J Korean Med Sci.
2022 Feb;37(5):e36. 10.3346/jkms.2022.37.e36.
Predicting Postoperative Complications and Long-Term Survival After Lung Cancer Surgery Using Eurolung Risk Score
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea
- KMID: 2525488
- DOI: http://doi.org/10.3346/jkms.2022.37.e36
Abstract
- Background
This study aimed to assess the clinical relevance of the parsimonious Eurolung risk scoring system for predicting postoperative morbidity, mortality, and long-term survival in Korean patients with surgically resected non-small cell lung cancer.
Methods
This retrospective analysis used the data of patients who underwent anatomical resection for non-small cell lung cancer between 2004 and 2018 at a single institution. The parsimonious aggregate Eurolung score was calculated for each patient. The Cox regression model was used to determine the ability of the Eurolung scoring system for predicting longterm outcomes.
Results
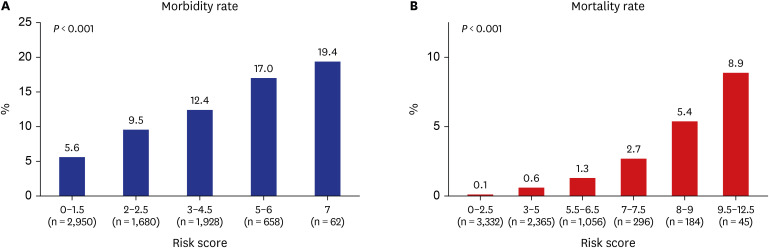
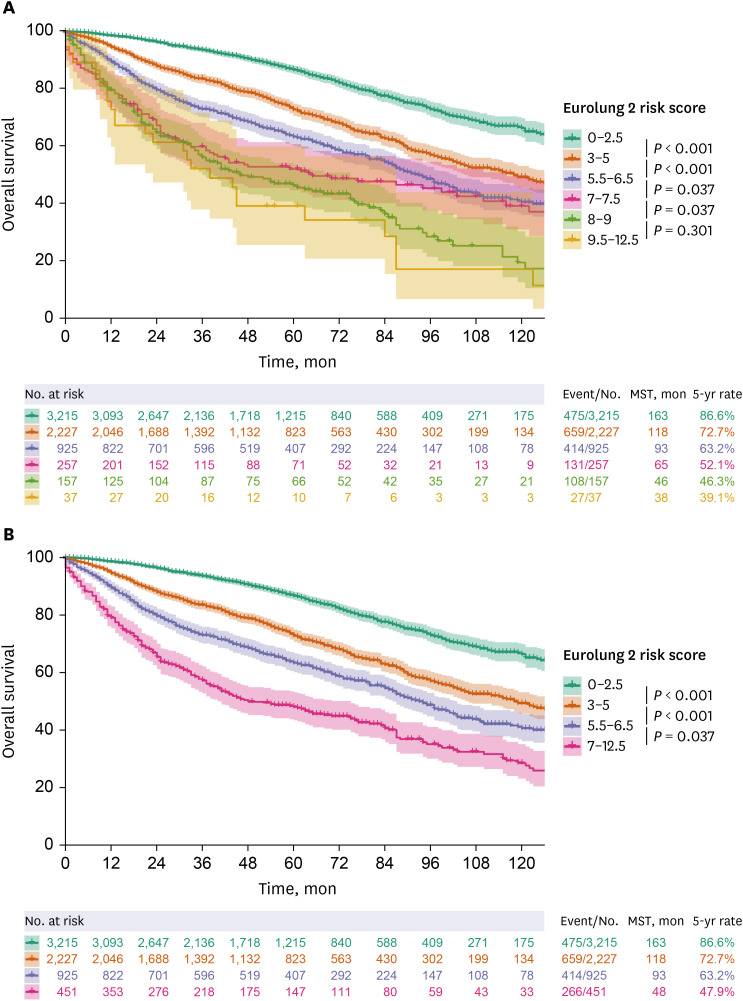
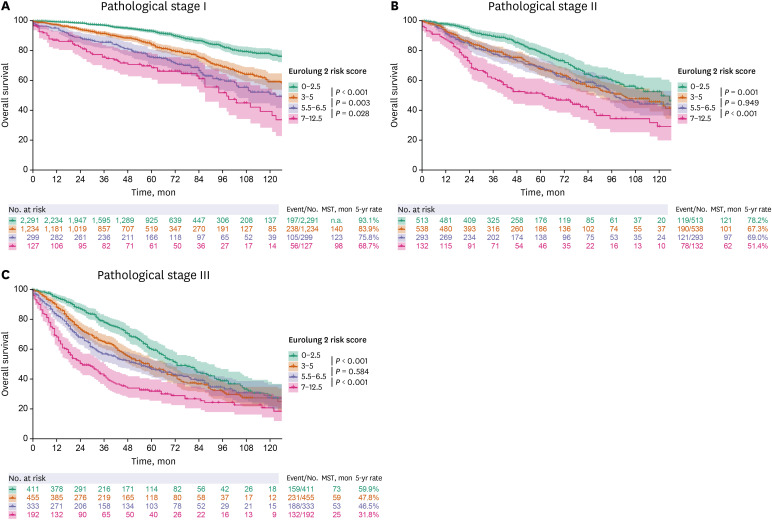
Of the 7,278 patients in the study, cardiopulmonary complications and mortality occurred in 687 (9.4%) and 53 (0.7%) patients, respectively. The rate of cardiopulmonary complications and mortality gradually increased with the increase in the Eurolung risk scores (all P < 0.001). When risk scores were grouped into four categories, the Eurolung scoring system showed a stepwise deterioration of overall survival with the increase in risk scores, and this association was statistically significant (P < 0.001). Multivariate Cox analysis showed that the Eurolung scoring system, classified into four categories, was a significant prognostic factor of overall survival even after adjusting for covariates such as tumor histology and pathological stage (P < 0.001).
Conclusion
Stratification based on the parsimonious Eurolung scoring system showed good discriminatory ability for predicting postoperative morbidity, mortality, and long-term survival in South Korean patients with surgically resected non-small cell lung cancer. This might help clinicians to provide a detailed prognosis and decide the appropriate treatment option for high-risk patients with non-small cell lung cancer.
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018; 68(1):7–30. PMID: 29313949.
Article2. Yun JK, Lee HP, Lee GD, Kim HR, Kim YH, Kim DK, et al. Recent trends in demographics, surgery, and prognosis of patients with surgically resected lung cancer in a single institution from Korea. J Korean Med Sci. 2019; 34(45):e291. PMID: 31760712.
Article3. Brunelli A, Salati M, Rocco G, Varela G, Van Raemdonck D, Decaluwe H, et al. European risk models for morbidity (EuroLung1) and mortality (EuroLung2) to predict outcome following anatomic lung resections: an analysis from the European Society of Thoracic Surgeons database. Eur J Cardiothorac Surg. 2017; 51(3):490–497. PMID: 27744321.
Article4. Brunelli A, Cicconi S, Decaluwe H, Szanto Z, Falcoz PE. Parsimonious Eurolung risk models to predict cardiopulmonary morbidity and mortality following anatomic lung resections: an updated analysis from the European Society of Thoracic Surgeons database. Eur J Cardiothorac Surg. 2020; 57(3):455–461. PMID: 31605105.
Article5. Brunelli A, Chaudhuri N, Kefaloyannis M, Milton R, Pompili C, Tcherveniakov P, et al. Eurolung risk score is associated with long-term survival after curative resection for lung cancer. J Thorac Cardiovasc Surg. 2021; 161(3):776–786. PMID: 32948299.
Article6. Detterbeck FC, Boffa DJ, Kim AW, Tanoue LT. The eighth edition lung cancer stage classification. Chest. 2017; 151(1):193–203. PMID: 27780786.
Article7. Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. WHO Panel. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015; 10(9):1243–1260. PMID: 26291008.8. Cukic V. Preoperative prediction of lung function in pneumonectomy by spirometry and lung perfusion scintigraphy. Acta Inform Med. 2012; 20(4):221–225. PMID: 23378687.
Article9. Fernandez FG, Falcoz PE, Kozower BD, Salati M, Wright CD, Brunelli A. The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons general thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg. 2015; 99(1):368–376. PMID: 25555970.
Article10. Zhang Z. Estimating the optimal cutoff point for logistic regression. Updated 2018. Accessed January 1, 2022. https://scholarworks.utep.edu/cgi/viewcontent.cgi?article=2564&context=open_etd .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current perspective of lung transplantation
- Adjuvant Chemotherapy for Completely Resected Non-Small Cell Lung Cancer
- The Impact of Different Types of Complications on Long-Term Survival After Total Gastrectomy for Gastric Cancer
- Result of Surgical Treatment of Stage IIIB Lung Cancer
- Prognostic Implications of Postoperative Infectious Complications in Non-Small Cell Lung Cancer