J Korean Med Sci.
2022 Mar;37(9):e71. 10.3346/jkms.2022.37.e71.
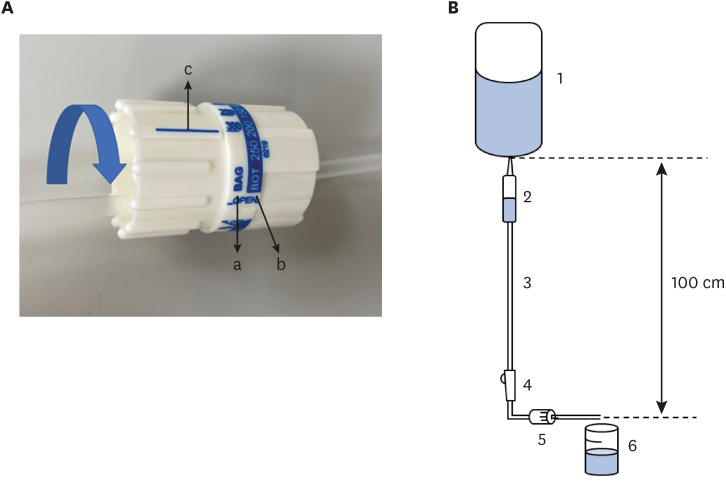
The Effects of Intravenous Fluid Viscosity on the Accuracy of Intravenous Infusion Flow Regulators
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Korea University Anam Hospital, Seoul, Korea
- 2College of Medicine, Korea University, Seoul, Korea
- 3Department of Biomedical Engineering, College of Medicine, Korea University, Seoul, Korea
- 4Department of Biomedical Science and Engineering, School of Mechanical Engineering, Gwangju Institute of Science and Technology, Gwangju, Korea
- KMID: 2526969
- DOI: http://doi.org/10.3346/jkms.2022.37.e71
Abstract
- Intravenous infusion flow regulators (IIFRs) are widely used devices but it is unknown how much the difference between the IIFR scale and the actual flow rate depends on the viscosity of the intravenous (IV) fluid. This study evaluated the effects of viscosity on the flow rate of five IV fluids (0.9% normal saline, Hartmann’s solution, plasma solution-A, 6% hetastarch, and 5% albumin) when using IIFRs. The viscosity of crystalloids was 1.07–1.12 mPa·s, and the viscosities of 6% hetastarch and 5% albumin were 2.59 times and 1.74 times that of normal saline, respectively. When the IIFR scales were preset to 20, 100, and 250 mL/hr, crystalloids were delivered at the preset flow rate within a difference of less than 10%, while 6% hetastarch was delivered at approximately 40% of the preset flow rates and 5% albumin was approximately 80% transmitted. When delivering colloids, IIFRs should be used with caution.
Figure
Reference
-
1. Doherty M, Buggy DJ. Intraoperative fluids: how much is too much? Br J Anaesth. 2012; 109(1):69–79. PMID: 22661747.
Article2. Bundgaard-Nielsen M, Secher NH, Kehlet H. ‘Liberal’ vs. ‘restrictive’ perioperative fluid therapy--a critical assessment of the evidence. Acta Anaesthesiol Scand. 2009; 53(7):843–851. PMID: 19519723.
Article3. Hoste EA, Maitland K, Brudney CS, Mehta R, Vincent JL, Yates D, et al. Four phases of intravenous fluid therapy: a conceptual model. Br J Anaesth. 2014; 113(5):740–747. PMID: 25204700.4. Caruba T, Havard L, Gillaizeau F, Guérot E, Prognon P, Pineau J. Evaluation of flow rate regulators for intravenous infusion. Ann Fr Anesth Reanim. 2009; 28(11):936–942. PMID: 19939620.5. Stoneham MD. An evaluation of methods of increasing the flow rate of i.v. fluid administration. Br J Anaesth. 1995; 75(3):361–365. PMID: 7547060.
Article6. Berman DJ, Schiavi A, Frank SM, Duarte S, Schwengel DA, Miller CR. Factors that influence flow through intravascular catheters: the clinical relevance of Poiseuille’s law. Transfusion. 2020; 60(7):1410–1417. PMID: 32643172.
Article7. Khoyratty SI, Gajendragadkar PR, Polisetty K, Ward S, Skinner T, Gajendragadkar PR. Flow rates through intravenous access devices: an in vitro study. J Clin Anesth. 2016; 31:101–105. PMID: 27185686.
Article8. Loner C, Acquisto NM, Lenhardt H, Sensenbach B, Purick J, Jones CM, et al. Accuracy of intravenous infusion flow regulators in the prehospital environment. Prehosp Emerg Care. 2018; 22(5):645–649. PMID: 29465284.
Article9. Feldheiser A, Pavlova V, Bonomo T, Jones A, Fotopoulou C, Sehouli J, et al. Balanced crystalloid compared with balanced colloid solution using a goal-directed haemodynamic algorithm. Br J Anaesth. 2013; 110(2):231–240. PMID: 23112214.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy and Continuity of Infusion Devices with Volumetric Analyzer
- A Report for the Research about the Accuracy of a flow Regulator
- The Effects of Vehicle Movement/ Operation on Fluid Flow Regulators During Patient Transport
- A Case of Acute Hepatitis Associated with Intravenous Infusion Amiodarone in Patient with Atrial Fibrillation
- Measarement of Drop Factor of IV Infusion Set with Infusion Pump