Analysis of Critical COVID-19 Cases Among Children in Korea
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Pediatrics, Chung-Ang University Hospital, Seoul, Korea
- 4Department of Pediatrics, Jeonbuk National University Medical School, Jeonju, Korea
- 5Department of Pediatrics, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Division of Pulmonary, Critical Care and Sleep Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- 8Department of Pediatrics, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea
- 9Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 10Division of Infectious Diseases, Department of Internal Medicine, Incheon Medical Center, Incheon, Korea
- 11Korea Disease Control and Prevention Agency, Cheongju, Korea
- KMID: 2524177
- DOI: http://doi.org/10.3346/jkms.2022.37.e13
Abstract
- Background
Coronavirus disease 2019 (COVID-19) is generally asymptomatic or mild in otherwise healthy children, however, severe cases may occur. In this study, we report the clinical characteristics of children classified as critical COVID-19 in Korea to provide further insights into risk factors and management in children.
Methods
This study was a retrospective case series of children < 18 years of age classified as critical COVID-19. Cases were identified by the Korea Disease Control and Prevention Agency surveillance system and medical records were reviewed. Critical COVID-19 was defined as cases with severe illness requiring noninvasive (high flow nasal cannula, continuous positive airway pressure, or bilevel positive airway pressure) or invasive mechanical ventilation, extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT), between January 20, 2020 and October 7, 2021.
Results
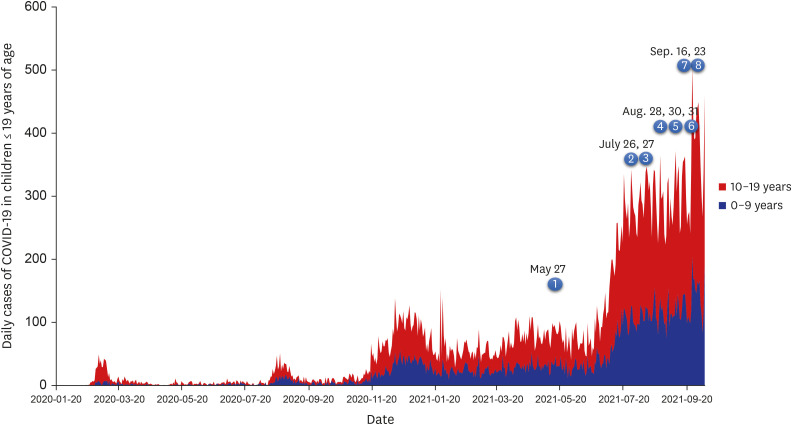
Among 39,146 cases diagnosed with COVID-19 in subjects < 18 years of age, eight cases (0.02%) were identified as critical COVID-19. The median age was 13 years (range 10 month–17 years) and male-to-female ratio was 1:1. Three children had underlying diseases; one child has asthma and major depressive disorder, one child had LennoxGastaut syndrome and one child had mental retardation and was newly diagnosed with type 2 diabetes mellitus with the diagnosis of COVID-19. Among the eight children, seven were obese (body mass index range [BMI] median 29.3, range 25.9–38.2, weight-for-length > 97% for infant) and one was overweight (BMI 21.3). All patients had fever, six patients had dyspnea or cough and other accompanied symptoms included sore throat, headache, lethargy and myalgia. Radiologic findings showed pneumonia within 1–8 days after symptom onset. Pneumonia progressed in these children for 2–6 days and was improved within 5–32 days after diagnosis. Among the eight critical cases, remdesivir was administered in six cases. Steroids were provided for all cases. Inotropics were administered in one case. Six cases were treated with noninvasive mechanical ventilator and three required mechanical ventilator. One case required ECMO due to acute respiratory distress syndrome. All cases were admitted to the intensive care unit and admission period ranged from 9–39 days. Among all critical COVID-19 cases < 18 years of age, there were no fatal cases.
Conclusion
To develop appropriate policies for children in the COVID-19 pandemic, it is important to monitor and assess the clinical burden in this population.
Keyword
Figure
Cited by 5 articles
-
Risk Factors for Severe COVID-19 in Children: A Systematic Review and Meta-Analysis
Jae Hong Choi, Soo-Han Choi, Ki Wook Yun
J Korean Med Sci. 2022;37(5):e35. doi: 10.3346/jkms.2022.37.e35.Soluble ACE2 and TMPRSS2 Levels in the Serum of Asthmatic Patients
Ji-Hyang Lee, Chae Eun Lee, Youngsang Yoo, Eunyong Shin, Jin An, Seo Young Park, Woo-Jung Song, Hyouk-Soo Kwon, You Sook Cho, Hee-Bom Moon, Tae-Bum Kim
J Korean Med Sci. 2022;37(8):e65. doi: 10.3346/jkms.2022.37.e65.Two Case Reports of Life-Threatening Croup Caused by the SARS-CoV-2 Omicron BA.2 Variant in Pediatric Patients
Soyeon Park, Jihye You, Jaehyeon Lee, Esther Park
J Korean Med Sci. 2022;37(24):e192. doi: 10.3346/jkms.2022.37.e192.SARS-CoV-2-Naïve Korean Children and Adolescents Hospitalized With COVID-19 in 2021
Youn Young Choi, Soo-Han Choi, Jae Hong Choi, Dong Hyun Kim, Joon Kee Lee, Byung Wook Eun, Hyunju Lee, Ye Kyung Kim, Bin Ahn, Seung Ha Song, Ki Wook Yun
J Korean Med Sci. 2022;37(42):e303. doi: 10.3346/jkms.2022.37.e303.Complications of the Central Nervous System in Pediatric Patients With Common Cold Coronavirus Infection During 2014–2019
Hwanhee Park, Kyung-Ran Kim, Hee Jae Huh, Yoonsun Yoon, Esther Park, Joongbum Cho, Jiwon Lee, Jeehun Lee, Ji Hye Kim, Yae-Jean Kim
J Korean Med Sci. 2023;38(46):e358. doi: 10.3346/jkms.2023.38.e358.
Reference
-
1. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020; 109(6):1088–1095. PMID: 32202343.
Article2. Mansourian M, Ghandi Y, Habibi D, Mehrabi S. COVID-19 infection in children: a systematic review and meta-analysis of clinical features and laboratory findings. Arch Pediatr. 2021; 28(3):242–248. PMID: 33483192.
Article3. Taheri L, Gheiasi SF, Taher M, Basirinezhad MH, Shaikh ZA, Dehghan Nayeri N. Clinical features of COVID-19 in newborns, infants, and children: a systematic review and meta-analysis. Compr Child Adolesc Nurs. Forthcoming. 2021; DOI: 10.1080/24694193.2021.1930288.
Article4. Viner RM, Ward JL, Hudson LD, Ashe M, Patel SV, Hargreaves D, et al. Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents. Arch Dis Child. 2021; 106(8):802–807.
Article5. Shoji K, Akiyama T, Tsuzuki S, Matsunaga N, Asai Y, Suzuki S, et al. Clinical characteristics of hospitalized COVID-19 in children: report from the COVID-19 registry in Japan. J Pediatric Infect Dis Soc. Forthcoming. 2021; DOI: 10.1093/jpids/piab085.
Article6. Han MS, Choi EH, Chang SH, Jin BL, Lee EJ, Kim BN, et al. Clinical Characteristics and viral RNA detection in children with coronavirus disease 2019 in the Republic of Korea. JAMA Pediatr. 2021; 175(1):73–80. PMID: 32857112.
Article7. Bailey LC, Razzaghi H, Burrows EK, Bunnell HT, Camacho PE, Christakis DA, et al. Assessment of 135 794 pediatric patients tested for severe acute respiratory syndrome coronavirus 2 across the United States. JAMA Pediatr. 2021; 175(2):176–184. PMID: 33226415.8. Delahoy MJ, Ujamaa D, Whitaker M, O’Halloran A, Anglin O, Burns E, et al. Hospitalizations associated with COVID-19 among children and adolescents - COVID-NET, 14 states, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(36):1255–1260. PMID: 34499627.9. Havers FP, Whitaker M, Self JL, Chai SJ, Kirley PD, Alden NB, et al. Hospitalization of adolescents aged 12–17 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 1, 2020-April 24, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(23):851–857. PMID: 34111061.10. McCormick DW, Richardson LC, Young PR, Viens LJ, Gould CV, Kimball A, et al. Deaths in children and adolescents associated with COVID-19 and MIS-C in the United States. Pediatrics. 2021; 148(5):e2021052273. PMID: 34385349.
Article11. Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021; 4(6):e2111182. PMID: 34097050.
Article12. Tsankov BK, Allaire JM, Irvine MA, Lopez AA, Sauvé LJ, Vallance BA, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2021; 103:246–256. PMID: 33227520.
Article13. Bellino S, Punzo O, Rota MC, Del Manso M, Urdiales AM, Andrianou X, et al. COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics. 2020; 146(4):e2020009399. PMID: 32665373.
Article14. Yoon Y, Kim KR, Park H, Kim S, Kim YJ. Stepwise school opening and an impact on the epidemiology of COVID-19 in the children. J Korean Med Sci. 2020; 35(46):e414. PMID: 33258334.
Article15. Yun KW, Kim KM, Kim YK, Kim MS, Kwon H, Han MS, et al. Limited benefit of facility isolation and the rationale for home care in children with mild COVID-19. J Korean Med Sci. 2021; 36(5):e45. PMID: 33527787.
Article16. Lee Y, Han JO, Lee H, Lim S. The development and operation of a home management system during the COVID-19 pandemic: experience of the local government Gyeonggi-do in Korea. J Korean Med Sci. 2021; 36(19):e134. PMID: 34002552.
Article17. Yi DY, Kim SC, Lee JH, Lee EH, Kim JY, Kim YJ, et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity: recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition. Korean J Pediatr. 2019; 62(1):3–21. PMID: 30589999.
Article18. Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York City. J Pediatr. 2020; 223:14–19.e2. PMID: 32407719.
Article19. Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020; 4(9):653–661. PMID: 32593339.
Article20. Duarte-Salles T, Vizcaya D, Pistillo A, Casajust P, Sena AG, Lai LY, et al. Thirty-day outcomes of children and adolescents with COVID-19: an international experience. Pediatrics. 2021; 148(3):e2020042929. PMID: 34049958.
Article21. Oliveira EA, Colosimo EA, Simões E Silva AC, Mak RH, Martelli DB, Silva LR, et al. Clinical characteristics and risk factors for death among hospitalised children and adolescents with COVID-19 in Brazil: an analysis of a nationwide database. Lancet Child Adolesc Health. 2021; 5(8):559–568. PMID: 34119027.
Article22. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021; 17(1):11–30. PMID: 33188364.
Article23. Holman N, Knighton P, Kar P, O’Keefe J, Curley M, Weaver A, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020; 8(10):823–833. PMID: 32798471.
Article24. Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021; 70(10):355–361. PMID: 33705371.
Article25. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020; 21(11):e13128. PMID: 32845580.
Article26. Aghili SM, Ebrahimpur M, Arjmand B, Shadman Z, Pejman Sani M, Qorbani M, et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes. 2021; 45(5):998–1016.
Article27. Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018; 12(9):755–767. PMID: 30056777.
Article28. Mahadev S, Salome CM, Berend N, King GG. The effect of low lung volume on airway function in obesity. Respir Physiol Neurobiol. 2013; 188(2):192–199. PMID: 23770312.
Article29. Spathopoulos D, Paraskakis E, Trypsianis G, Tsalkidis A, Arvanitidou V, Emporiadou M, et al. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol. 2009; 44(3):273–280. PMID: 19208374.
Article30. Chiotos K, Hayes M, Kimberlin DW, Jones SB, James SH, Pinninti SG, et al. Multicenter interim guidance on use of antivirals for children with coronavirus disease 2019/severe acute respiratory syndrome coronavirus 2. J Pediatric Infect Dis Soc. 2021; 10(1):34–48. PMID: 32918548.
Article31. Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020; 369:m1849. PMID: 32409561.
Article32. Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020; 383(21):2030–2040. PMID: 33031652.33. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020; 382(19):1787–1799. PMID: 32187464.34. Bhimraj AM, Shumaker AH, Lavergne V, Baden L, Cheng VC, Edwards KM, et al. Infectious Diseases Society of America Guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2021.
Article35. NIH. Coronavirus disease 2019 (COVID-19) Treatment guidelines 2021. Updated 2021. Accessed September 15, 2021. https://www.covid19treatmentguidelines.nih.gov/ .36. FDA. Coronavirus (COVID-19) update: FDA revokes emergency use authorization for chloroquine and hydroxychloroquine. Updated 2020. Accessed September 15, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and .37. Yin W, Mao C, Luan X, Shen DD, Shen Q, Su H, et al. Structural basis for inhibition of the RNA-dependent RNA polymerase from SARS-CoV-2 by remdesivir. Science. 2020; 368(6498):1499–1504. PMID: 32358203.
Article38. Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19 - final report. N Engl J Med. 2020; 383(19):1813–1826. PMID: 32445440.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutics in the Treatment of COVID-19 for Children and Adolescents
- Therapeutics for the treatment of coronavirus disease 2019 in children and adolescents
- Impact of COVID-19 on the clinical course of nephrotic syndrome in children: a single-center study
- The Pathologic Mechanisms and Epidemiology of Dysphagia Associated with COVID-19
- Delphi Survey for COVID-19 Vaccination in Korean Children Between 5 and 11 Years Old