J Korean Assoc Oral Maxillofac Surg.
2022 Feb;48(1):13-20. 10.5125/jkaoms.2022.48.1.13.
Epistaxis in dental and maxillofacial practice: a comprehensive review
- Affiliations
-
- 11st Academic ENT Department, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki, Greece.
- 21st Propedeutic Department of Internal Medicine, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki, Greece.
- 3School of Dentistry, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki, Greece.
- KMID: 2526806
- DOI: http://doi.org/10.5125/jkaoms.2022.48.1.13
Abstract
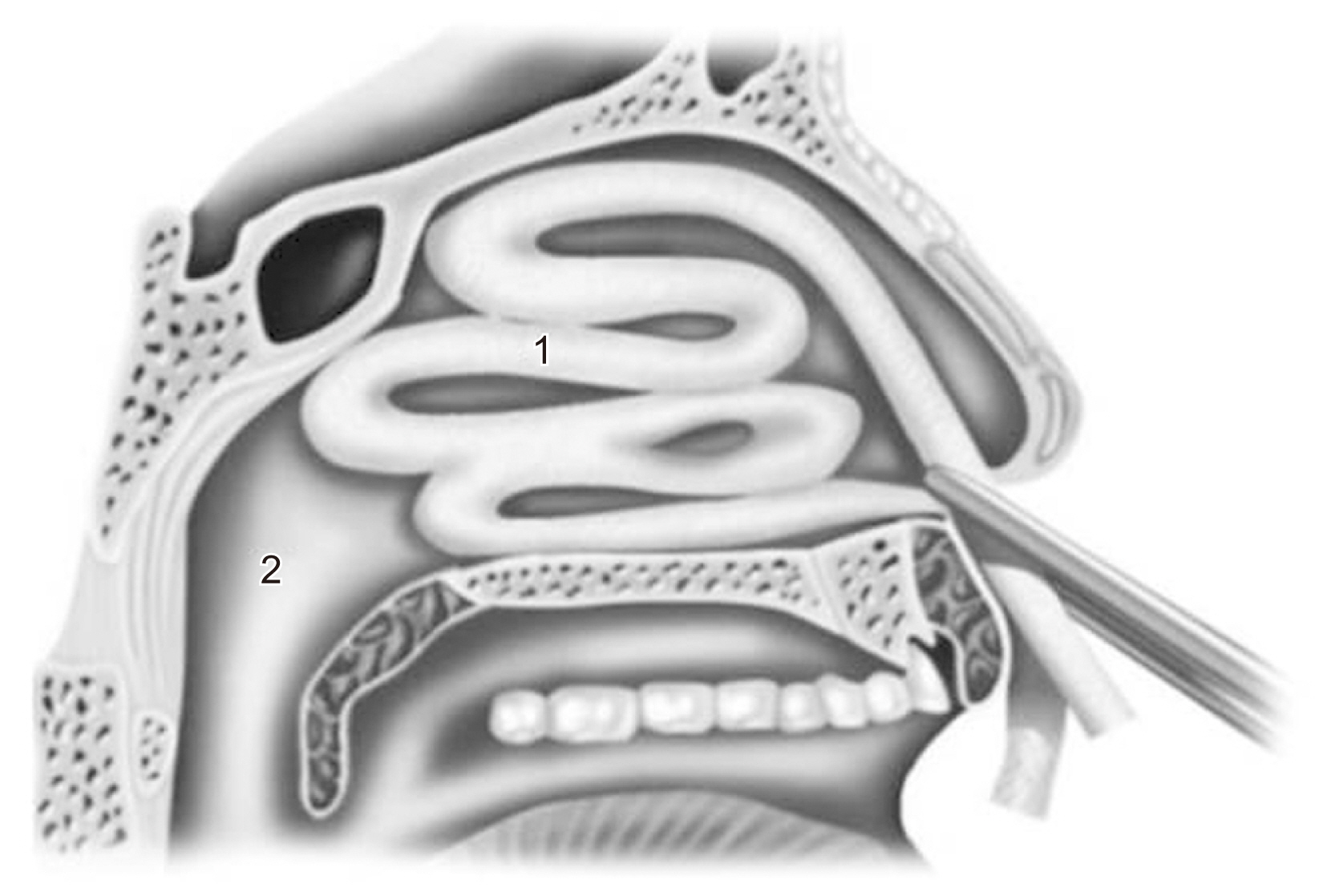
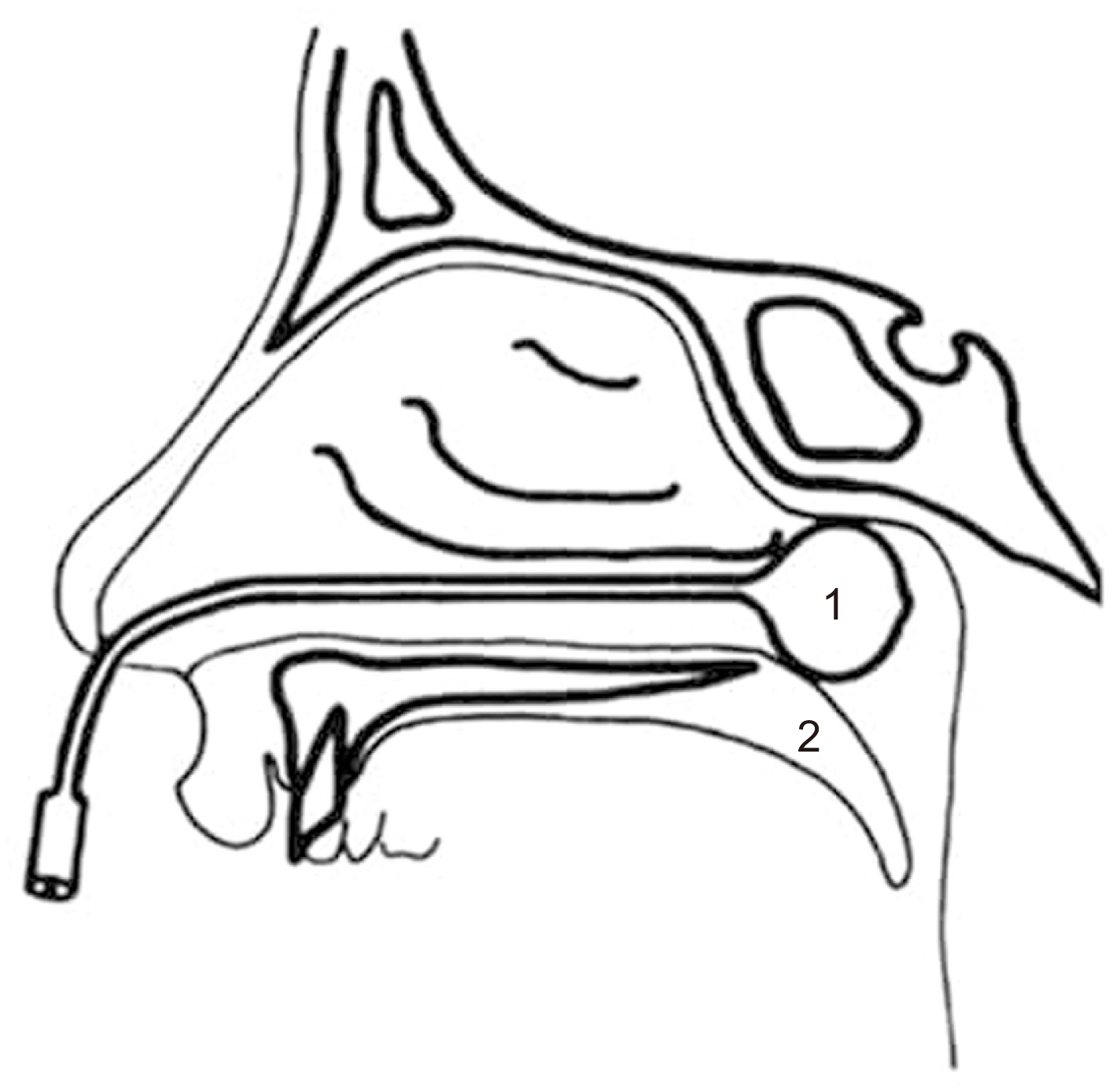
- The lifetime incidence of epistaxis in dental and maxillofacial practice has been reported to be as high as 60% and can be caused by dental implant placement, Le Fort I osteotomy, intranasal supernumerary tooth, odontogenic tumors, blood disorders and maxillofacial trauma. Most epistaxis cases are minor and easily managed with direct compression on the nares for 10 minutes. For more significant or recurrent epistaxis, other techniques might include electrocautery, anterior or posterior nasal packing, or Foley catheter balloon. For patients with refractory epistaxis, cauterization of the sphenopalatine artery under endonasal endoscopy or embolization of the internal maxillary artery should be performed. Epistaxis control is required in patients diagnosed with inherited or acquired bleeding disorders or with drug-induced coagulopathies during dental procedures. In these cases, hemostatic system adjustment and hemostasis achieved by local and adjunctive methods are required. Dentists and maxillofacial surgeons must be aware that the nasal cavity is a potential source of perioperative hemorrhage. Depending on the invasiveness of the dental intervention, preoperative involvement of the hematologist and cardiologist is usually necessary to reverse anticoagulation or to cease anticoagulant therapy.
Figure
Reference
-
References
1. Morgan DJ, Kellerman R. 2014; Epistaxis: evaluation and treatment. Prim Care. 41:63–73. https://doi.org/10.1016/j.pop.2013.10.007. DOI: 10.1016/j.pop.2013.10.007. PMID: 24439881.
Article2. Solomons NB, Blumgart R. 1988; Severe late-onset epistaxis following Le Fort I osteotomy: angiographic localization and embolization. J Laryngol Otol. 102:260–3. https://doi.org/10.1017/s0022215100104670. DOI: 10.1017/S0022215100104670. PMID: 3356937.
Article3. Krulewitz NA, Fix ML. 2019; Epistaxis. Emerg Med Clin North Am. 37:29–39. https://doi.org/10.1016/j.emc.2018.09.005. DOI: 10.1016/j.emc.2018.09.005. PMID: 30454778.
Article4. Tatum H Jr. 1986; Maxillary and sinus implant reconstructions. Dent Clin North Am. 30:207–29. PMID: 3516738.5. Ferguson M. 2014; Rhinosinusitis in oral medicine and dentistry. Aust Dent J. 59:289–95. https://doi.org/10.1111/adj.12193. DOI: 10.1111/adj.12193. PMID: 24861778.
Article6. Stacchi C, Andolsek F, Berton F, Perinetti G, Navarra CO, Di Lenarda R. 2017; Intraoperative complications during sinus floor elevation with lateral approach: a systematic review. Int J Oral Maxillofac Implants. 32:e107–18. https://doi.org/10.11607/jomi.4884. DOI: 10.11607/jomi.4884. PMID: 28494033.
Article7. Alberti PW. 1976; Applied surgical anatomy of the maxillary sinus. Otolaryngol Clin North Am. 9:3–20. DOI: 10.1016/S0030-6665(20)32713-4. PMID: 1246431.
Article8. Hong YH, Mun SK. 2011; A case of massive maxillary sinus bleeding after dental implant. Int J Oral Maxillofac Surg. 40:758–60. https://doi.org/10.1016/j.ijom.2010.11.027. DOI: 10.1016/j.ijom.2010.11.027. PMID: 21377328.
Article9. Nooh N. 2013; Effect of schneiderian membrane perforation on posterior maxillary implant survival. J Int Oral Health. 5:28–34. PMID: 24155599. PMCID: PMC3769876.10. Kim HY, Yang JY, Chung BY, Kim JC, Yeo IS. 2013; Peri-implant bone length changes and survival rates of implants penetrating the sinus membrane at the posterior maxilla in patients with limited vertical bone height. J Periodontal Implant Sci. 43:58–63. https://doi.org/10.5051/jpis.2013.43.2.58. DOI: 10.5051/jpis.2013.43.2.58. PMID: 23678388. PMCID: PMC3651938.
Article11. Shihab OI. 2017; Intentional penetration of dental implants into the maxillary sinus: a retrospective study. Zanco J Med Sci. 21:1536–9. https://doi.org/10.15218/zjms.2017.001. DOI: 10.15218/zjms.2017.001.
Article12. Bae OY, Kim YS, Shin SY, Kim WK, Lee YK, Kim SH. 2015; Clinical outcomes of reamer- vs osteotome-mediated sinus floor elevation with simultaneous implant placement: a 2-year retrospective study. Int J Oral Maxillofac Implants. 30:925–30. https://doi.org/10.11607/jomi.3779. DOI: 10.11607/jomi.3779. PMID: 26252045.
Article13. Lanigan DT, Hey JH, West RA. 1990; Major vascular complications of orthognathic surgery: hemorrhage associated with Le Fort I osteotomies. J Oral Maxillofac Surg. 48:561–73. https://doi.org/10.1016/s0278-2391(10)80468-9. DOI: 10.1016/S0278-2391(10)80468-9. PMID: 2341936.
Article14. Mehra P, Cottrell DA, Caiazzo A, Lincoln R. 1999; Life-threatening, delayed epistaxis after surgically assisted rapid palatal expansion: a case report. J Oral Maxillofac Surg. 57:201–4. https://doi.org/10.1016/s0278-2391(99)90241-0. DOI: 10.1016/S0278-2391(99)90241-0. PMID: 9973133.
Article15. Williams BJ, Currimbhoy S, Silva A, O'Ryan FS. 2012; Complications following surgically assisted rapid palatal expansion: a retrospective cohort study. J Oral Maxillofac Surg. 70:2394–402. https://doi.org/10.1016/j.joms.2011.09.050. DOI: 10.1016/j.joms.2011.09.050. PMID: 22516838.
Article16. de Mol van Otterloo JJ, Tuinzing DB, Greebe RB, van der Kwast WA. 1991; Intra- and early postoperative complications of the Le Fort I osteotomy. A retrospective study on 410 cases. J Craniomaxillofac Surg. 19:217–22. https://doi.org/10.1016/s1010-5182(05)80551-7. DOI: 10.1016/S1010-5182(05)80551-7. PMID: 1894740.
Article17. Eshghpour M, Mianbandi V, Samieirad S. 2018; Intra- and postoperative complications of Le Fort I maxillary osteotomy. J Craniofac Surg. 29:e797–803. https://doi.org/10.1097/SCS.0000000000004828. DOI: 10.1097/SCS.0000000000004828. PMID: 30277955.
Article18. Avelar RL, Goelzer JG, Becker OE, de Oliveira RB, Raupp EF, de Magalhães PS. 2010; Embolization of pseudoaneurysm of the internal maxillary artery after orthognathic surgery. J Craniofac Surg. 21:1764–8. https://doi.org/10.1097/SCS.0b013e3181f40393. DOI: 10.1097/SCS.0b013e3181f40393. PMID: 21119417.
Article19. Park B, Jang WH, Lee BK. 2019; An idiopathic delayed maxillary hemorrhage after orthognathic surgery with Le Fort I osteotomy: a case report. J Korean Assoc Oral Maxillofac Surg. 45:364–8. https://doi.org/10.5125/jkaoms.2019.45.6.364. DOI: 10.5125/jkaoms.2019.45.6.364. PMID: 31966982. PMCID: PMC6955418.
Article20. Garg S, Kaur S. 2014; Evaluation of post-operative complication rate of Le Fort I osteotomy: a retrospective and prospective study. J Maxillofac Oral Surg. 13:120–7. https://doi.org/10.1007/s12663-012-0457-4. DOI: 10.1007/s12663-012-0457-4. PMID: 24822002. PMCID: PMC4016385.
Article21. Niazi MH, El-Ghanem M, Al-Mufti F, Wajswol E, Dodson V, Abdulrazzaq A, et al. 2018; Endovascular management of epistaxis secondary to dissecting pseudoaneurysm of the descending palatine artery following orthognathic surgery. J Vasc Interv Neurol. 10:41–6. PMID: 30746009. PMCID: PMC6350872.22. Bykowski MR, Hill A, Garland C, Tobler W, Losee JE, Goldstein JA. 2018; Ruptured pseudoaneurysm of the maxillary artery and its branches following Le Fort I osteotomy: evidence-based guidelines. J Craniofac Surg. 29:998–1001. https://doi.org/10.1097/SCS.0000000000004396. DOI: 10.1097/SCS.0000000000004396. PMID: 29498976.
Article23. Krishnan B, Parida PK, Gopalakrishnan S, Satyparakash MV. 2013; An unusual cause of epistaxis in a young patient: the supernumerary nasal tooth. Oral Maxillofac Surg. 17:315–7. https://doi.org/10.1007/s10006-013-0393-6. DOI: 10.1007/s10006-013-0393-6. PMID: 23344617.
Article24. Iwai T, Aoki N, Yamashita Y, Omura S, Matsui Y, Maegawa J, et al. 2012; Endoscopic removal of bilateral supernumerary intranasal teeth. J Oral Maxillofac Surg. 70:1030–4. https://doi.org/10.1016/j.joms.2011.10.014. DOI: 10.1016/j.joms.2011.10.014. PMID: 22538022.
Article25. Verma RK, Bakshi J, Panda NK. 2012; Ectopic intranasal tooth: an unusual cause of epistaxis in a child. Ear Nose Throat J. 91:242–4. DOI: 10.1177/014556131209100606. PMID: 22711391.
Article26. Al Dhafeeri HO, Kavarodi A, Al Shaikh K, Bukhari A, Al Hussain O, El Baramawy A. 2014; Recurrent epistaxis caused by an intranasal supernumerary tooth in a young adult. Am J Case Rep. 15:291–3. https://doi.org/10.12659/AJCR.890710. DOI: 10.12659/AJCR.890710. PMID: 25031783. PMCID: PMC4099208.
Article27. Kirmeier R, Truschnegg A, Payer M, Malyk J, Daghighi S, Jakse N. 2009; The supernumerary nasal tooth. Int J Oral Maxillofac Surg. 38:1219–22. https://doi.org/10.1016/j.ijom.2009.06.013. DOI: 10.1016/j.ijom.2009.06.013. PMID: 19596556.
Article28. Lee FP. 2001; Endoscopic extraction of an intranasal tooth: a review of 13 cases. Laryngoscope. 111:1027–31. https://doi.org/10.1097/00005537-200106000-00017. DOI: 10.1097/00005537-200106000-00017. PMID: 11404615.
Article29. Milam SB, Cooper RL. 1983; Extensive bleeding following extractions in a patient undergoing chronic hemodialysis. Oral Surg Oral Med Oral Pathol. 55:14–6. https://doi.org/10.1016/0030-4220(83)90298-0. DOI: 10.1016/0030-4220(83)90298-0. PMID: 6600828.
Article30. Gupta A, Epstein JB, Cabay RJ. 2007; Bleeding disorders of importance in dental care and related patient management. J Can Dent Assoc. 73:77–83. PMID: 17295950.31. Rafique S, Fiske J, Palmer G, Daly B. 2013; Special care dentistry: part 1. Dental management of patients with inherited bleeding disorders. Dent Update. 40:613–6. 619–22. 625–6 passim. https://doi.org/10.12968/denu.2013.40.8.613. DOI: 10.12968/denu.2013.40.8.613. PMID: 24279214.
Article32. Virupakshappa D, Rajashekhara BS, Manjunatha BS, Das N. 2014; Adenomatoid odontogenic tumour in a 20-year-old woman. BMJ Case Rep. 2014:bcr2013010436. https://doi.org/10.1136/bcr-2013-010436. DOI: 10.1136/bcr-2013-010436. PMID: 24810436. PMCID: PMC3992600.
Article33. Wenig BL, Sciubba JJ, Cohen A, Goldstein A, Abramson AL. 1985; An unusual cause of unilateral nasal obstruction: ameloblastoma. Otolaryngol Head Neck Surg. 93:426–32. https://doi.org/10.1177/019459988509300327. DOI: 10.1177/019459988509300327. PMID: 3927244.
Article34. Kühnel TS, Reichert TE. 2015; Trauma of the midface. GMS Curr Top Otorhinolaryngol Head Neck Surg. 14:Doc06. https://doi.org/10.3205/cto000121. DOI: 10.3205/cto000121. PMID: 26770280. PMCID: PMC4702055.
Article35. Dallan I, Tschabitscher M, Castelnuovo P, Bignami M, Muscatello L, Lenzi R, et al. 2009; Management of severely bleeding ethmoidal arteries. J Craniofac Surg. 20:450–4. https://doi.org/10.1097/SCS.0b013e31819b9803. DOI: 10.1097/SCS.0b013e31819b9803. PMID: 19276822.
Article36. Yonezawa H, Yanamoto S, Hoshino T, Yamada S, Fujiwara T, Umeda M. 2013; Management of maxillary alveolar bone fracture and severely intruded maxillary central incisor: report of a case. Dent Traumatol. 29:416–9. https://doi.org/10.1111/j.1600-9657.2011.01111.x. DOI: 10.1111/j.1600-9657.2011.01111.x. PMID: 22233224.
Article37. Pashen D, Stevens M. 2002; Management of epistaxis in general practice. Aust Fam Physician. 31:717–21. PMID: 12189661.38. Kitamura T, Takenaka Y, Takeda K, Oya R, Ashida N, Shimizu K, et al. 2019; Sphenopalatine artery surgery for refractory idiopathic epistaxis: systematic review and meta-analysis. Laryngoscope. 129:1731–6. https://doi.org/10.1002/lary.27767. DOI: 10.1002/lary.27767. PMID: 30613985.
Article39. Shah QA. 2008; Bilateral tri-arterial embolization for the treatment of epistaxis. J Vasc Interv Neurol. 1:102–5. PMID: 22518233. PMCID: PMC3317326.40. Tomljenovic B, Herrmann S, Filippi A, Kühl S. 2016; Life-threatening hemorrhage associated with dental implant surgery: a review of the literature. Clin Oral Implants Res. 27:1079–84. https://doi.org/10.1111/clr.12685. DOI: 10.1111/clr.12685. PMID: 26364684.
Article41. Lazaridis N, Tilaveridis I, Venetis G, Lazaridou M. 2008; Maxillary sinus osteoplasty with vascularized pedicled bone flap. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 106:828–32. https://doi.org/10.1016/j.tripleo.2008.05.030. DOI: 10.1016/j.tripleo.2008.05.030. PMID: 18656389.
Article42. Aukštakalnis R, Simonavičiūtė R, Simuntis R. 2018; Treatment options for odontogenic maxillary sinusitis: a review. Stomatologija. 20:22–6. PMID: 29806655.43. Levin M, Sommer DD. 2019; Endoscopic removal of ectopic sinonasal teeth: a systematic review. J Otolaryngol Head Neck Surg. 48:30. https://doi.org/10.1186/s40463-019-0353-8. DOI: 10.1186/s40463-019-0353-8. PMID: 31277707. PMCID: PMC6612209.
Article44. Peisker A, Raschke GF, Schultze-Mosgau S. 2014; Management of dental extraction in patients with haemophilia A and B: a report of 58 extractions. Med Oral Patol Oral Cir Bucal. 19:e55–60. https://doi.org/10.4317/medoral.19191. DOI: 10.4317/medoral.19191. PMID: 24121912. PMCID: PMC3909433.
Article45. Anderson JA, Brewer A, Creagh D, Hook S, Mainwaring J, McKernan A, et al. 2013; Guidance on the dental management of patients with haemophilia and congenital bleeding disorders. Br Dent J. 215:497–504. https://doi.org/10.1038/sj.bdj.2013.1097. DOI: 10.1038/sj.bdj.2013.1097. PMID: 24264665.
Article46. Dézsi CA, Dézsi BB, Dézsi AD. 2017; Management of dental patients receiving antiplatelet therapy or chronic oral anticoagulation: a review of the latest evidence. Eur J Gen Pract. 23:196–201. Erratum in: Eur J Gen Pract 2017;23:i-ii. https://doi.org/10.1080/13814788.2017.1350645. DOI: 10.1080/13814788.2017.1350645. PMID: 28743214. PMCID: PMC5774272.
Article47. Kwak EJ, Nam S, Park KM, Kim SY, Huh J, Park W. 2019; Bleeding related to dental treatment in patients taking novel oral anticoagulants (NOACs): a retrospective study. Clin Oral Investig. 23:477–84. https://doi.org/10.1007/s00784-018-2458-2. DOI: 10.1007/s00784-018-2458-2. PMID: 29696419.
Article48. Ho JPK, Bari N, Riffat F. 2020; Management of epistaxis in patients on novel oral anticoagulation therapy. J Laryngol Otol. 134:316–22. https://doi.org/10.1017/S0022215120000754. DOI: 10.1017/S0022215120000754. PMID: 32281535.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blind Intubation Using Fiberoptic Bronchoscope in Epistaxis
- The Clinical Study for Epistaxis and Tube Insertion Failure Incidence on the Choice of Nostril during Nasotracheal Intubation
- Education of Oral and Maxillofacial Radiology in South Korea
- Diagnosis and treatment of obstructive atelectasis after general anesthesia in a patient with abscess in the maxillofacial area: A case report
- Job Analysis by Department in Clinical Practice for Realization of Legal Scope of Dental Hygienists: Focusing on Conservation, Pediatric Dentistry, Prosthodontics, Oral and Maxillofacial Surgery, and Implant Departments