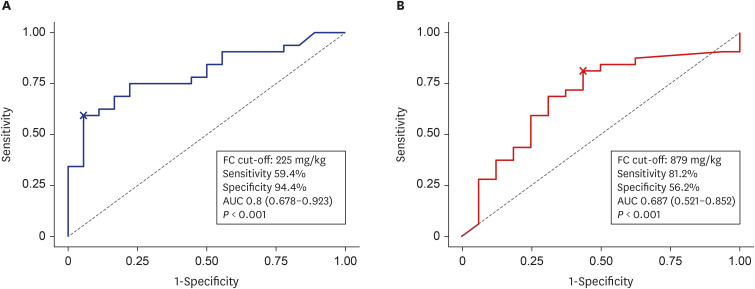
A total 127 patients were included. Thirty-five patients (27.6%) had colorectal polyps, followed by anal fissure (14.2%), ulcerative colitis (UC; 12.6%), and others. A significant difference in FC levels was observed between patients with colorectal polyps (median, 278.7 mg/kg), anal fissures (median, 42.2 mg/kg), and UC (median, 981 mg/ kg) (P < 0.001). According to receiver operating characteristic curve analysis, among patients diagnosed with colorectal polyp or anal fissure, the most accurate FC cut-off for discriminating colorectal polyps from anal fissures on colonoscopy was 225 mg/kg (sensitivity, 59.4%; specificity, 94.4%; positive predictive value [PPV], 95.0%; negative predictive value [NPV], 56.7%; area under the curve [AUC], 0.8; 95% confidence interval [CI], 0.678–0.923; P < 0.001), while among patients diagnosed with colorectal polyp or UC, the most accurate FC cut-off for discriminating colorectal polyps from UC on colonoscopy was 879 mg/kg (sensitivity, 81.2%; specificity, 56.2%; PPV, 78.8%; NPV, 60.0%; AUC, 0.687; 95% CI, 0.521–0.852; P < 0.001).
Conclusion
FC may assist in assessing the cause of lower gastrointestinal tract bleeding in children who present with isolated hematochezia.
Figure
Reference
-
1. Silbermintz A, Matar M, Assa A, Zevit N, Glassberg YM, Shamir R. Endoscopic findings in children with isolated lower gastrointestinal bleeding. Clin Endosc. 2019; 52(3):258–261. PMID: 31085966.
Article2. Lee YJ, Park JH. The most common cause of lower gastrointestinal bleeding without other symptoms in children is colonic polyp: is total colonoscopy needed? Clin Endosc. 2019; 52(3):207–208. PMID: 31121995.
Article3. Lee BG, Shin SH, Lee YA, Wi JH, Lee YJ, Park JH. Juvenile polyp and colonoscopic polypectomy in childhood. Pediatr Gastroenterol Hepatol Nutr. 2012; 15(4):250–255. PMID: 24010095.
Article4. Kim DY, Bae JY, Ko KO, Cheon EJ, Lim JW, Song YH, et al. Juvenile polyp associated with hypovolemic shock due to massive lower gastrointestinal bleeding. Pediatr Gastroenterol Hepatol Nutr. 2019; 22(6):613–618. PMID: 31777730.
Article5. Sahn B, Bitton S. Lower gastrointestinal bleeding in children. Gastrointest Endosc Clin N Am. 2016; 26(1):75–98. PMID: 26616898.
Article6. D’Haens G, Ferrante M, Vermeire S, Baert F, Noman M, Moortgat L, et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012; 18(12):2218–2224. PMID: 22344983.
Article7. Lee YM, Choi S, Choe BH, Jang HJ, Kim S, Koh H, et al. Association between fecal calprotectin and mucosal healing in pediatric patients with Crohn’s disease who have achieved sustained clinical remission with anti-tumor necrosis factor agents. Gut Liver. 2022; 16(1):62–70. PMID: 33833135.
Article8. Koninckx CR, Donat E, Benninga MA, Broekaert IJ, Gottrand F, Kolho KL, et al. The use of fecal calprotectin testing in paediatric disorders: a position paper of the European Society for Paediatric Gastroenterology and Nutrition Gastroenterology Committee. J Pediatr Gastroenterol Nutr. 2021; 72(4):617–640. PMID: 33716293.
Article9. Pauley-Hunter RJ, Kunnath S, Wolff K, Vanderhoof JA. Fecal calprotectin and pediatric juvenile polyps. J Pediatr Gastroenterol Nutr. 2015; 60(4):e30–e31. PMID: 24048165.
Article10. Olafsdottir I, Nemeth A, Lörinc E, Toth E, Agardh D. Value of fecal calprotectin as a biomarker for juvenile polyps in children investigated with colonoscopy. J Pediatr Gastroenterol Nutr. 2016; 62(1):43–46. PMID: 26147630.
Article11. Di Nardo G, Esposito F, Ziparo C, Strisciuglio C, Vassallo F, Di Serafino M, et al. Faecal calprotectin and ultrasonography as non-invasive screening tools for detecting colorectal polyps in children with sporadic rectal bleeding: a prospective study. Ital J Pediatr. 2020; 46(1):66. PMID: 32434534.
Article12. Das SR, Karim AS, RukonUzzaman M, Mazumder MW, Alam R, Benzamin M, et al. Juvenile polyps in Bangladeshi children and their association with fecal calprotectin as a biomarker. Pediatr Gastroenterol Hepatol Nutr. 2022; 25(1):52–60. PMID: 35087733.
Article13. Campbell AM, Sugarman I. Does painless rectal bleeding equate to a colonic polyp? Arch Dis Child. 2017; 102(11):1049–1051. PMID: 28550146.
Article14. Jeong SJ. The role of fecal calprotectin in pediatric disease. Korean J Pediatr. 2019; 62(8):287–291. PMID: 30999729.
Article16. Yoo IH, Cho JM, Joo JY, Yang HR. Fecal calprotectin as a useful non-invasive screening marker for eosinophilic gastrointestinal disorder in Korean children. J Korean Med Sci. 2020; 35(17):e120. PMID: 32356420.
Article16. Cozijnsen MA, Ben Shoham A, Kang B, Choe BH, Choe YH, Jongsma MM, et al. Development and validation of the mucosal inflammation noninvasive index for pediatric Crohn’s disease. Clin Gastroenterol Hepatol. 2020; 18(1):133–140.e1. PMID: 30981008.
Article17. Hyer W. Pediatric polyposis syndrome. Wyllie R, Hyams JS, Kay M, editors. Pediatric Gastrointestinal and Liver Disease. 5th ed. Philadelphia, PA, USA: Elsevier;2016. p. 496–507.18. Prell C, Nagel D, Freudenberg F, Schwarzer A, Koletzko S. Comparison of three tests for faecal calprotectin in children and young adults: a retrospective monocentric study. BMJ Open. 2014; 4(5):e004558.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of Fecal Neutrophil Gelatinase-Associated Lipocalin and Calprotectin as Biomarkers of Clostridioides (Clostridium) difficile Infection
- Resection of Diminutive and Small Colorectal Polyps: What Is the Optimal Technique?
- Juvenile Polyps in Bangladeshi Children and Their Association with Fecal Calprotectin as a Biomarker
- Usefulness of fecal immunochemical test and fecal calprotectin for detection of active ulcerative colitis
- Role of Fecal Calprotectin in Differentiating between Hirschsprung's Disease and Functional Constipation