Cancer Res Treat.
2022 Jan;54(1):269-276. 10.4143/crt.2021.313.
Clinical Characteristics and Treatment Outcomes of Childhood Acute Promyelocytic Leukemia in Korea: A Nationwide Multicenter Retrospective Study by Korean Pediatric Oncology Study Group
- Affiliations
-
- 1Department of Pediatrics, Dongnam Institute of Radiological and Medical Sciences, Busan, Korea
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pediatrics, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Pediatrics, Seoul National University Cancer Institute, Seoul National University College of Medicine, Seoul, Korea
- 6Division of Pediatric Hematology and Oncology, Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Korea
- 7Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University medical school, Gwangju, Korea
- 8Department of Pediatrics, Pusan National University School of Medicines, Yangsan, Korea
- 9Department of Pediatrics, Gyeongsang National University College of Medicine, Jinju, Korea
- 10Department of Pediatrics, Daegu Catholic University School of Medicine, Daegu, Korea
- 11Department of Pediatrics, University of Ulsan School of Medicine, Ulsan, Korea
- 12Department of Pediatrics, Yeungnam University College of Medicine, Daegu, Korea
- 13Department of Pediatrics, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 14Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 15Department of Pediatrics, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 16Department of Pediatrics, Kosin University of Medicine, Busan, Korea
- 17Departments of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- KMID: 2524608
- DOI: http://doi.org/10.4143/crt.2021.313
Abstract
- Purpose
Acute promyelocytic leukemia (APL) is a rare disease in children and there are some different characteristics between children and adult. We aimed to evaluate incidence, clinical characteristics and treatment outcomes of pediatric APL in Korea.
Materials and Methods
Seventy-nine pediatric APL patients diagnosed from January 2009 to December 2016 in 16 tertiary medical centers in Korea were reviewed retrospectively.
Results
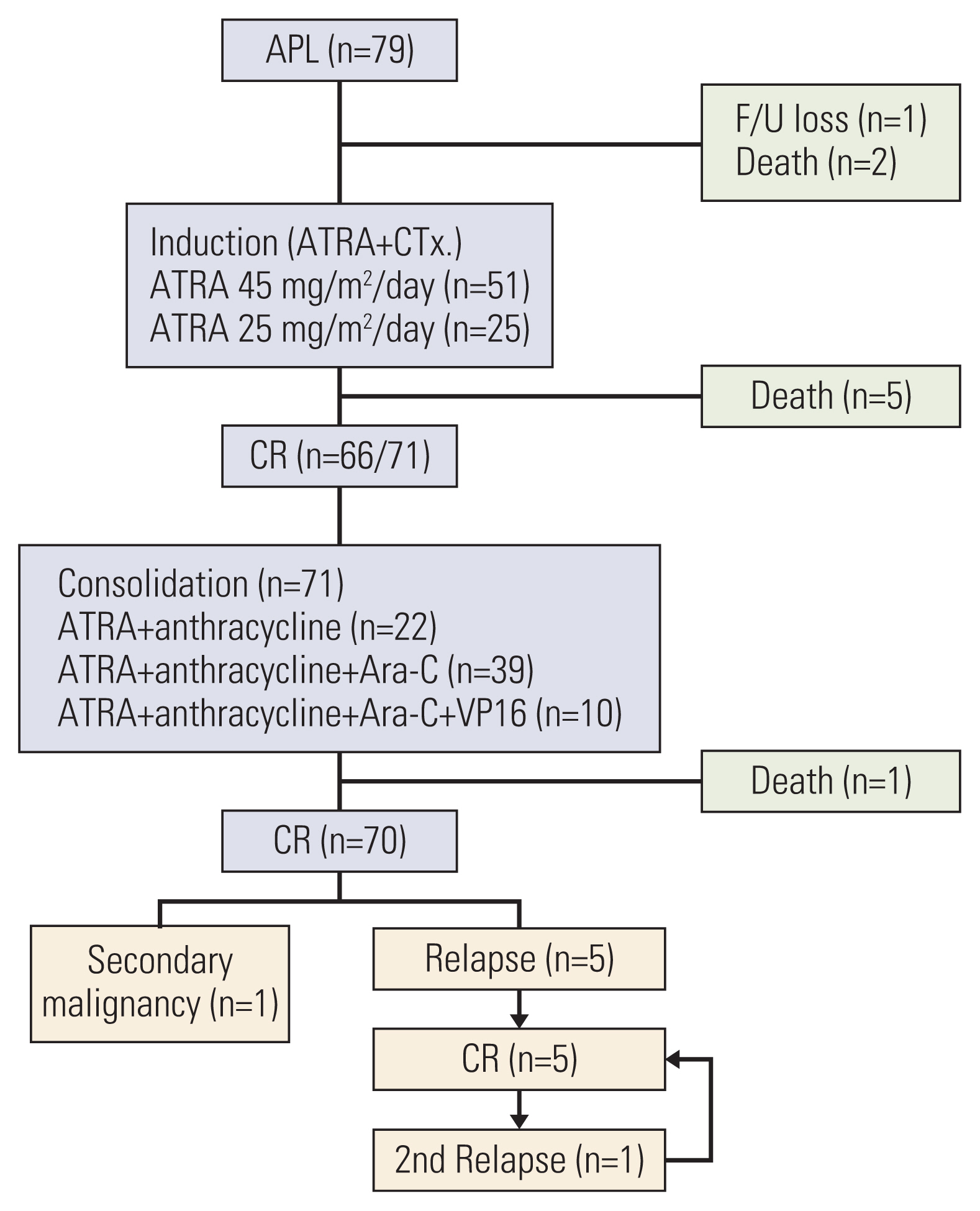
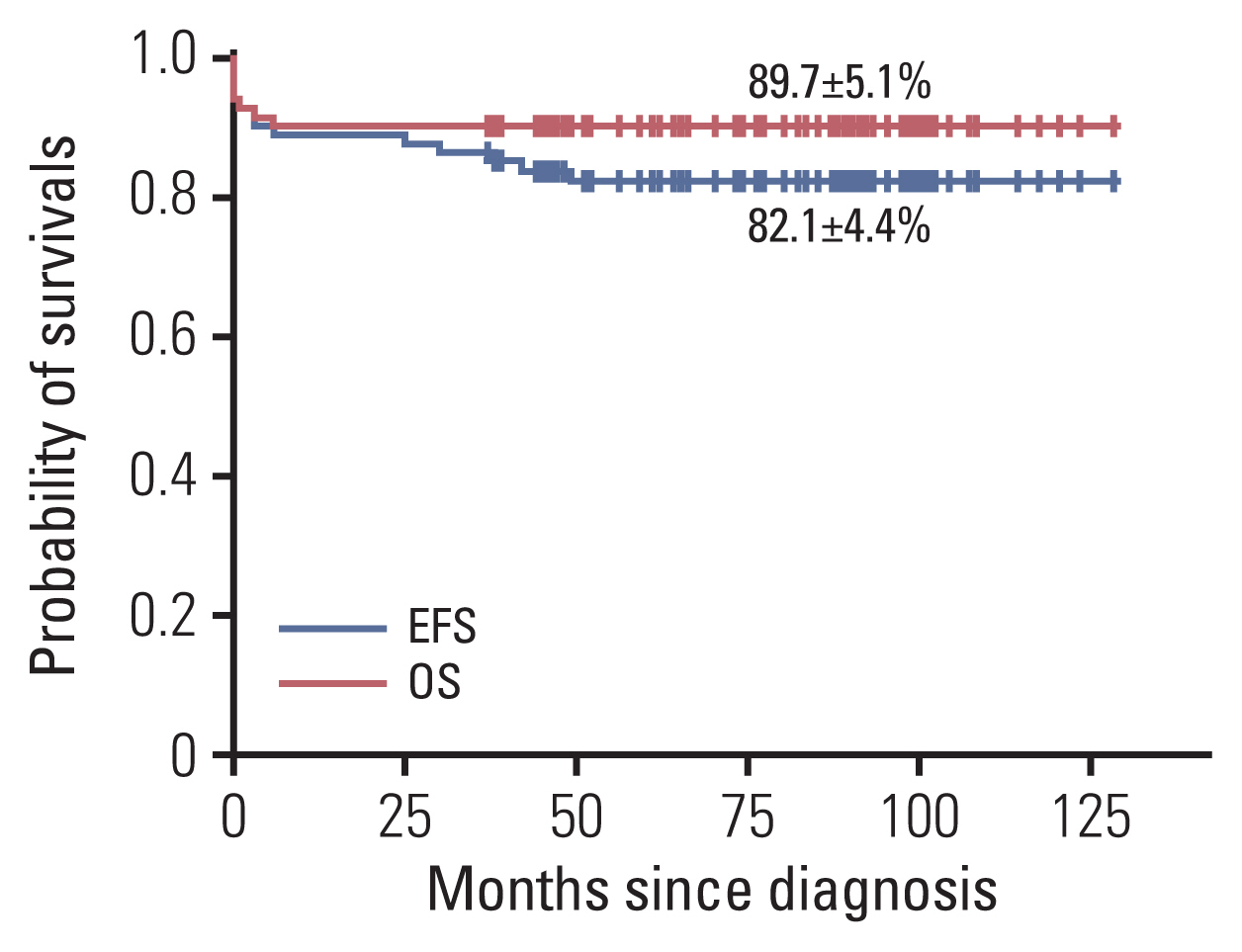
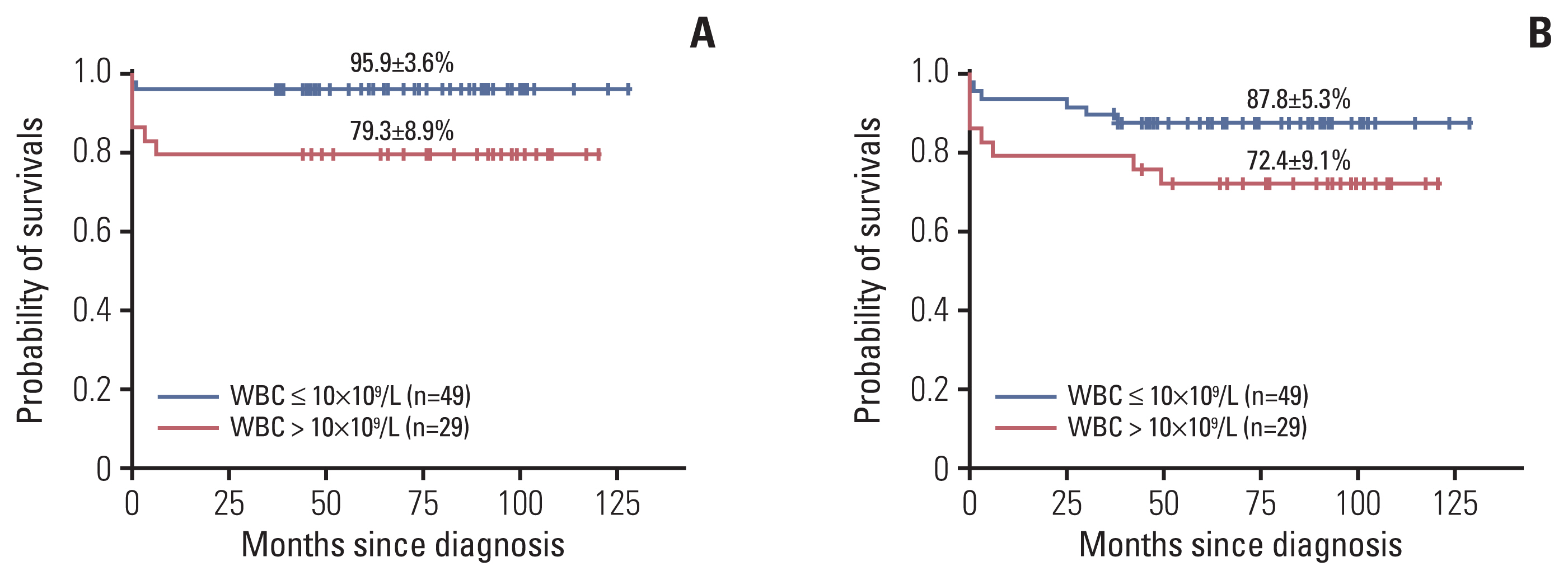
Of 801 acute myeloid leukemia children, 79 (9.9%) were diagnosed with APL. The median age at diagnosis was 10.6 years (range, 1.3 to 18.0). Male and female ratio was 1:0.93. Thirty patients (38.0%) had white blood cell (WBC) count greater than 10×109/L at diagnosis. All patients received induction therapy consisting of all-trans retinoic acid and chemotherapy. Five patients (6.6%) died during induction chemotherapy and 66 patients (86.8%) achieved complete remission (CR) after induction chemotherapy. The causes of death were three intracranial hemorrhage, one cerebral infarction, and one sepsis. Five patients (7.1%) suffered a relapse during or after maintenance chemotherapy. The estimated 4-year event-free survival and overall survival (OS) rates were 82.1%±4.4%, 89.7%±5.1%, respectively. The 4-year OS was significantly higher in patients with initial WBC < 10×109/L than in those with initial WBC ≥ 10×109/L (p=0.020).
Conclusion
This study showed that the CR rates and survival outcomes in Korean pediatric APL patients were relatively good. The initial WBC count was the most important prognostic factor and most causes of death were related to serious bleeding in the early stage of treatment.
Figure
Reference
-
References
1. Mantadakis E, Samonis G, Kalmanti M. A comprehensive review of acute promyelocytic leukemia in children. Acta Haematol. 2008; 119:73–82.
Article2. Kutny MA, Gregory J Jr, Feusner JH. Treatment of paediatric APL: how does the therapeutic approach differ from adults? Best Pract Res Clin Haematol. 2014; 27:69–78.
Article3. Yoo ES. Recent advances in the diagnosis and management of childhood acute promyelocytic leukemia. Korean J Pediatr. 2011; 54:95–105.
Article4. Jastaniah W, Alsultan A, Al Daama S, Ballourah W, Bayoumy M, Al-Anzi F, et al. Clinical characteristics and outcome of childhood acute promyelocitic leukemia (APL) in Saudi Arabia: a multicenter SAPHOS leukemia group study. Hematology. 2018; 23:316–23.
Article5. Thomas X. Acute promyelocytic leukemia: a history over 60 years. From the most malignant to the most curable form of acute leukemia. Oncol Ther. 2019; 7:33–65.6. de Botton S, Coiteux V, Chevret S, Rayon C, Vilmer E, Sanz M, et al. Outcome of childhood acute promyelocytic leukemia with all-trans-retinoic acid and chemotherapy. J Clin Oncol. 2004; 22:1404–12.
Article7. Ortega JJ, Madero L, Martin G, Verdeguer A, Garcia P, Parody R, et al. Treatment with all-trans retinoic acid and anthracycline monochemotherapy for children with acute promyelocytic leukemia: a multicenter study by the PETHEMA Group. J Clin Oncol. 2005; 23:7632–40.
Article8. Bally C, Fadlallah J, Leverger G, Bertrand Y, Robert A, Baruchel A, et al. Outcome of acute promyelocytic leukemia (APL) in children and adolescents: an analysis in two consecutive trials of the European APL Group. J Clin Oncol. 2012; 30:1641–6.
Article9. Testi AM, Biondi A, Lo Coco F, Moleti ML, Giona F, Vignetti M, et al. GIMEMA-AIEOPAIDA protocol for the treatment of newly diagnosed acute promyelocytic leukemia (APL) in children. Blood. 2005; 106:447–53.
Article10. Testi AM, D’Angio M, Locatelli F, Pession A, Lo Coco F. Acute promyelocytic leukemia (APL): comparison between children and adults. Mediterr J Hematol Infect Dis. 2014; 6:e2014032.
Article11. Abla O, Ribeiro RC. How I treat children and adolescents with acute promyelocytic leukaemia. Br J Haematol. 2014; 164:24–38.
Article12. Sanz MA, Lo Coco F, Martin G, Avvisati G, Rayon C, Barbui T, et al. Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups. Blood. 2000; 96:1247–53.13. Kim MH, Choi CS, Lee JW, Jang PS, Chung NG, Cho B, et al. Outcome of childhood acute promyelocytic leukemia treated using a modified AIDA protocol. Korean J Hematol. 2010; 45:236–41.
Article14. Testi AM, Pession A, Diverio D, Grimwade D, Gibson B, de Azevedo AC, et al. Risk-adapted treatment of acute promyelocytic leukemia: results from the International Consortium for Childhood APL. Blood. 2018; 132:405–12.
Article15. Rajpurkar M, Alonzo TA, Wang YC, Gerbing RB, Gamis AS, Feusner JH, et al. Risk markers for significant bleeding and thrombosis in pediatric acute promyelocytic leukemia: report from the Children’s Oncology Group Study AAML0631. J Pediatr Hematol Oncol. 2019; 41:51–5.
Article16. Sanz MA, Montesinos P. Open issues on bleeding and thrombosis in acute promyelocytic leukemia. Thromb Res. 2010; 125(Suppl 2):S51–4.
Article17. Castaigne S, Lefebvre P, Chomienne C, Suc E, Rigal-Huguet F, Gardin C, et al. Effectiveness and pharmacokinetics of low-dose all-trans retinoic acid (25 mg/m2) in acute promyelocytic leukemia. Blood. 1993; 82:3560–3.18. Creutzig U, Zimmermann M, Dworzak M, Urban C, Henze G, Kremens B, et al. Favourable outcome of patients with childhood acute promyelocytic leukaemia after treatment with reduced cumulative anthracycline doses. Br J Haematol. 2010; 149:399–409.
Article19. Kutny MA, Alonzo TA, Gerbing RB, Wang YC, Raimondi SC, Hirsch BA, et al. Arsenic trioxide consolidation allows anthracycline dose reduction for pediatric patients with acute promyelocytic leukemia: report from the Children’s Oncology Group Phase III Historically Controlled Trial AAML0631. J Clin Oncol. 2017; 35:3021–9.
Article20. Douer D, Zickl LN, Schiffer CA, Appelbaum FR, Feusner JH, Shepherd L, et al. All-trans retinoic acid and late relapses in acute promyelocytic leukemia: very long-term follow-up of the North American Intergroup Study I0129. Leuk Res. 2013; 37:795–801.
Article21. Dvorak CC, Agarwal R, Dahl GV, Gregory JJ, Feusner JH. Hematopoietic stem cell transplant for pediatric acute promyelocytic leukemia. Biol Blood Marrow Transplant. 2008; 14:824–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overview of Acute Promyelocytic Leukemia
- Characteristics and Therapeutic Outcomes of Acute Promyelocytic Leukemia in Children and Adolescents
- Advances in the Treatment of Childhood Acute Lymphoblastic Leukemia
- Salvage treatments with all-trans retinoic acid and arsenic trioxide-based regimens in acute promyelocytic leukemia
- Meeting Report: 2009 Symposium on Childhood Acute Lymphoblastic Leukemia - Update on the Diagnosis and Treatment for Acute Lymphoblastic Leukemia in Childhood & Adolescence; Seoul; Korea; June 27, 2009