Pediatr Emerg Med J.
2021 Dec;8(2):95-99. 10.22470/pemj.2021.00395.
Risk factors for acute bronchiolitis-related return visits to the emergency department
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2524001
- DOI: http://doi.org/10.22470/pemj.2021.00395
Abstract
- Purpose
Acute bronchiolitis (AB)-related return visits incur overuse of emergency medicine resources, crowding of emergency departments (EDs), and deterioration of rapport with the guardians. The authors aimed to analyze factors associated with the return visits to the ED.
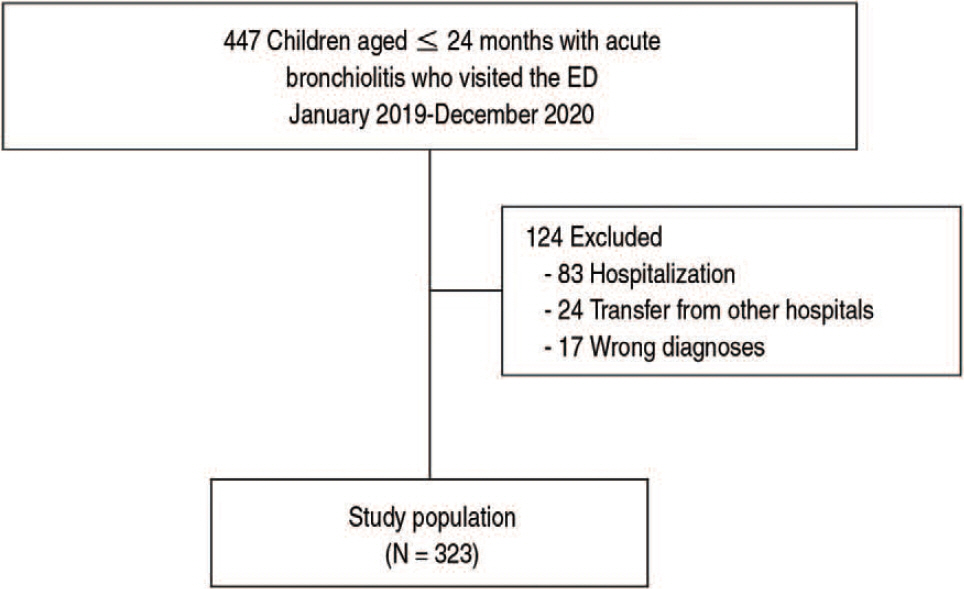
Methods
This study was conducted based on the medical records of 447 children aged 24 months or younger with AB who visited the ED from January 2019 through December 2020. A return visit was defined as an AB-related visit to the ED within 7 days of index visit. According to the return visit, we compared the clinical features. Multivariable logistic regression was conducted to identify independent factors for the return visit.
Results
Of the 323 children with AB, 77 (23.8%) made return visits. The returning children showed a younger median age (6 [interquartile range, 2-10] vs. 8 months [3-14]; P < 0.001), a lower mean oxyhemoglobin saturation (92.9 ± 4.3% vs. 97.1 ± 1.8%; P < 0.001), and higher frequencies of congenital heart diseases (22.1% vs. 10.6%; P = 0.009) and bronchopulmonary dysplasia (11.7% vs. 5.7%; P = 0.013), and respiratory syncytial virus infection (57.1% vs. 37.0%; P = 0.002). No other variables, such as the hospitalization rate, differed as per return visits. The factors associated with return visits were respiratory syncytial virus infection (adjusted odds ratio, 9.41; 95% confidence interval, 2.13-41.57), lower oxygen saturation (2.00; 1.64-2.43), and age younger than 3 months (1.25; 1.07-1.24).
Conclusion
AB-related return visits may be associated with age younger than 3 months, lower oxygen saturation, and respiratory syncytial virus infection.
Figure
Reference
-
References
1. Meissner HC. Viral Bronchiolitis in Children. N Engl J Med. 2016; 374:62–72.
Article2. Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet. 2017; 389:211–24.
Article3. Fujiogi M, Goto T, Yasunaga H, Fujishiro J, Mansbach JM, Camargo CA Jr, et al. Trends in bronchiolitis hospitalizations in the United States: 2000-2016. Pediatrics. 2019; 144:e20192614.
Article4. Silver AH, Nazif JM. Bronchiolitis. Pediatr Rev. 2019; 40:568–76.
Article5. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014; 134:e1474–502.
Article6. Kirolos A, Manti S, Blacow R, Tse G, Wilson T, Lister M, et al. A systematic review of clinical practice guidelines for the diagnosis and management of bronchiolitis. J Infect Dis. 2020; 222(Suppl 7):S672–9.
Article7. Yusuf S, Caviness AC, Adekunle-Ojo AO. Risk factors for admission in children with bronchiolitis from pediatric emergency department observation unit. Pediatr Emerg Care. 2012; 28:1132–5.
Article8. Cozzi G, Ghirardo S, Fiorese I, Proietti I, Monasta L, Minute M, et al. Risk of hospitalisation after early-revisit in the emergency department. J Paediatr Child Health. 2017; 53:850–4.
Article9. Norwood A, Mansbach JM, Clark S, Waseem M, Camargo CA Jr. Prospective multicenter study of bronchiolitis: predictors of an unscheduled visit after discharge from the emergency department. Acad Emerg Med. 2010; 17:376–82.
Article10. Principi T, Coates AL, Parkin PC, Stephens D, DaSilva Z, Schuh S. Effect of oxygen desaturations on subsequent medical visits in infants discharged from the emergency department with bronchiolitis. JAMA Pediatr. 2016; 170:602–8.
Article11. Swingler GH, Hussey GD, Zwarenstein M. Duration of illness in ambulatory children diagnosed with bronchiolitis. Arch Pediatr Adolesc Med. 2000; 154:997–1000.
Article12. Schuh S, Kwong JC, Holder L, Graves E, Macdonald EM, Finkelstein Y. Predictors of critical care and mortality in bronchiolitis after emergency department discharge. J Pediatr. 2018; 199:217–22.
Article13. Lee TK, Kyong YY, Woo SH, Park JT, Oh YM, Jung HH, et al. Factors associated with hospitalization via emergency department in children with acute bronchiolitis. Pediatr Emerg Med J. 2018; 5:49–53. Korean.
Article14. Dumas O, Mansbach JM, Jartti T, Hasegawa K, Sullivan AF, Piedra PA, et al. A clustering approach to identify severe bronchiolitis profiles in children. Thorax. 2016; 71:712–8.
Article15. Ghazaly M, Nadel S. Characteristics of children admitted to intensive care with acute bronchiolitis. Eur J Pediatr. 2018; 177:913–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Large observational study on risks predicting emergency department return visits and associated disposition deviations
- Factors associated with obesity of acute bronchiolitis in infants: association of obesity with disease severity
- Characteristics of frequent pediatric emergency department users at a tertiary university hospital
- Clinical characteristics of patients with acute bronchiolitis who visited 146 Emergency Department in Korea in 2012
- Factors associated with hospitalization via emergency department in children with acute bronchiolitis