Arch Hand Microsurg.
2022 Mar;27(1):79-82. 10.12790/ahm.21.0107.
Direction change in a distal bypass graft due to increased collateral perfusion after the free flap transfer: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Sapporo City General Hospital, Sapporo, Japan
- 2Department of Cardiovascular Medicine, Sapporo City General Hospital, Sapporo, Japan
- KMID: 2526653
- DOI: http://doi.org/10.12790/ahm.21.0107
Abstract
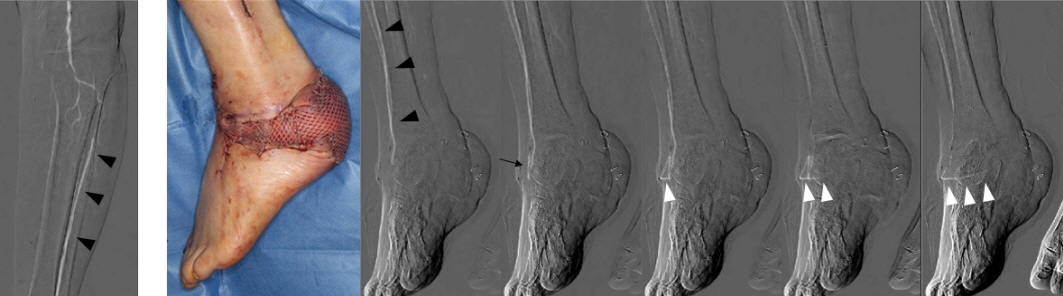
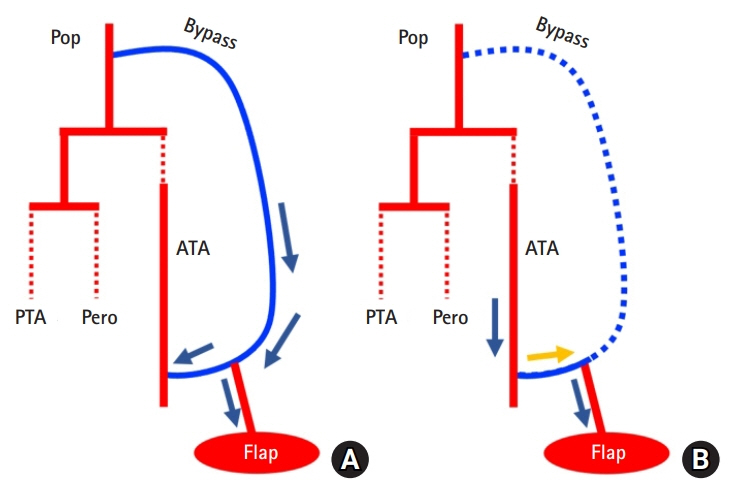
- Distal bypass combined with a free flap is a frequent surgical option for ischemic ulcers of the lower extremities. Here, we describe a patient in whom there was a change in the direction of blood flow in a distal bypass graft. A 68-year-old male patient with an ischemic ulcer on his left heel was referred to our facility by a local dermatology clinic. Surgical revascularization was performed between the popliteal artery and the dorsalis pedis artery using an ipsilateral great saphenous vein as the graft vessel. The wound site did not heal postoperatively, so it was covered using a free latissimus dorsi muscle flap. At the same time, the thoracodorsal artery was anastomosed to the bypass graft in an end-to-side manner to serve as a nutrient vessel. Initially, blood flow into the thoracodorsal artery from the bypass graft was via the popliteal artery. However, after occlusion of the proximal anastomotic site of the bypass graft, blood flow into the thoracodorsal artery from the bypass graft was via the dorsalis pedis artery, which was the distal anastomotic site. The change in direction of blood flow might have been the result of an increase in blood flow in the collateral vessels in the ischemic lower leg, which eventually overwhelmed the blood flow in the bypass graft.
Keyword
Figure
Reference
-
References
1. Mätzke S, Tukiainen EJ, Lepäntalo MJ. Survival of a microvascular muscle flap despite the late occlusion of the inflow artery in a neuroischaemic diabetic foot. Scand J Plast Reconstr Surg Hand Surg. 1997; 31:71–5.
Article2. Tanaka K, Igari K, Kishino M, et al. The possibility of free tissue transfer as a nutrient flap for critical ischemic foot: a case report. Microsurgery. 2017; 37:694–8.
Article3. Meyer A, Goller K, Horch RE, et al. Results of combined vascular reconstruction and free flap transfer for limb salvage in patients with critical limb ischemia. J Vasc Surg. 2015; 61:1239–48.
Article4. Mimoun M, Hilligot P, Baux S. The nutrient flap: a new concept of the role of the flap and application to the salvage of arteriosclerotic lower limbs. Plast Reconstr Surg. 1989; 84:458–67.5. Levin SR, Arinze N, Siracuse JJ. Lower extremity critical limb ischemia: a review of clinical features and management. Trends Cardiovasc Med. 2020; 30:125–30.
Article6. Slovut DP, Sullivan TM. Critical limb ischemia: medical and surgical management. Vasc Med. 2008; 13:281–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Application of Tensor Fascia Lata Myocutaneous Free Flap: Two Cases Report
- Neurovascular Free Flap Transfer by Microsurgery
- Treatment of Large Heel Defect in Diabetic Patients; Use of Artificial Bypass Graft and Antero-lateral Thigh Perforator Flap: A Case Report
- Salvage of Esophageal Reconstruction with Colon Free Flap
- Sural Vessels as Recipient Vessels for Free Flap Transfer to the Single Vessel Leg