Ann Hepatobiliary Pancreat Surg.
2022 Feb;26(1):113-117. 10.14701/ahbps.21-071.
Curative intent radical cholecystectomy followed by hyperthermic intraperitoneal chemotherapy in ruptured intraductal papillary neoplasm of gallbladder with invasive carcinoma
- Affiliations
-
- 1Yonsei University College of Medicine, Seoul, Korea
- 2Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Surgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 4Division of Colorectal Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2526840
- DOI: http://doi.org/10.14701/ahbps.21-071
Abstract
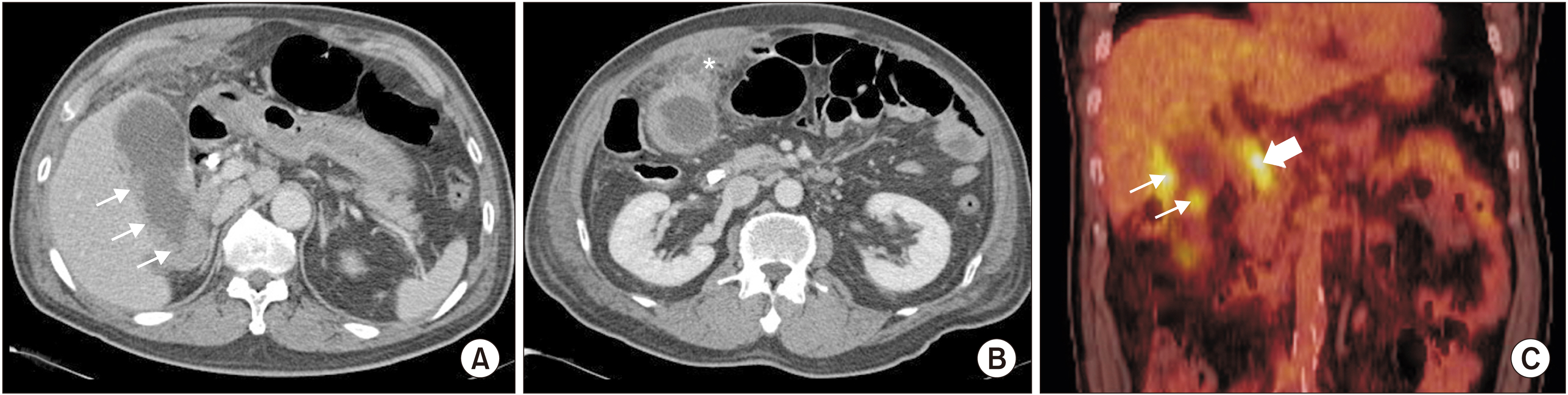
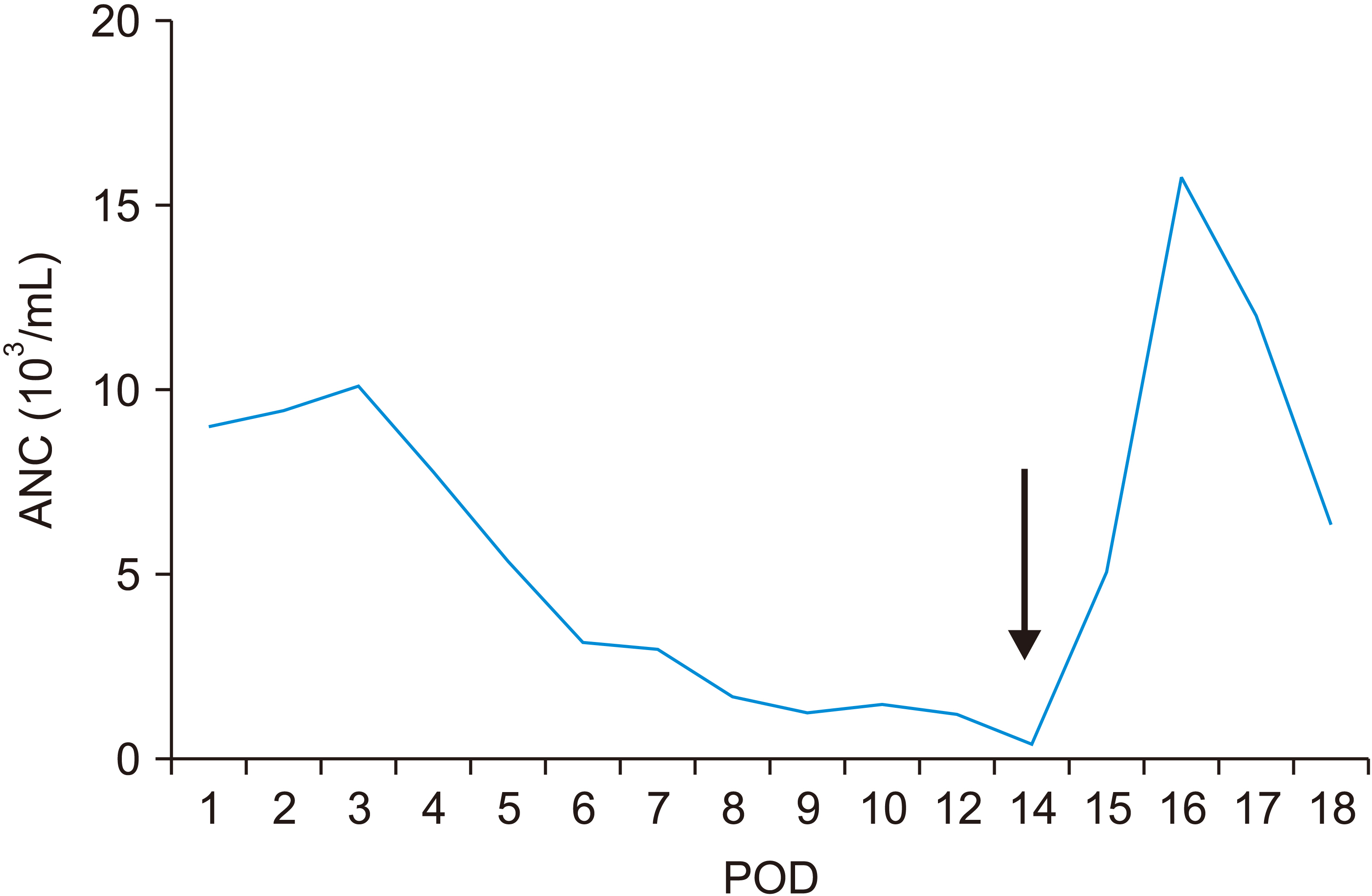
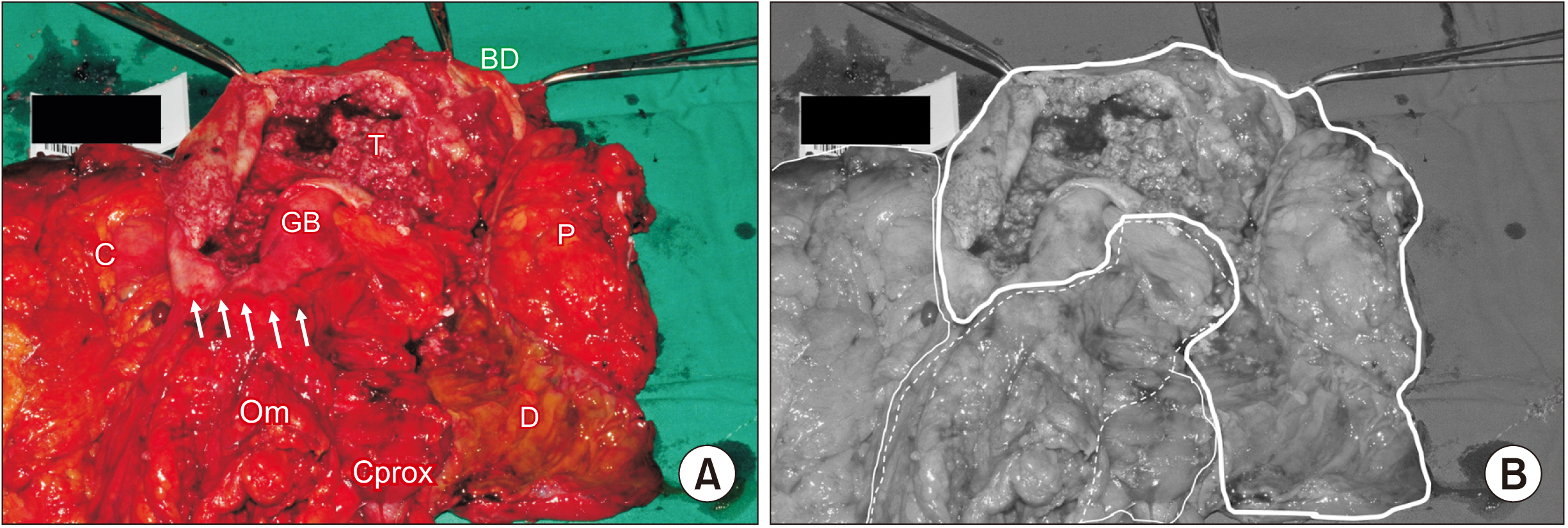
- Gallbladder cancer has a poor prognosis, especially in peritoneal carcinomatosis related to perforation of the gallbladder followed by bile spillage. Previously, curative-intent treatment was not considered in carcinomatosis from cancer of the biliary tract. A 72-year-old male was referred to the hospital with a perforated gallbladder cancer. Intraoperatively, the tumor was confined to the gallbladder and liver. We presented a case of intention-to-curative resection of perforated gallbladder cancer followed by intraoperative hyperthermic intraperitoneal chemotherapy.
Keyword
Figure
Reference
-
1. Kim YJ, Kim K. 2017; Conditional survival in patients with gallbladder cancer. Chin J Cancer. 36:85. DOI: 10.1186/s40880-017-0252-1. PMID: 29084608. PMCID: PMC5663056.
Article2. Nishio H, Nagino M, Ebata T, Yokoyama Y, Igami T, Nimura Y. 2007; Aggressive surgery for stage IV gallbladder carcinoma; what are the contraindications? J Hepatobiliary Pancreat Surg. 14:351–357. DOI: 10.1007/s00534-006-1187-0. PMID: 17653632.
Article3. van Driel WJ, Koole SN, Sikorska K, Schagen van Leeuwen JH, Schreuder HWR, Hermans RHM, et al. 2018; Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med. 378:230–240. DOI: 10.1056/NEJMoa1708618. PMID: 29342393.
Article4. Vanounou T, Garfinkle R. 2016; Evaluation of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis of colorectal origin in the era of value-based medicine. Ann Surg Oncol. 23:2556–2561. DOI: 10.1245/s10434-016-5096-4. PMID: 26957499.
Article5. Goéré D, Passot G, Gelli M, Levine EA, Bartlett DL, Sugarbaker PH, et al. 2017; Complete cytoreductive surgery plus HIPEC for peritoneal metastases from unusual cancer sites of origin: results from a worldwide analysis issue of the Peritoneal Surface Oncology Group International (PSOGI). Int J Hyperthermia. 33:520–527. DOI: 10.1080/02656736.2017.1301576. PMID: 28540827.
Article6. Glehen O, Gilly FN, Boutitie F, Bereder JM, Quenet F, Sideris L, et al. 2010; Toward curative treatment of peritoneal carcinomatosis from nonovarian origin by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy: a multi-institutional study of 1,290 patients. Cancer. 116:5608–5618. DOI: 10.1002/cncr.25356. PMID: 20737573.
Article7. Levine EA, Stewart JH 4th, Russell GB, Geisinger KR, Loggie BL, Shen P. 2007; Cytoreductive surgery and intraperitoneal hyperthermic chemotherapy for peritoneal surface malignancy: experience with 501 procedures. J Am Coll Surg. 204:943–953. discussion 953–955. DOI: 10.1016/j.jamcollsurg.2006.12.048. PMID: 17481516.
Article8. Glockzin G, Renner P, Popp FC, Dahlke MH, von Breitenbuch P, Schlitt HJ, et al. 2011; Hepatobiliary procedures in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 18:1052–1059. DOI: 10.1245/s10434-010-1415-3. PMID: 21046262.
Article9. Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D'Angelica MI, et al. 2012; Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 56:1352–1360. DOI: 10.1002/hep.25786. PMID: 22504729.
Article10. Nakanuma Y, Kakuda Y, Uesaka K. 2019; Characterization of intraductal papillary neoplasm of the bile duct with respect to the histopathologic similarities to pancreatic intraductal papillary mucinous neoplasm. Gut Liver. 13:617–627. DOI: 10.5009/gnl18476. PMID: 30982236. PMCID: PMC6860037.
Article11. Wasif N, Bentrem DJ, Farrell JJ, Ko CY, Hines OJ, Reber HA, et al. 2010; Invasive intraductal papillary mucinous neoplasm versus sporadic pancreatic adenocarcinoma: a stage-matched comparison of outcomes. Cancer. 116:3369–3377. DOI: 10.1002/cncr.25070. PMID: 20564064. PMCID: PMC2902567.
Article12. Choi M, Chong JU, Hwang HK, Seo HI, Yang K, Ryu JH, et al. 2021; Role of postoperative adjuvant therapy in resected invasive intraductal papillary mucinous neoplasm of the pancreas: a multicenter external validation. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.996 [in press]. DOI: 10.1002/jhbp.996. PMID: 34028187.
Article13. Bennett S, Marginean EC, Paquin-Gobeil M, Wasserman J, Weaver J, Mimeault R, et al. 2015; Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder. HPB (Oxford). 17:811–818. DOI: 10.1111/hpb.12460. PMID: 26278323. PMCID: PMC4557656.
Article14. Castelo Branco M, Estevinho F, Correia Pinto J, Honavar M, Raposo C, Silva AC, et al. 2019; Gallbladder cancer: complete resection after second line treatment in stage IV disease. J Gastrointest Cancer. 50:564–567. DOI: 10.1007/s12029-017-0044-5. PMID: 29292472.
Article15. Kuga D, Ebata T, Yokoyama Y, Igami T, Sugawara G, Mizuno T, et al. 2017; Long-term survival after multidisciplinary therapy for residual gallbladder cancer with peritoneal dissemination: a case report. Surg Case Rep. 3:76. DOI: 10.1186/s40792-017-0351-x. PMID: 28616794. PMCID: PMC5471273.
Article16. Kang MJ, Song Y, Jang JY, Han IW, Kim SW. 2012; Role of radical surgery in patients with stage IV gallbladder cancer. HPB (Oxford). 14:805–811. DOI: 10.1111/j.1477-2574.2012.00544.x. PMID: 23134181. PMCID: PMC3521908.
Article17. Randle RW, Levine EA, Clark CJ, Stewart JH, Shen P, Votanopoulos KI. 2014; Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for gallbladder cancer: a retrospective review. Am Surg. 80:710–713. DOI: 10.1177/000313481408000728. PMID: 24987905.
Article18. Kwon W, Kim H, Han Y, Hwang YJ, Kim SG, Kwon HJ, et al. 2020; Role of tumour location and surgical extent on prognosis in T2 gallbladder cancer: an international multicentre study. Br J Surg. 107:1334–1343. DOI: 10.1002/bjs.11618. PMID: 32452559.
Article19. Yuza K, Sakata J, Prasoon P, Hirose Y, Ohashi T, Toge K, et al. 2020; Longterm outcomes of surgical resection for T1b gallbladder cancer: an institutional evaluation. BMC Cancer. 20:20. DOI: 10.1186/s12885-019-6507-2. PMID: 31907021. PMCID: PMC6945689.
Article20. Navarro JG, Kang I, Hwang HK, Yoon DS, Lee WJ, Kang CM. 2020; Oncologic safety of laparoscopic radical cholecystectomy in pT2 gallbladder cancer: a propensity score matching analysis compared to open approach. Medicine (Baltimore). 99:e20039. DOI: 10.1097/MD.0000000000020039. PMID: 32443308. PMCID: PMC7253605.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Small cell carcinoma of the gallbladder: a case report
- Analysis of Clinical Outcome and Prognostic Factors in Patients with Gallbladder Cancer
- Surgical outcome and prognostic factors in patients with gallbladder carcinoma
- What is your initial surgical procedure for suspicious T2 gallbladder cancer? - Minimally invasive surgery.
- Synchronous Undifferentiated Carcinoma of Gallbladder in a Patient with Intrahepatic Intraductal Papillary Mucinous Neoplasia (b-IPMN)