Anesth Pain Med.
2021 Oct;16(4):322-328. 10.17085/apm.21060.
Real-time ultrasound guided thoracic epidural catheterization: a technical review
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2524443
- DOI: http://doi.org/10.17085/apm.21060
Abstract
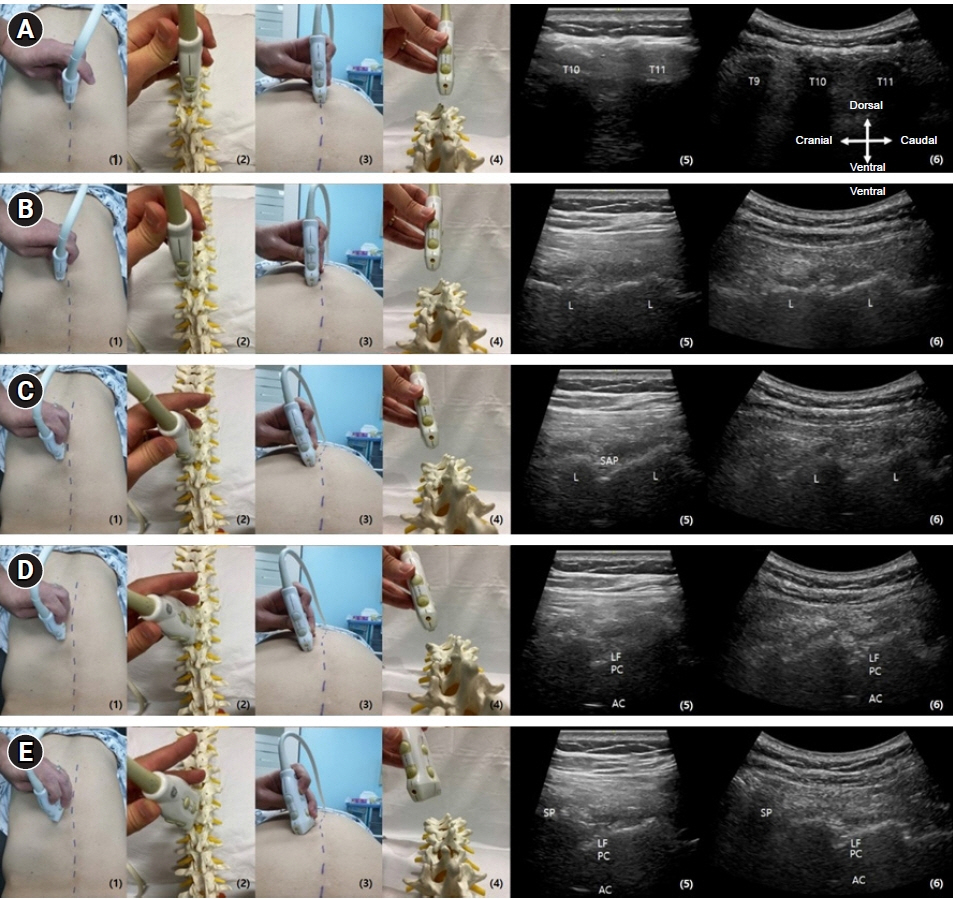
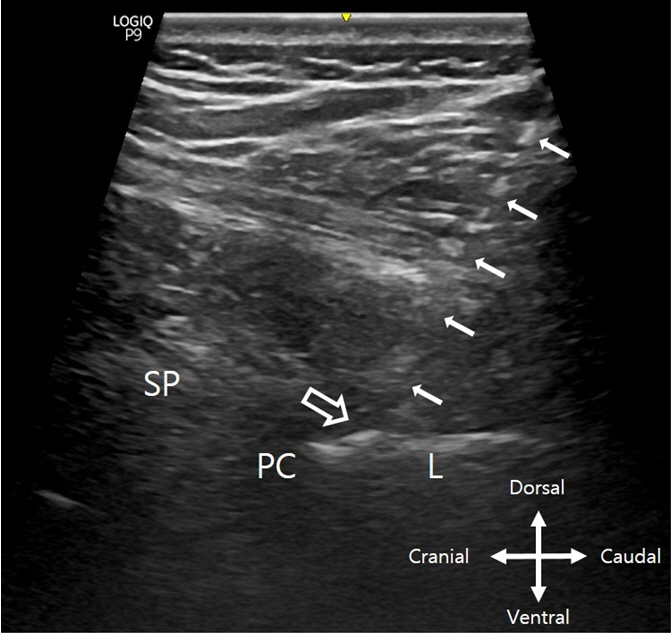
- Thoracic epidural analgesia is known to have superior perioperative pain control over intravenous opioid analgesia in open abdominal surgery and is an essential enhanced recovery after surgery component in major abdominal surgeries. Recently, the ultrasound-guided thoracic epidural catheter placement (TECP) technique has drawn attention as an alternative for the traditional landmark palpation-based TECP or fluoroscopic-guided TECP technique due to the equipment’s improvement and increased popularity. However, only a small number of studies have introduced the advantages and usefulness of ultrasound-guided TECP. Moreover, a certain level of ultrasound-guided in-plane technique is required to perform this technique. Thus, to apply ultrasound-guided TECP correctly and reduce the likelihood of side effects and complications, the practitioner must have a thorough understanding of the anatomical region, optimal block positioning, device selection, and management. In this technical review, the authors have compared the advantages and disadvantages of ultrasound-guided TECP to traditional techniques and described its technical aspects from patient positioning, ultrasound probe selection and scanning, needle insertion under ultrasound guidance, and successful thoracic epidural catheter insertion confirmation through ultrasound imaging. Additionally, the recommended epidural catheter tip placement level with the extent of its injectate epidural spread is further described in this review in reference to a recent prospective study published by the authors.
Figure
Reference
-
1. Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003; 290:2455–63.2. Radovanović D, Radovanović Z, Škorić-Jokić S, Tatić M, Mandić A, Ivković-Kapicl T. Thoracic epidural versus intravenous patient-controlled analgesia after open colorectal cancer surgery. Acta Clin Croat. 2017; 56:244–54.3. Aloia TA, Kim BJ, Segraves-Chun YS, Cata JP, Truty MJ, Shi Q, et al. A Randomized controlled trial of postoperative thoracic epidural analgesia versus intravenous patient-controlled analgesia after major hepatopancreatobiliary surgery. Ann Surg. 2017; 266:545–54.4. Pöpping DM, Elia N, Marret E, Remy C, Tramèr MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Arch Surg. 2008; 143:990–9; discussion 1000.5. Schricker T, Lattermann R. Strategies to attenuate the catabolic response to surgery and improve perioperative outcomes. Can J Anaesth. 2007; 54:414–9.6. Carli F, Halliday D. Continuous epidural blockade arrests the postoperative decrease in muscle protein fractional synthetic rate in surgical patients. Anesthesiology. 1997; 86:1033–40.7. Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: causes and management. Br J Anaesth. 2012; 109:144–54.8. Auyong DB, Hostetter L, Yuan SC, Slee AE, Hanson NA. Evaluation of ultrasound-assisted thoracic epidural placement in patients undergoing upper abdominal and thoracic surgery: a randomized, double-blind study. Reg Anesth Pain Med. 2017; 42:204–9.9. Parra MC, Washburn K, Brown JR, Beach ML, Yeager MP, Barr P, et al. Fluoroscopic guidance increases the incidence of thoracic epidural catheter placement within the epidural space: a randomized trial. Reg Anesth Pain Med. 2017; 42:17–24.10. Kim DH, Lee MS, Lee S, Yoon SH, Shin JW, Choi SS. A prospective randomized comparison of the efficacy of ultrasound- vs fluoroscopy-guided genicular nerve block for chronic knee osteoarthritis. Pain Physician. 2019; 22:139–46.11. Karmakar MK, Li X, Ho AM, Kwok WH, Chui PT. Real-time ultrasound-guided paramedian epidural access: evaluation of a novel in-plane technique. Br J Anaesth. 2009; 102:845–54.12. Kim DH, Lee JH, Sim JH, Jeong W, Lee D, Kwon HM, et al. Real-time ultrasound-guided low thoracic epidural catheter placement: technical consideration and fluoroscopic evaluation. Reg Anesth Pain Med. 2021; 46:512–7.13. Pak DJ, Gulati A. Real-time ultrasound-assisted thoracic epidural placement: a feasibility study of a novel technique. Reg Anesth Pain Med. 2018; 43:613–5.14. Gnaho A, Nau A, Gentil ME. Real-time ultrasound-guided epidural catheter insertion in obese parturients. Obstet Anesth Digest. 2016; 36:161.15. Grau T, Leipold RW, Delorme S, Martin E, Motsch J. Ultrasound imaging of the thoracic epidural space. Reg Anesth Pain Med. 2002; 27:200–6.16. Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011; 114:1459–85.17. Salman A, Arzola C, Tharmaratnam U, Balki M. Ultrasound imaging of the thoracic spine in paramedian sagittal oblique plane: the correlation between estimated and actual depth to the epidural space. Reg Anesth Pain Med. 2011; 36:542–7.18. Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen NH. Miller's anesthesia. 8th ed. Philadelphia, PA: Saunders;2014.19. Rapp HJ, Folger A, Grau T. Ultrasound-guided epidural catheter insertion in children. Anesth Analg. 2005; 101:333–9.20. Ortega-Romero A, Domingo-Rufes T, del-Olmo C, Ismael MF, Mayoral V. Ultrasound-guided interventional procedures for lumbar pain. Tech Reg Anesth Pain Manag. 2013; 17:96–106.21. Yamauchi M. Ultrasound-guided neuraxial block. Trends Anaesth Crit Care. 2012; 2:234–43.22. Greher M, Moriggl B, Peng PW, Minella CE, Zacchino M, Eichenberger U. Ultrasound-guided approach for L5 dorsal ramus block and fluoroscopic evaluation in unpreselected cadavers. Reg Anesth Pain Med. 2015; 40:713–7.23. Perlas A, Chaparro LE, Chin KJ. Lumbar neuraxial ultrasound for spinal and epidural anesthesia: a systematic review and meta-analysis. Reg Anesth Pain Med. 2016; 41:251–60.24. Vallejo MC, Phelps AL, Singh S, Orebaugh SL, Sah N. Ultrasound decreases the failed labor epidural rate in resident trainees. Int J Obstet Anesth. 2010; 19:373–8.25. Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JC, Beyene J, et al. Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ. 2013; 346:f1720.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Caudal and epidural blocks in infants and small children: historical perspective and ultrasound-guided approaches
- Incidence of intravascular insertion in thoracic epidural catheterization by using real time fluoroscopy
- Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review
- Ultrasound-guided arterial catheterization
- Comparison of landmark and real-time ultrasound-guided epidural catheter placement in the pediatric population: a prospective randomized comparative trial