Lab Med Online.
2021 Apr;11(2):81-87. 10.47429/lmo.2021.11.2.81.
Utilization of C-Reactive Protein Test as a Predictor of Lung Injury in Patients with Coronavirus Disease 2019
- Affiliations
-
- 1Department of Laboratory Medicine, Daegu Catholic University School of Medicine, Daegu Catholic University Medical Center,
- 2Department of Radiology, Daegu Catholic University School of Medicine, Daegu, Korea
- 3Division of Pulmonology, Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- 5Department of Medical Statistics, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2525786
- DOI: http://doi.org/10.47429/lmo.2021.11.2.81
Abstract
- Background
C-reactive protein (CRP) test can be used at coronavirus disease 2019 (COVID-19) screening clinics as a point of care test. The aim of this study was to determine whether CRP test can be used as an indicator of lung injury.
Methods
In all, 98 patients with COVID-19 were enrolled for this study. We collected medical records and laboratory results of the patients. Chest radiographic findings were classified into five groups. We analyzed the correlation between laboratory tests and the grade of lung injury.
Results
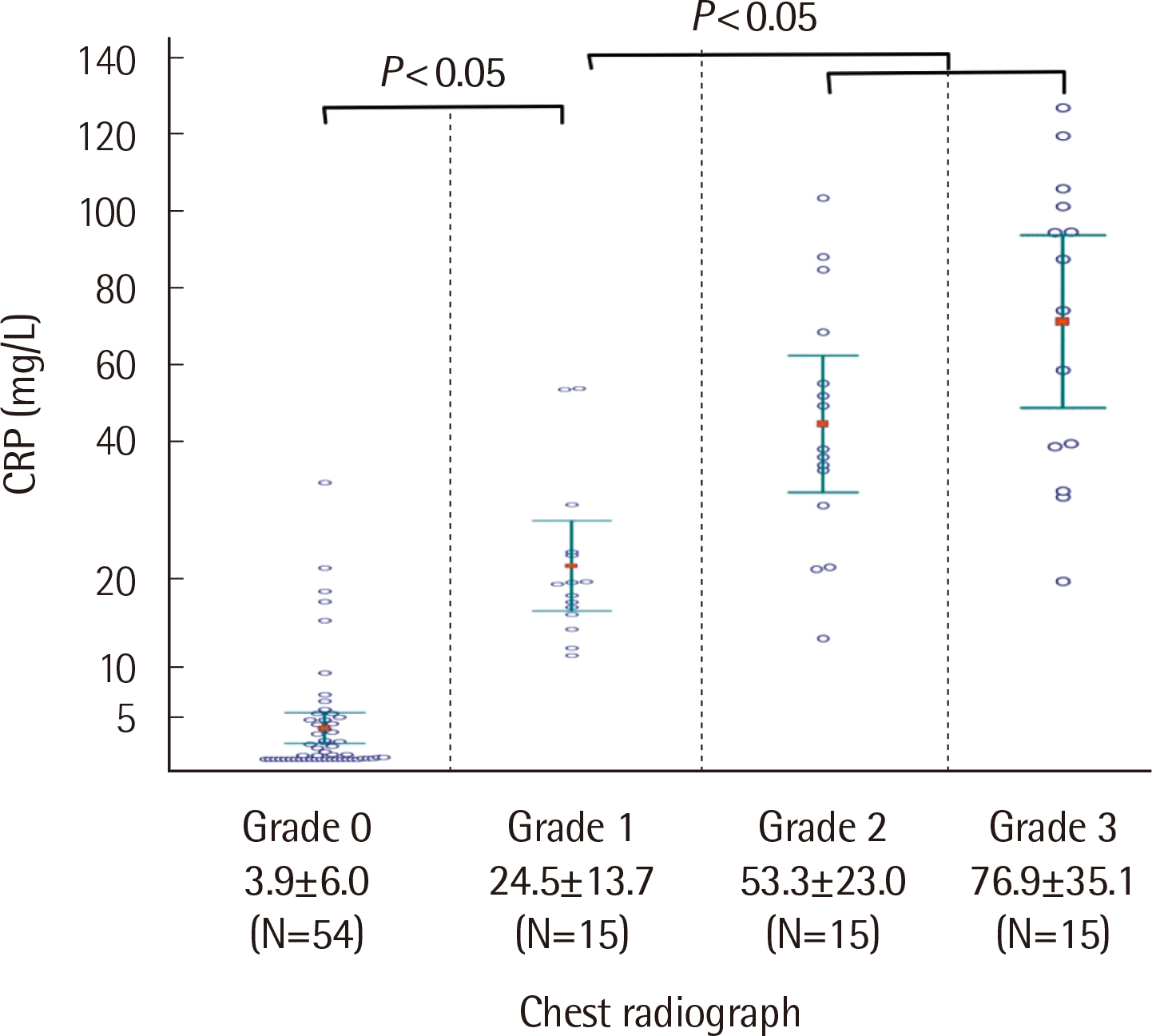
In patients with COVID-19, increased CRP and erythrocyte sedimentation rate (ESR), and lymphocytopenia were noted. CRP , ESR, and segmented neutrophils were found to be positively correlated while albumin and lymphocyte were negatively correlated with lung injury grade. CRP levels showed the highest correlation coefficient of 0.858. Based on the chest radiographs, the sensitivity and specificity of CRP was 100% and 77.8%, respectively. Within the reference range of CRP , abnormal chest radiograph was not recognized. In addition, initial and subsequent increase in CRP levels in patients with unremarkable chest radiograph could be associated with aggravated lung injury.
Conclusions
CRP test showed a sensitivity of 100% in detection of lung injury, and the level was proportional to the extent of lung lesions.Therefore, CRP test will be useful as a predictor of lung injury in patients with COVID-19.
Figure
Reference
-
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. 2020; Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 395:497–506. DOI: 10.1016/S0140-6736(20)30183-5. PMID: 31986264. PMCID: PMC7159299.
Article2. Rothan HA, Byrareddy SN. 2020; The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 109:102433. DOI: 10.1016/j.jaut.2020.102433. PMID: 32113704. PMCID: PMC7127067.
Article3. Matheeussen V, Van Hoof V, Loens K, Lammens C, Vanderstraeten A, Coenen S, et al. 2018; Analytical performance of a platform for point-of-care CRP testing in adults consulting for lower respiratory tract infection in primary care. Eur J Clin Microbiol Infect Dis. 37:1319–23. DOI: 10.1007/s10096-018-3253-3. PMID: 29744764.
Article4. Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y, et al. 2020; C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 92:856–62. DOI: 10.1002/jmv.25871. PMID: 32281668. PMCID: PMC7262341.
Article5. Chen W, Zheng KI, Liu S, Yan Z, Xu C, Qiao Z. 2020; Plasma CRP level is positively associated with the severity of COVID-19. Ann Clin Microbiol Antimicrob. 19:18. DOI: 10.1186/s12941-020-00362-2. PMID: 32414383. PMCID: PMC7227180.
Article6. Bhargava A, Fukushima EA, Levine M, Zhao W, Tanveer F, Szpunar SM, et al. 2020; Predictors for severe COVID-19 infection. Clin Infect Dis. 71:1962–8. DOI: 10.1093/cid/ciaa674. PMID: 32472676. PMCID: PMC7314166.
Article7. Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, et al. 2020; The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. 10:2188–92. DOI: 10.1002/jmv.26031. PMID: 32436996. PMCID: PMC7280691.
Article8. Wang L. 2020; C-reactive protein levels in the early stage of COVID-19. Med Mal Infect. 50:332–4. DOI: 10.1016/j.medmal.2020.03.007. PMID: 32243911. PMCID: PMC7146693.
Article9. Zeng F, Huang Y, Guo Y, Yin M, Chen X, Xiao L, et al. 2020; Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis. 96:467–74. DOI: 10.1016/j.ijid.2020.05.055. PMID: 32425643. PMCID: PMC7233226.
Article10. Zhang ZL, Hou YL, Li DT, Li FZ. 2020; Laboratory findings of COVID-19: a systematic review and meta-analysis. Scand J Clin Lab Invest. 80:441–7. DOI: 10.1080/00365513.2020.1768587. PMID: 32449374. PMCID: PMC7256350.
Article11. Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. 2020; Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 63:364–74. DOI: 10.1007/s11427-020-1643-8. PMID: 32048163. PMCID: PMC7088566.
Article12. Litao MK, Kamat D. 2014; Erythrocyte sedimentation rate and C-reactive protein: how best to use them in clinical practice. Pediatr Ann. 43:417–20. DOI: 10.3928/00904481-20140924-10. PMID: 25290132.
Article13. Sproston NR, Ashworth JJ. 2018; Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 9:754. DOI: 10.3389/fimmu.2018.00754. PMID: 29706967. PMCID: PMC5908901.
Article14. Korppi M, Kröger L. 1993; C-reactive protein in viral and bacterial respiratory infection in children. Scand J Infect Dis. 25:207–13. DOI: 10.3109/00365549309008486. PMID: 8511515.
Article15. Zhao Y, Zhao Z, Wang Y, Zhou Y, Ma Y, Zuo W. 2020; Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am J Respir Crit Care Med. 202:756–9. DOI: 10.1164/rccm.202001-0179LE. PMID: 32663409. PMCID: PMC7462411.
Article16. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. 2020; Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 8:420–2. DOI: 10.1016/S2213-2600(20)30076-X. PMID: 32085846. PMCID: PMC7164771.
Article17. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. 2020; Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 34:101623. DOI: 10.1016/j.tmaid.2020.101623. PMID: 32179124. PMCID: PMC7102608.
Article18. Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. 2020; Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 295:210–7. DOI: 10.1148/radiol.2020200274. PMID: 32027573. PMCID: PMC7233366.
Article19. Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. 2020; COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 92:577–83. DOI: 10.1002/jmv.25757. PMID: 32162702. PMCID: PMC7228329.
Article20. Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, et al. 2020; Characteristics of COVID-19 infection in Beijing. J Infect. 80:401–6. DOI: 10.1016/j.jinf.2020.02.018. PMID: 32112886. PMCID: PMC7102527.
Article21. Zheng HY, Zhang M, Yang CX, Zhang N, Wang XC, Yang XP, et al. 2020; Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol Immunol. 17:541–3. DOI: 10.1038/s41423-020-0401-3. PMID: 32203186. PMCID: PMC7091621.
Article22. Zheng M, Gao Y, Wang G, Song G, Liu S, Sun D, et al. 2020; Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 17:533–5. DOI: 10.1038/s41423-020-0402-2. PMID: 32203188. PMCID: PMC7091858.
Article23. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. 2020; Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 395:507–13. DOI: 10.1016/S0140-6736(20)30211-7. PMID: 32007143. PMCID: PMC7135076.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evidence of Lung Function for Stratification of Cardiovascular Disease Risk
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Changes in Health Care Utilization during the COVID-19 Pandemic
- Acute kidney injury and mortality in coronavirus disease 2019: results from a cohort study of 1,280 patients
- Effect of Neutrophil Elastase inhibitor, ICI 200,355, on Interleukin-1 Induced acute lung injury in rats