J Korean Neurosurg Soc.
2022 Jan;65(1):151-160. 10.3340/jkns.2021.0088.
Circadian Biorhythmicity in Normal Pressure Hydrocephalus - A Case Series Report
- Affiliations
-
- 1Department of Neurosurgery and Neurotraumatology, Independent Public Regional Hospital, Szczecin, Poland
- KMID: 2523924
- DOI: http://doi.org/10.3340/jkns.2021.0088
Abstract
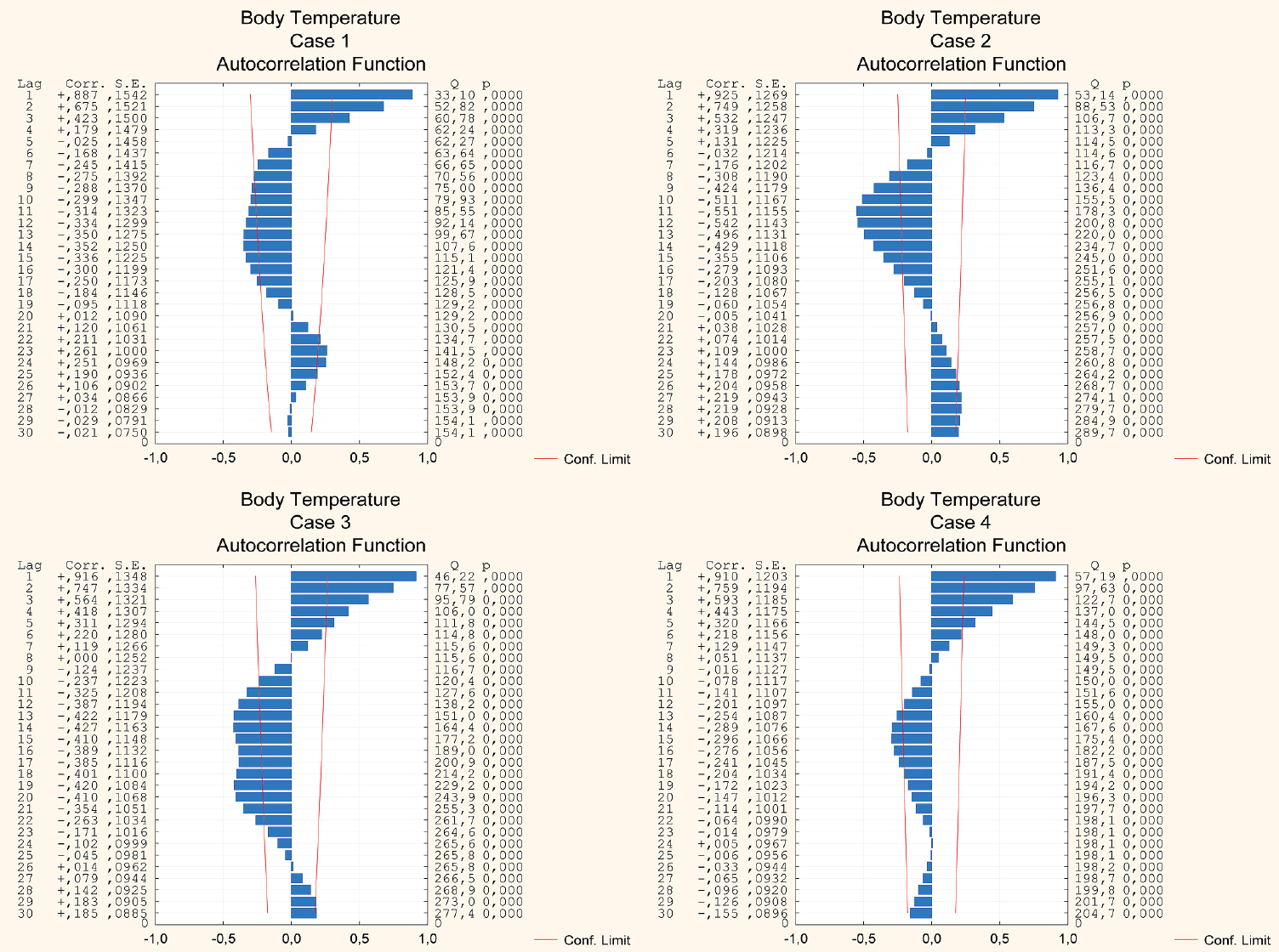
- Continuous monitoring of intracranial pressure is a well established medical procedure. Still, little is known about long-term behavior of intracranial pressure in normal pressure hydrocephalus. The present study is designed to evaluate periodicity of intracranial pressure over long-time scales using intraventricular pressure monitoring in patients with normal pressure hydrocephalus. In addition, the circadian and diurnal patterns of blood pressure and body temperature in those patients are studied. Four patients, selected with “probable” normal pressure hydrocephalus, were monitored for several dozen hours. Intracranial pressure, blood pressure, and body temperature were recorded hourly. Autocorrelation functions were calculated and cross-correlation analysis were carried out to study all the time-series data. Autocorrelation results show that intracranial pressure, blood pressure, and body temperature values follow bimodal (positive and negative) curves over a day. The cross-correlation functions demonstrate causal relationships between intracranial pressure, blood pressure, and body temperature. The results show that long-term fluctuations in intracranial pressure exhibit cyclical patterns with periods of about 24 hours. Continuous intracranial pressure recording in “probable” normal pressure hydrocephalus patients reveals circadian fluctuations not related to the day and night cycle. These fluctuations are causally related to changes in blood pressure and body temperature. The present study reveals the complete loss of the diurnal blood pressure and body temperature rhythmicities in patients with “probable” normal pressure hydrocephalus.
Keyword
Figure
Reference
-
References
1. Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 284:2177–2181. 1999.
Article2. Farajnia S, Deboer T, Rohling JH, Meijer JH, Michel S. Aging of the suprachiasmatic clock. Neuroscientist. 20:44–55. 2014.
Article3. Halberg F, Carandente F, Cornelissen G, Katinas GS. Glossary of chronobiology (author’s transl). Chronobiologia 4 Suppl. 1:1–189. 1977.4. Hassnaoui M, Pupier R, Attia J, Blanc M, Beauchaud M, Buisson B. Some tools to analyze changes of rhythms in biological time series. Biological Rhythm Research. 29:353–366. 1998.
Article5. Hofstra WA, de Weerd AW. How to assess circadian rhythm in humans: a review of literature. Epilepsy Behav. 13:438–444. 2008.
Article6. Jain S, Namboodri KKN, Kumari S, Prabhakar S. Loss of circadian rhythm of blood pressure following acute stroke. BMC Neurol. 4:1. 2004.
Article7. Keong NC, Pena A, Price SJ, Czosnyka M, Czosnyka Z, DeVito EE, et al. Diffusion tensor imaging profiles reveal specific neural tract distortion in normal pressure hydrocephalus. PLoS One. 12:e0181624. 2017.
Article8. Kim DR, Yang SH, Sung JH, Lee SW, Son BC. Significance of intracranial pressure monitoring after early decompressive craniectomy in patients with severe traumatic brain injury. J Korean Neurosurg Soc. 55:26–31. 2014.
Article9. Kropyvnytskyy IV, Saunders FW, Klemfuss H. Circadian rhythm of cerebral perfusion pressure and intracranial pressure in head injury. Brain Inj. 13:45–52. 1999.
Article10. Li X, Guan J, Hou W, Cheng S, Jiang Z, et al. The circadian intracranial pressure would be a prognostic factor in traumatic brain injury? Biol Rhythm Res. 47:823–832. 2016.
Article11. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 57(3 Suppl):S4–S16. discussion ii-v. 2016.
Article12. Shuai C, Renyi S. Autocorrelation algorithm to evaluate minimum periodicity of digital sequence. In : 2011 Fourth International Conference on Intelligent Computation Technology and Automation; 2011 Mar 28-29; Shenzhen, China. Los Alamitos: IEEE;2011. Apr. p. 961–963.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Normal Volume Hydrocephalus
- Clinical Study of Normal Pressure Hydrocephalus
- Pisa Syndrome in a Patient with Alzheimer's Disease and Concomitant Normal Pressure Hydrocephalus: A Case Report
- Argyria Accompanied by Normal Pressure Hydrocephalus
- The Impact of Comorbid Alzheimer's Disease in a Patient with Normal Pressure Hydrocephalus?