Brain Tumor Res Treat.
2022 Jan;10(1):34-37. 10.14791/btrt.2022.10.e14.
Symptomatic Change of an Intracranial Neuroepithelial Cyst 7 Years After Its Incidental Finding
- Affiliations
-
- 1Departments of Neurosurgery, Tokyo Metropolitan Neurological Hospital, Tokyo, Japan
- 2Department of Neurosurgery, The University of Tokyo Hospital, Tokyo, Japan
- 3Departments of Pathology, Tokyo Metropolitan Neurological Hospital, Tokyo, Japan
- KMID: 2525300
- DOI: http://doi.org/10.14791/btrt.2022.10.e14
Abstract
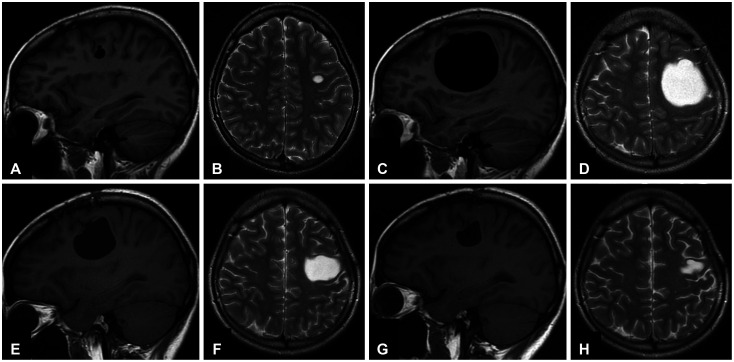
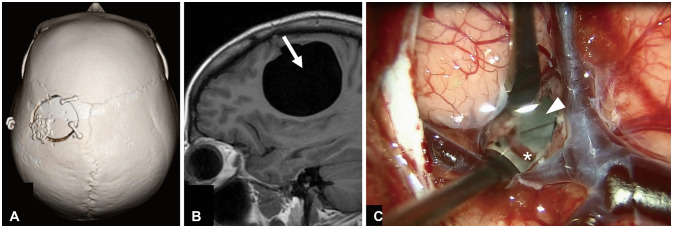
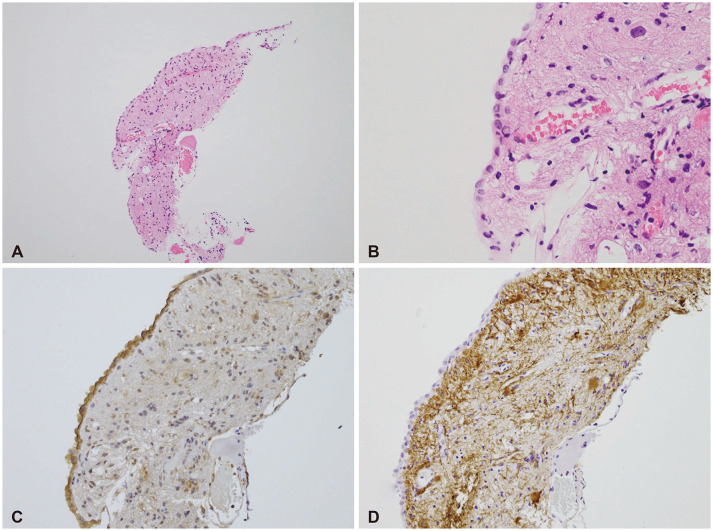
- A natural course of asymptomatic neuroepithelial cysts (NECs) is poorly understood due to its rarity.Herein we report a 23-year-old female patient of an asymptomatic NEC which grew in size from 1 cm to 5 cm and caused progressive symptoms seven years after its incidental finding. Partial resection of the cyst was performed for decompression and pathological examination and effectively achieved symptoms alleviation and regression of the cyst. Our case showed the importance of regular follow-up because NECs may show symptomatic change even in the late phase.
Figure
Reference
-
1. Robles LA, Paez JM, Ayala D, Boleaga-Duran B. Intracranial glioependymal (neuroglial) cysts: a systematic review. Acta Neurochir (Wien). 2018; 160:1439–1449. PMID: 29802560.
Article2. Morigaki R, Shinno K, Pooh KH, Nakagawa Y. Giant glioependymal cyst in an infant. J Neurosurg Pediatr. 2011; 7:175–178. PMID: 21284464.
Article3. Azzam NI, Timperley WR. Intracerebral cyst due to ectopic choroid plexus: case report. J Neurosurg. 1981; 55:651–653. PMID: 7277015.4. Asamoto S, Fukui Y, Nishiyama M, Ishikawa M, Fujita N, Nakamura S, et al. Diagnosis and surgical strategy for sacral meningeal cysts with check-valve mechanism: technical note. Acta Neurochir (Wien). 2013; 155:309–313. PMID: 23160631.
Article