J Korean Diabetes.
2021 Dec;22(4):250-258. 10.4093/jkd.2021.22.4.250.
2021 Clinical Practice Guidelines for Diabetes: Pharmacotherapy and the Korean Diabetes Association Support System
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2526208
- DOI: http://doi.org/10.4093/jkd.2021.22.4.250
Abstract
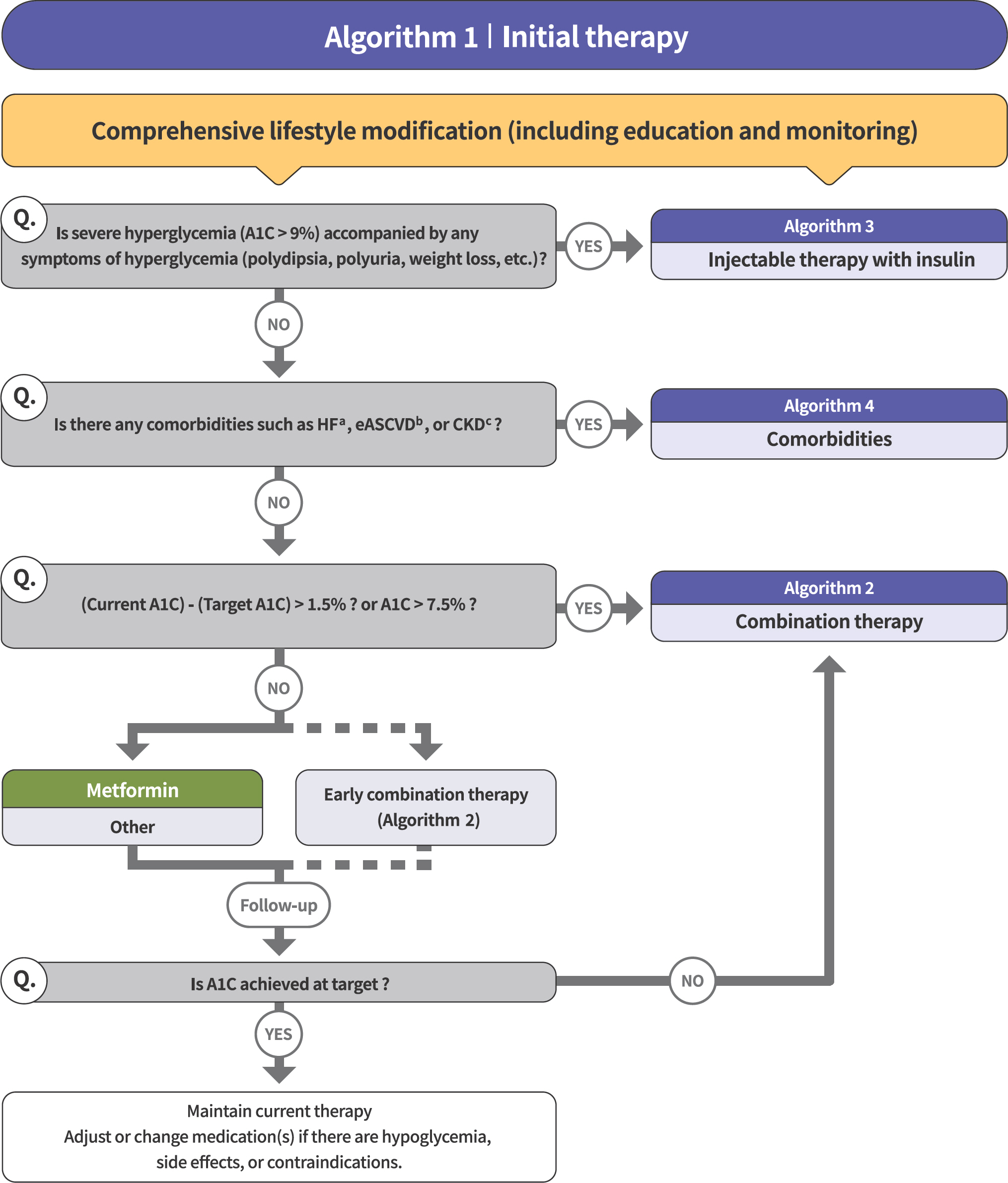
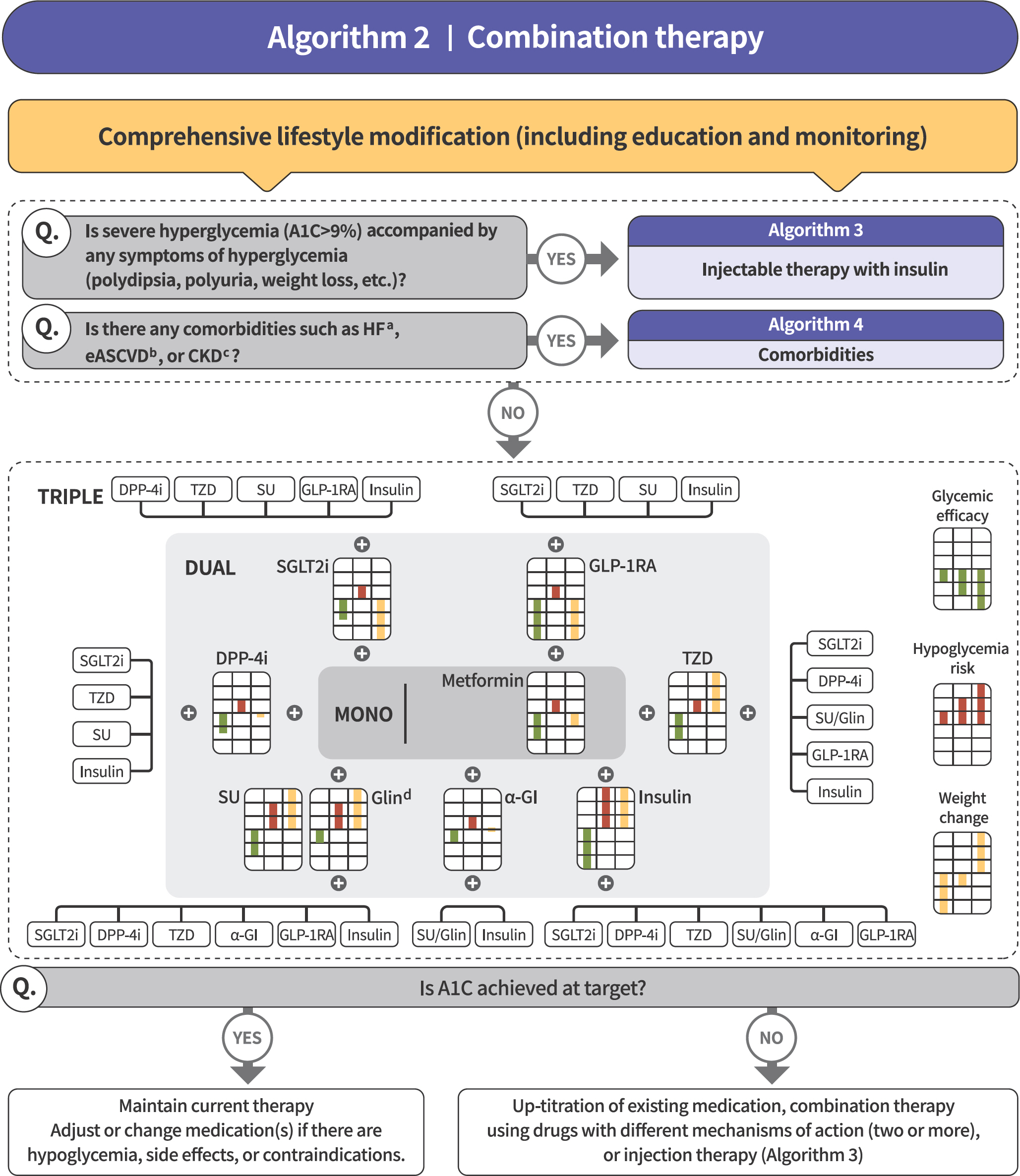
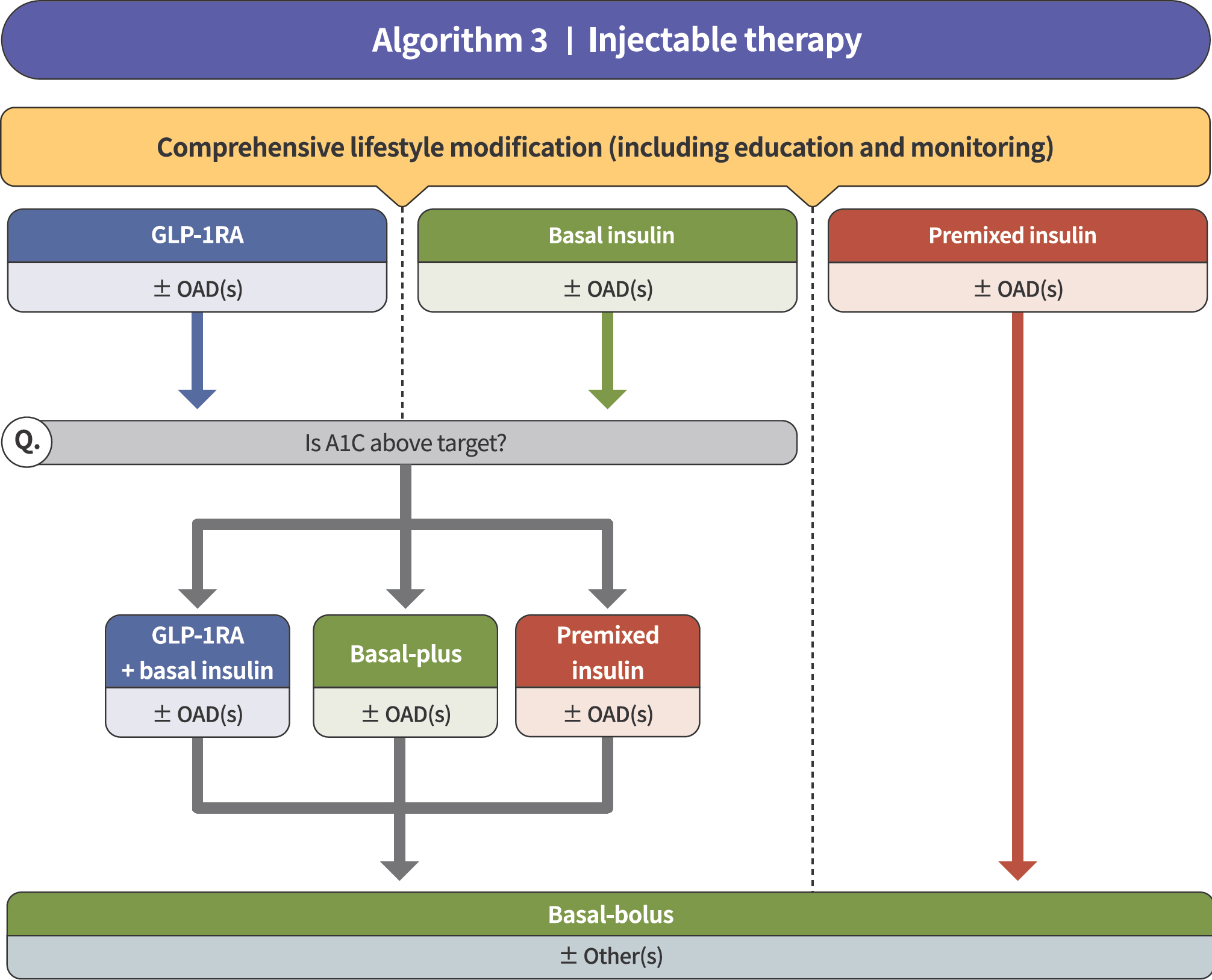
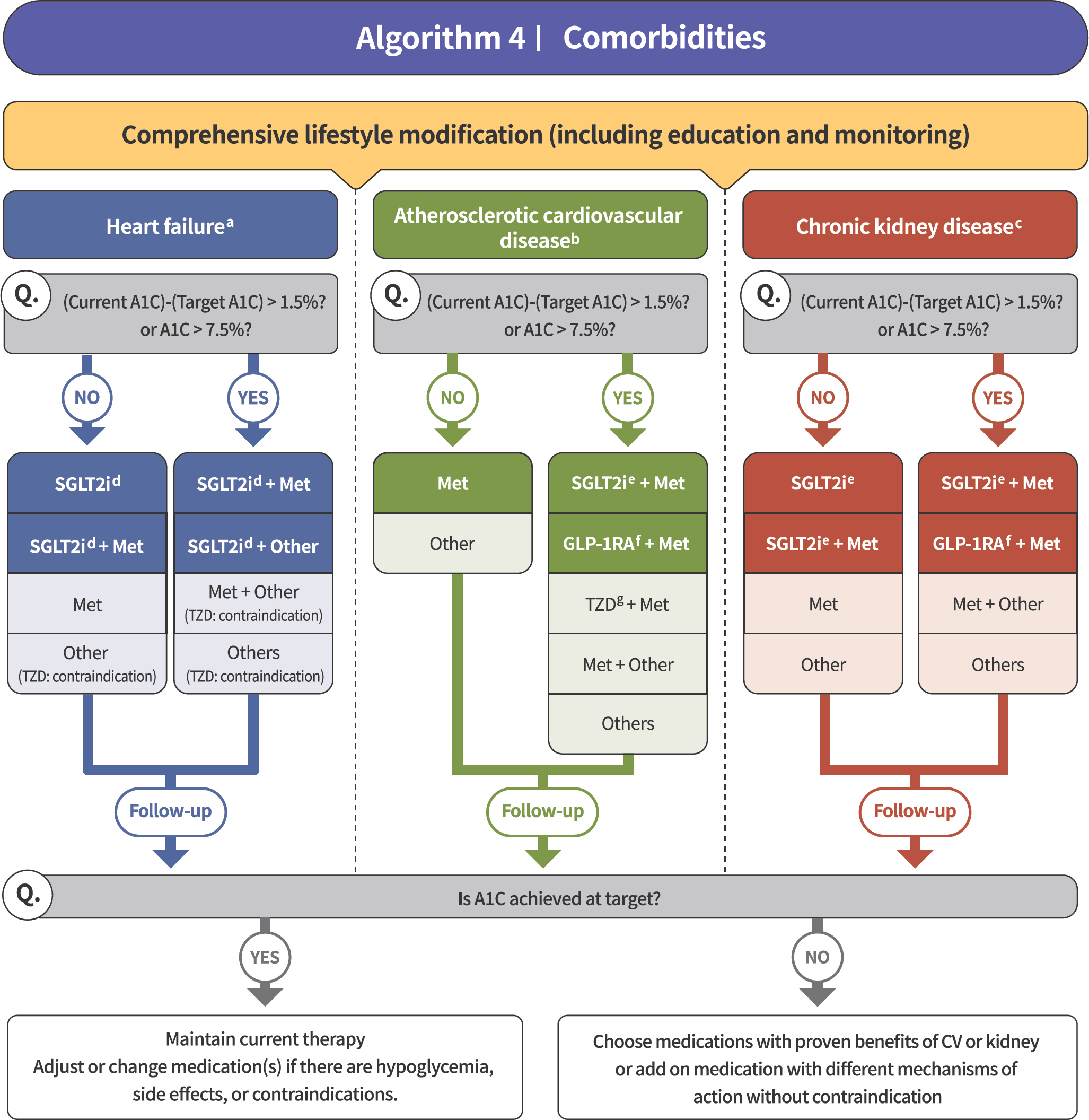
- The most important change introduced in the pharmacotherapy session for the 2021 Clinical Practice Guidelines for Diabetes is the recommendation of two different strategies according to the patient’s condition. One approach is to optimize the blood glucose levels, while the other approach is to reduce adverse cardiovascular events or mortality, especially in patients with comorbidities (e.g., heart failure, atherosclerotic cardiovascular disease, or chronic kidney disease). We suggest four algorithms that take into account the patient’s condition (algorithms 1 to 4). The Korean Diabetes Association (KDA) developed a web-based clinical decision support system, known as the KDA support system (KDASS), which helps with the diagnosis of diabetes or gestational diabetes and whether to use glucose-lowering agents according to the patient’s condition.
Keyword
Figure
Reference
-
1.Hur KY., Moon MK., Park JS., Kim SK., Lee SH., Yun JS, et al. 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association. Diabetes Metab J. 2021. 45:461–81.
Article2.Stratton IM., Adler AI., Neil HA., Matthews DR., Manley SE., Cull CA, et al. Association of glycaemia with macro-vascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000. 321:405–12.
Article3.Kramer CK., Zinman B., Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: a system-atic review and meta-analysis. Lancet Diabetes Endocrinol. 2013. 1:28–34.
Article4.Tsapas A., Avgerinos I., Karagiannis T., Malandris K., Manol-opoulos A., Andreadis P, et al. Comparative effectiveness of glucose-lowering drugs for type 2 diabetes: a system-atic review and network meta-analysis. Ann Intern Med. 2020. 173:278–86.5.Moon MK. 2021 clinical practice guidelines for diabetes: management of cardiovascular risk. J Korean Diabetes. 2021. 22:259–67.
Article6.Kim NH. 2021 Korean Diabetes Association clinical practice guidelines for diabetes: diabetic kidney disease. J Korean Diabetes. 2021. 22:268–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
- 2021 Korean Diabetes Association Clinical Practice Guidelines for Diabetes: Diabetic Kidney Disease
- 2023 Clinical Practice Guidelines for Diabetes
- 2023 Clinical Practice Guidelines for Diabetes: Recommendations for Pharmacological Treatment of Type 2 Diabetes
- 2021 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk