Healthc Inform Res.
2022 Jan;28(1):95-101. 10.4258/hir.2022.28.1.95.
Reliability of Measuring Leg Segments and Joint Angles Using Smartphones during Aquatic Exercise
- Affiliations
-
- 1Department of Physical Therapy, U1 University, Yeongdong-gun, Chungbuk, Korea
- 2Department of Physical Therapy, Daejeon Health Institute of Technology, Daejeon, Korea
- KMID: 2526498
- DOI: http://doi.org/10.4258/hir.2022.28.1.95
Abstract
Objectives
Aquatic therapy is a significant intervention method for both patients and healthy individuals. However, in clinical practice, quantitative measurements are rarely applied in aquatic therapy due to the disadvantages of submerging expensive instruments in water. In this study, we used readily available smartphones and armbands to measure leg segments and joint angles during aquatic gait and evaluated the reliability of these measurements.
Methods
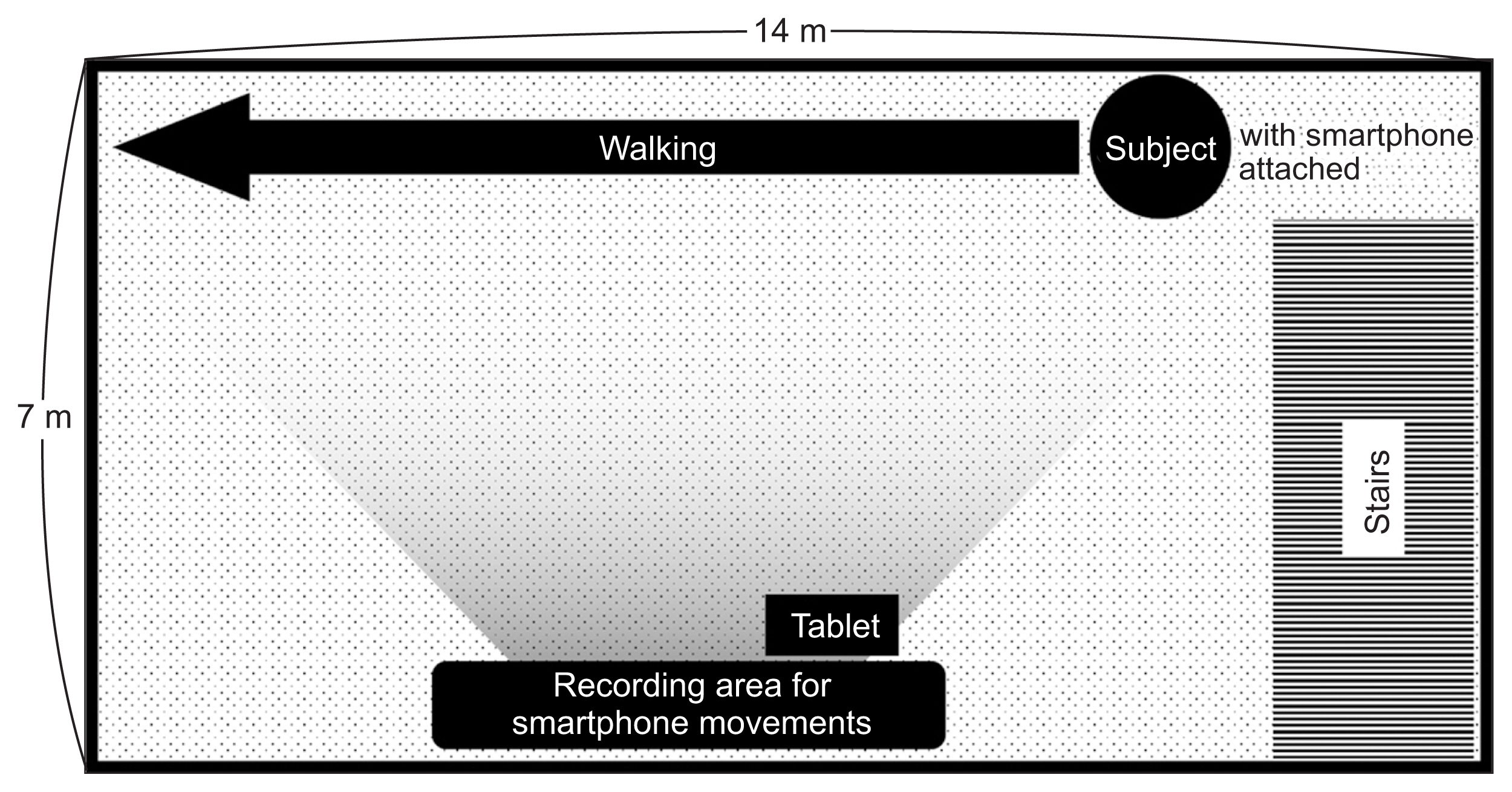
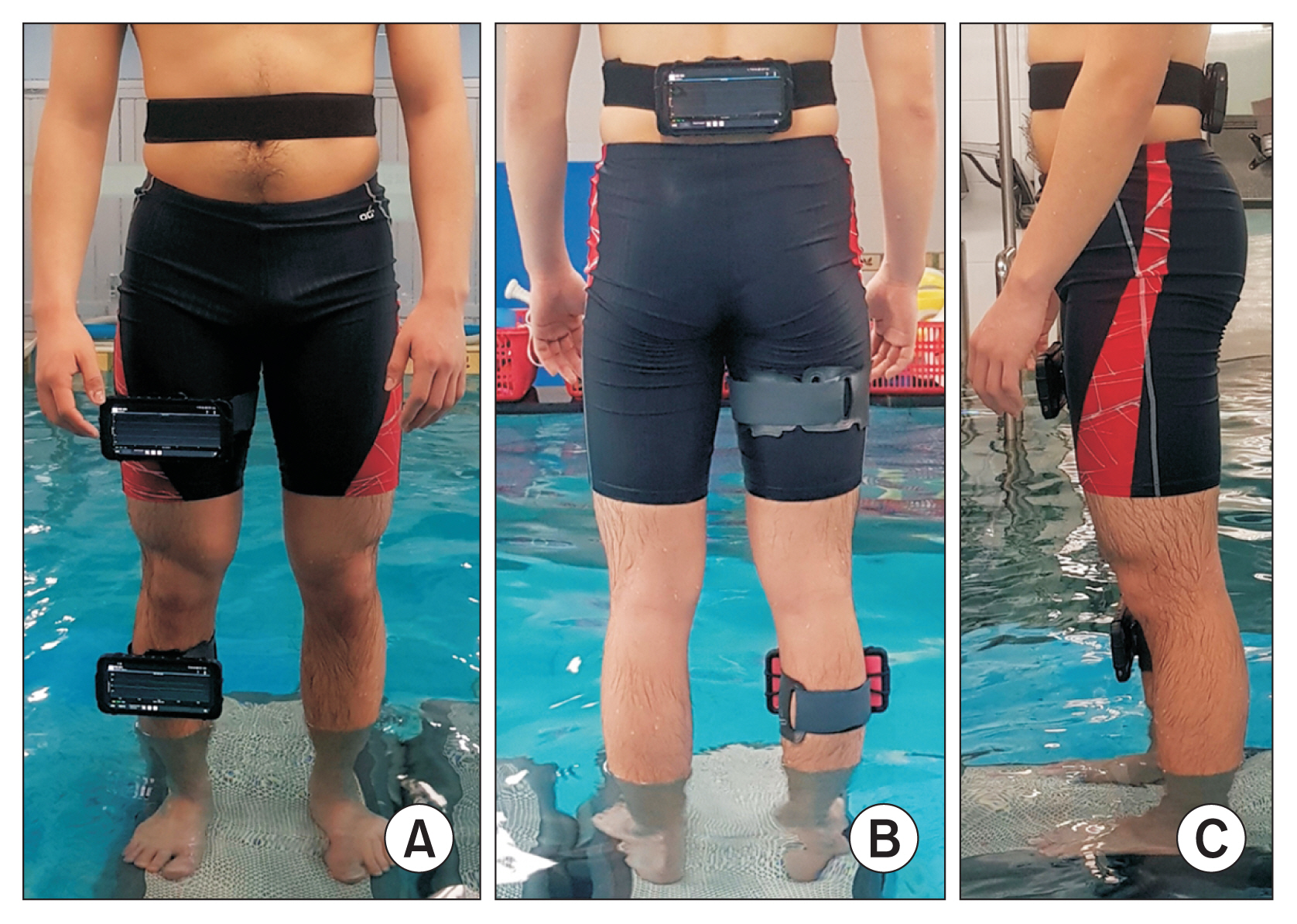
Waterproof smartphones were strapped to the trunk, thighs, and shanks of 19 healthy young adults using armbands. The angles of the trunk, thigh, and shank segments were measured during aquatic gait. The measurements were repeated 1 day later. The data were analyzed to obtain the angles of the hip and knee joints.
Results
Measurement repeatability, calculated using the intraclass correlation coefficient (ICC), was the highest for the shank segment range of motion (ROM) (first 46.79° ± 5.50°, second 50.12° ± 9.98°, ICC = 0.78). There was high agreement in trunk segment ROM (first 6.36° ± 1.42°, second 4.29° ± 1.83°, ICC = 0.73), thigh segment ROM (first 33.49° ± 5.18°, second 37.31° ± 8.70°, ICC = 0.62), and knee joint ROM (first 52.43° ± 11.26°, second 62.19° ± 16.65°, ICC = 0.68) and fair agreement in hip joint ROM (first 34.60°±4.71°, second 37.80° ± 7.84°, ICC = 0.59).
Conclusions
Smartphones can be used to reliably measure leg segments and joint angles during aquatic gait, providing a simpler method for obtaining these measurements and enabling the wider use of aquatic motion analysis in clinical practice and research.
Keyword
Figure
Reference
-
References
1. Mangia AL, Cortesi M, Fantozzi S, Giovanardi A, Borra D, Gatta G. The use of IMMUs in a water environment: instrument validation and application of 3D multi-body kinematic analysis in medicine and sport. Sensors (Basel). 2017; 17(4):927.
Article2. Fantozzi S, Giovanardi A, Borra D, Gatta G. Gait kinematic analysis in water using wearable inertial magnetic sensors. PLoS One. 2015; 10(9):e0138105.
Article3. Mercer JA, Applequist BC, Masumoto K. Muscle activity during running with different body-weight-support mechanisms: aquatic environment versus body-weight-support treadmill. J Sport Rehabil. 2014; 23(4):300–6.
Article4. Jung T, Kim Y, Lim H, Vrongistinos K. The influence of water depth on kinematic and spatiotemporal gait parameters during aquatic treadmill walking. Sports Biomech. 2019; 18(3):297–307.
Article5. Dolbow DR, Farley RS, Kim JK, Caputo JL. Oxygen consumption, heart rate, rating of perceived exertion, and systolic blood pressure with water treadmill walking. J Aging Phys Act. 2008; 16(1):14–23.
Article6. Nakazawa K, Yano H, Miyashita M. Ground reaction forces during walking in water. Mutoh Y, Miyashita M, Richardson AB, editors. Medicine and science in aquatic sports. Basel, Switzerland: S. Karger AG;1994. p. 28–34.
Article7. Murray JM, Hunter DL, Kelsey DD, Murray TD. Determination of the physiological effects of unloaded treadmill exercise. Cardiopulm Phys Ther J. 1993; 4(2):13–6.
Article8. Skelton DA, Dinan SM. Exercise for falls management: rationale for an exercise programme aimed at reducing postural instability. Physiother Theory Pract. 1999; 15(2):105–20.
Article9. Alikhajeh Y, Hosseini SR, Moghaddam A. Effects of hydrotherapy in static and dynamic balance among elderly men. Procedia Soc Behav Sci. 2012; 46:2220–4.
Article10. Silsupadol P, Teja K, Lugade V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: body, bag, belt, hand, and pocket. Gait Posture. 2017; 58:516–22.
Article11. Masumoto K, Hamada A, Tomonaga HO, Kodama K, Amamoto Y, Nishizaki Y, et al. Physiological and perceptual responses to backward and forward treadmill walking in water. Gait Posture. 2009; 29(2):199–203.
Article12. Ceseracciu E, Sawacha Z, Fantozzi S, Cortesi M, Gatta G, Corazza S, et al. Markerless analysis of front crawl swimming. J Biomech. 2011; 44(12):2236–42.
Article13. Cortesi M, Fantozzi S, Gatta G. Effects of distance specialization on the backstroke swimming kinematics. J Sports Sci Med. 2012; 11(3):526–32.14. McCabe CB, Sanders RH. Kinematic differences between front crawl sprint and distance swimmers at a distance pace. J Sports Sci. 2012; 30(6):601–8.
Article15. Tamburella F, Scivoletto G, Cosentino E, Molinari M. Walking in water and on land after an incomplete spinal cord injury. Am J Phys Med Rehabil. 2013; 92(10 Suppl 2):e4–15.
Article16. Silvatti AP, Dias FA, Cerveri P, Barros RM. Comparison of different camera calibration approaches for underwater applications. J Biomech. 2012; 45(6):1112–6.
Article17. Silvatti AP, Cerveri P, Telles T, Dias FA, Baroni G, Barros RM. Quantitative underwater 3D motion analysis using submerged video cameras: accuracy analysis and trajectory reconstruction. Comput Methods Biomech Biomed Engin. 2013; 16(11):1240–8.
Article18. Magalhaes FA, Sawacha Z, Di Michele R, Cortesi M, Gatta G, Fantozzi S. Effectiveness of an automatic tracking software in underwater motion analysis. J Sports Sci Med. 2013; 12(4):660–7.19. Mooney R, Corley G, Godfrey A, Osborough C, Newell J, Quinlan LR, et al. Analysis of swimming performance: perceptions and practices of US-based swimming coaches. J Sports Sci. 2016; 34(11):997–1005.
Article20. Masumoto K, Mercer JA. Biomechanics of human locomotion in water: an electomyographic analysis. Exerc Sport Sci Rev. 2008; 36(3):160–9.21. Buechi R, Faes L, Bachmann LM, Thiel MA, Bodmer NS, Schmid MK, et al. Evidence assessing the diagnostic performance of medical smartphone apps: a systematic review and exploratory meta-analysis. BMJ Open. 2017; 7(12):e018280.
Article22. Longoni L, Brunati R, Sale P, Casale R, Ronconi G, Ferriero G. Smartphone applications validated for joint angle measurement: a systematic review. Int J Rehabil Res. 2019; 42(1):11–9.
Article23. Polechonski J, Nawrocka A, Wodarski P, Tomik R. Applicability of smartphone for dynamic postural stability evaluation. Biomed Res Int. 2019; 2019:9753898.24. Lee D, Han S. Study on the reliability of smartphone-based measurements of leg segment and joint angles during gait. J Korean Soc Precis Eng. 2019; 36(3):293–300.
Article25. Furrer M, Bichsel L, Niederer M, Baur H, Schmid S. Validation of a smartphone-based measurement tool for the quantification of level walking. Gait Posture. 2015; 42(3):289–94.
Article26. Samsung Galaxy S [Internet]. Seoul, Korea: Samsung;c2021. [cited at 2022 Jan 4]. Available from: https://www.samsung.com/sec/smartphones/galaxy-s8/ .27. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994; 6(4):284–90.
Article28. Lugade V, Fortune E, Morrow M, Kaufman K. Validity of using tri-axial accelerometers to measure human movement. Part I: posture and movement detection. Med Eng Phys. 2014; 36(2):169–76.29. Fortune E, Lugade V, Morrow M, Kaufman K. Validity of using tri-axial accelerometers to measure human movement. Part II: step counts at a wide range of gait velocities. Med Eng Phys. 2014; 36(6):659–69.30. Barela AM, Stolf SF, Duarte M. Biomechanical characteristics of adults walking in shallow water and on land. J Electromyogr Kinesiol. 2006; 16(3):250–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of Joint Position Sense of Dorsi-Plantar Flexion of Ankle Measurements Using a Smartphone
- An Effects of Aquatic Exercise on in Home Stroke Patients
- Comparison of Effects among Tai-Chi Exercise, Aquatic Exercise, and a Self-help Program for Patients with Knee Osteoarthritis
- Changes in Activation of Abdominal Muscles at Selected Angles During Trunk Exercise by Using Ultrasonography
- The Effect of Aquatic Exercise Program on Body Weight, Muscle Strength and Flexibility in Healthy Middle-aged Women