Ann Rehabil Med.
2021 Dec;45(6):459-470. 10.5535/arm.21137.
Effect of Foot Orthoses in Children With Symptomatic Flexible Flatfoot Based on Ultrasonography of the Ankle Invertor and Evertor Muscles
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2523843
- DOI: http://doi.org/10.5535/arm.21137
Abstract
Objective
To examine the changes in the cross-sectional area (CSA) ratio of the ankle invertors and evertors following rigid foot orthosis (RFO) application in children with symptomatic flexible flatfoot and to determine the correlation between the degree of change in CSA ratio and pain-severity after RFO application.
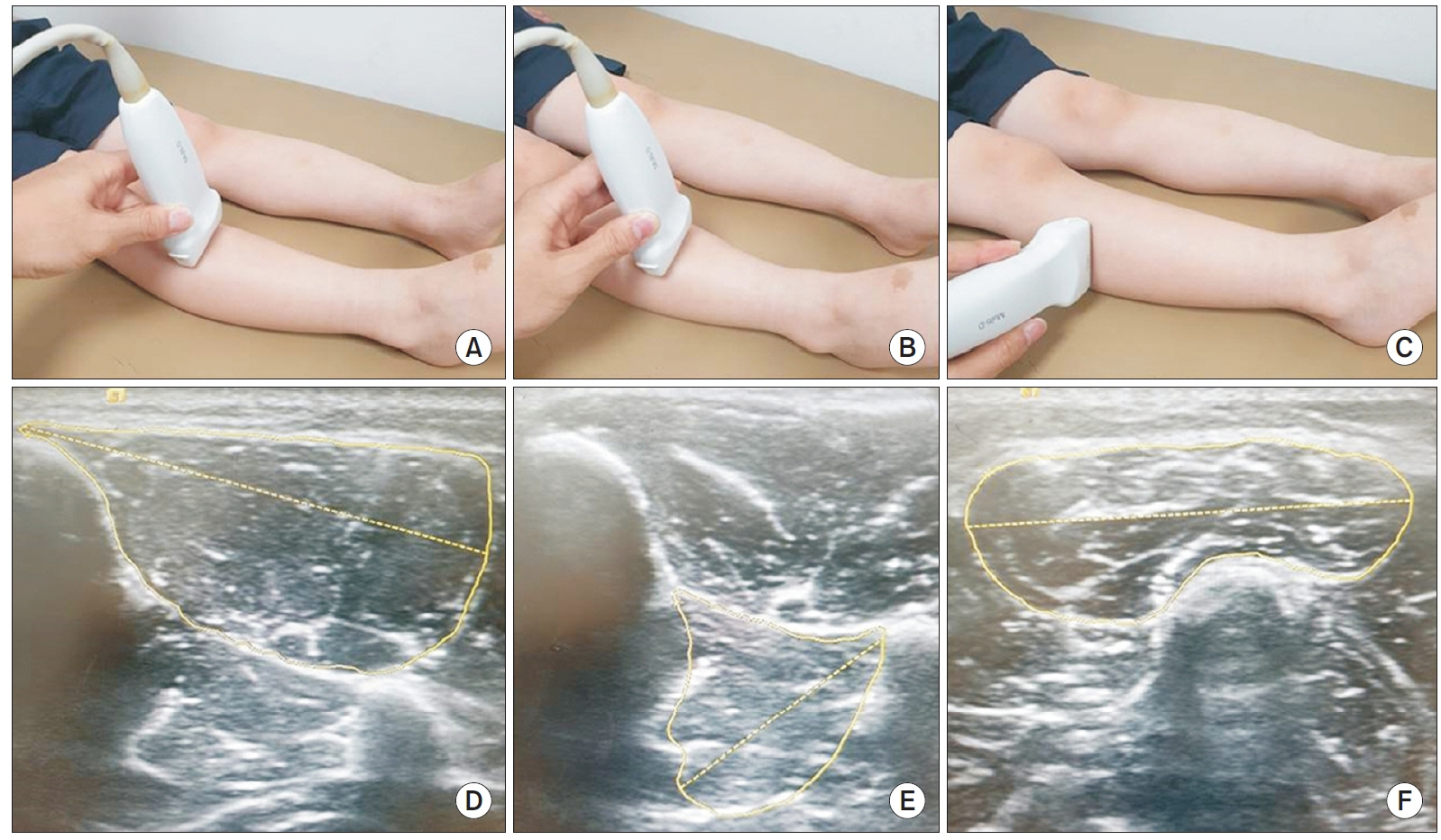
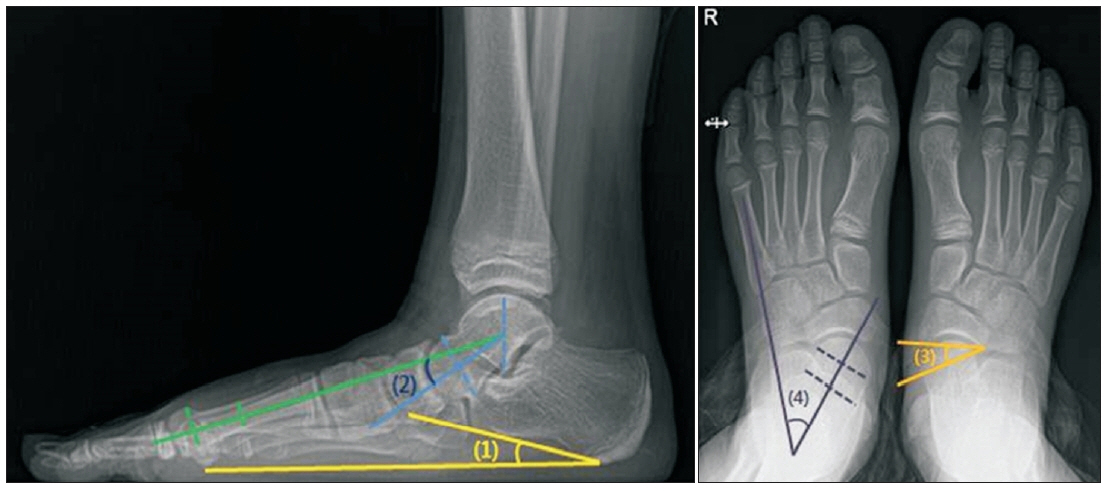
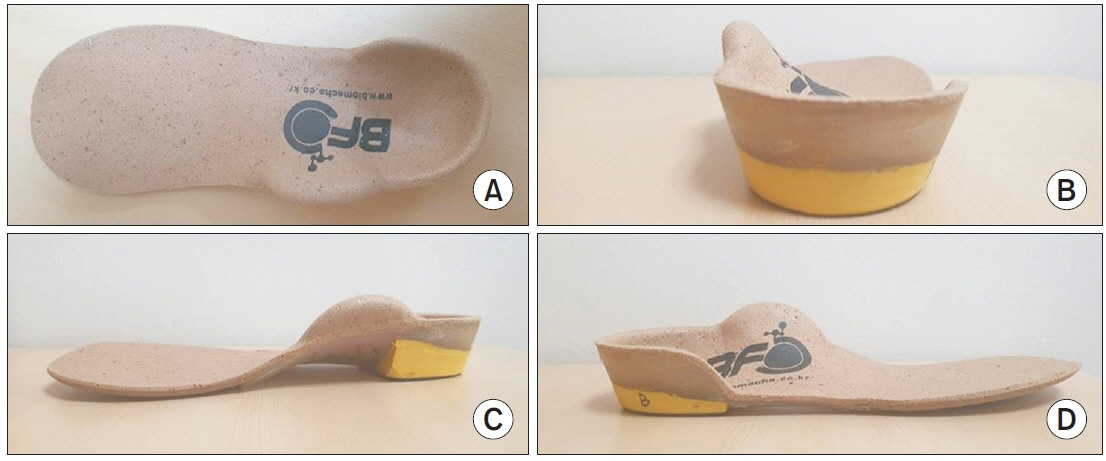
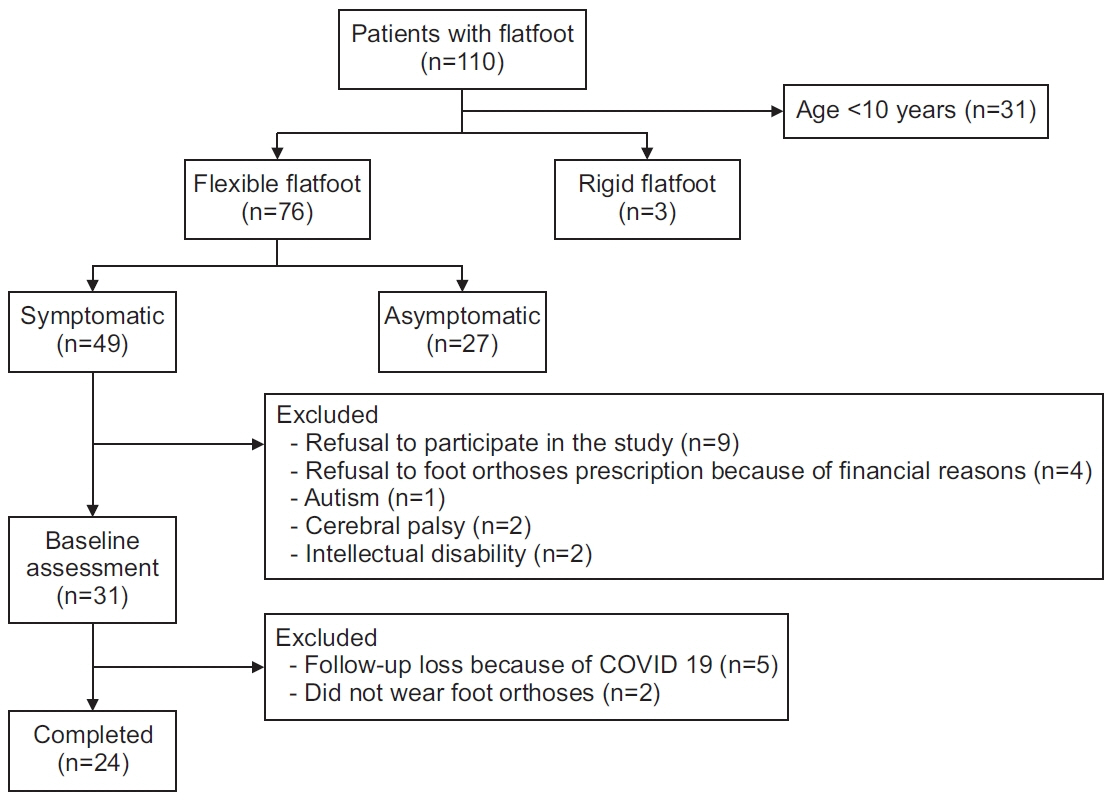
Methods
We included 24 children with symptomatic flexible flatfoot without comorbidities and measured the CSAs of tibialis anterior (TA), tibialis posterior (TP), and peroneus longus (PL) using ultrasonography, resting calcaneal stance position (RCSP) angle, calcaneal pitch (CP), Meary’s angle, talonavicular coverage angle, and talocalcaneal angle using radiography, and foot function index (FFI) at baseline and 12 months after RFO application. We analyzed 48 data by measuring both feet of 24 children. The CSA ratios, the ratio of CSA of each muscle to the sum of CSA of TA, TP, and PL, were also compared. Correlations between the degree of change in FFI, each muscle’s CSA ratio, RCSP angle, and radiographic measurements were investigated.
Results
Following RFO application, significant increase in the PL ratio and CP and significant decrease in the RCSP angle, FFI total, pain, and disability scores were observed. The degree of change in the total score, pain, and disability score of FFI were significantly correlated with the degree of change in the PL ratio and RCSP angle.
Conclusion
RFOs applied to children with symptomatic flexible flatfoot might reduce the compensatory activities of the ankle invertors, thereby increasing the PL ratio, and pain decreases as the PL ratio increases.
Figure
Cited by 1 articles
-
Biomechanical Evidence From Ultrasonography Supports Rigid Foot Orthoses in Children With Flatfoot
Joon-Ho Shin
Ann Rehabil Med. 2021;45(6):411-412. doi: 10.5535/arm.21189.
Reference
-
1. Aenumulapalli A, Kulkarni MM, Gandotra AR. Prevalence of flexible flat foot in adults: a cross-sectional study. J Clin Diagn Res. 2017; 11:AC17–20.
Article2. Sakamoto K, Kudo S. Morphological characteristics of intrinsic foot muscles among flat foot and normal foot using ultrasonography. Acta Bioeng Biomech. 2020; 22:161–6.
Article3. Sadeghi-Demneh E, Melvin JM, Mickle K. Prevalence of pathological flatfoot in school-age children. Foot (Edinb). 2018; 37:38–44.
Article4. Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006; 118:634–9.
Article5. Jandric SD, Kragulj P. Scoliosis, life style and low back pain in adolescents. Vojnosanit Pregl. 2021; 78:987–93.
Article6. Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iran J Pediatr. 2013; 23:247–60.7. Amoozadeh F, Kazemian G, Rasi AM, Kazemi P, Safaeinik F, Khazanchin A. Surveying the relationship between flatfoot and chronic mechanical low back pain. Indian J Fundam Appl Life Sci. 2015; 5:79–83.8. Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010; 4:107–21.
Article9. Murley GS, Menz HB, Landorf KB. Foot posture influences the electromyographic activity of selected lower limb muscles during gait. J Foot Ankle Res. 2009; 2:35.
Article10. Han K, Bae K, Levine N, Yang J, Lee JS. Biomechanical effect of foot orthoses on rearfoot motions and joint moment parameters in patients with flexible flatfoot. Med Sci Monit. 2019; 25:5920–8.
Article11. Murley GS, Tan JM, Edwards RM, De Luca J, Munteanu SE, Cook JL. Foot posture is associated with morphometry of the peroneus longus muscle, tibialis anterior tendon, and Achilles tendon. Scand J Med Sci Sports. 2014; 24:535–41.
Article12. Shin JB, Kim SW, You S, Lee SK, Kim HS. Biomechanic analysis of lower extremities in children and teenagers with pes planus. J Korean Acad Rehabil Med. 2008; 32:154–9.13. Angin S, Crofts G, Mickle KJ, Nester CJ. Ultrasound evaluation of foot muscles and plantar fascia in pes planus. Gait Posture. 2014; 40:48–52.
Article14. Shin Y, Ahn SY, Bok SK. Relationships between relative ankle muscle ratios, severity of symptoms, and radiologic parameters in adolescent patients with symptomatic flexible flat feet. Ann Rehabil Med. 2021; 45:123–30.
Article15. Evans AM, Rome K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur J Phys Rehabil Med. 2011; 47:69–89.16. Banwell HA, Paris ME, Mackintosh S, Williams CM. Paediatric flexible flat foot: how are we measuring it and are we getting it right?: a systematic review. J Foot Ankle Res. 2018; 11:21.
Article17. Lee HJ, Lim KB, Yoo J, Yoon SW, Jeong TH. Effect of foot orthoses on children with lower extremity growing pains. Ann Rehabil Med. 2015; 39:285–93.
Article18. Lee HJ, Lim KB, Yoo J, Yoon SW, Yun HJ, Jeong TH. Effect of custom-molded foot orthoses on foot pain and balance in children with symptomatic flexible flat feet. Ann Rehabil Med. 2015; 39:905–13.
Article19. Ueki Y, Sakuma E, Wada I. Pathology and management of flexible flat foot in children. J Orthop Sci. 2019; 24:9–13.
Article20. Dars S, Uden H, Banwell HA, Kumar S. The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: a systematic review: Update. PLoS One. 2018; 13:e0193060.
Article21. Unver B, Erdem EU, Akbas E. Effects of short-foot exercises on foot posture, pain, disability, and plantar pressure in pes planus. J Sport Rehabil. 2019; 29:436–40.
Article22. Bok SK, Kim BO, Lim JH, Ahn SY. Effects of custommade rigid foot orthosis on pes planus in children over 6 years old. Ann Rehabil Med. 2014; 38:369–75.
Article23. Jay RM, Schoenhaus HD, Seymour C, Gamble S. The Dynamic Stabilizing Innersole System (DSIS): the management of hyperpronation in children. J Foot Ankle Surg. 1995; 34:124–31.
Article24. Whitford D, Esterman A. A randomized controlled trial of two types of in-shoe orthoses in children with flexible excess pronation of the feet. Foot Ankle Int. 2007; 28:715–23.
Article25. Youn KJ, Ahn SY, Kim BO, Park IS, Bok SK. Longterm effect of rigid foot orthosis in children older than six years with flexible flat foot. Ann Rehabil Med. 2019; 43:224–9.
Article26. Johnson AW, Bruening DA, Violette VA, Perkins KV, Thompson CL, Ridge ST. Ultrasound imaging is reliable for tibialis posterior size measurements. J Ultrasound Med. 2020; 39:2305–12.
Article27. Ahn SY, Bok SK, Kim BO, Park IS. The effects of talus control foot orthoses in children with flexible flatfoot. J Am Podiatr Med Assoc. 2017; 107:46–53.
Article28. Sobel E, Levitz SJ, Caselli MA, Tran M, Lepore F, Lilja E, et al. Reevaluation of the relaxed calcaneal stance position: reliability and normal values in children and adults. J Am Podiatr Med Assoc. 1999; 89:258–64.
Article29. Schon LC, Weinfeld SB, Horton GA, Resch S. Radiographic and clinical classification of acquired midtarsus deformities. Foot Ankle Int. 1998; 19:394–404.
Article30. Arunakul M, Amendola A, Gao Y, Goetz JE, Femino JE, Phisitkul P. Tripod Index: diagnostic accuracy in symptomatic flatfoot and cavovarus foot: part 2. Iowa Orthop J. 2013; 33:47–53.31. Bourdet C, Seringe R, Adamsbaum C, Glorion C, Wicart P. Flatfoot in children and adolescents: analysis of imaging findings and therapeutic implications. Orthop Traumatol Surg Res. 2013; 99:80–7.
Article32. Coughlin MJ, Kaz A. Correlation of Harris mats, physical exam, pictures, and radiographic measurements in adult flatfoot deformity. Foot Ankle Int. 2009; 30:604–12.
Article33. Sensiba PR, Coffey MJ, Williams NE, Mariscalco M, Laughlin RT. Inter- and intraobserver reliability in the radiographic evaluation of adult flatfoot deformity. Foot Ankle Int. 2010; 31:141–5.
Article34. Moraleda L, Mubarak SJ. Flexible flatfoot: differences in the relative alignment of each segment of the foot between symptomatic and asymptomatic patients. J Pediatr Orthop. 2011; 31:421–8.35. Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991; 44:561–70.
Article36. Budiman-Mak E, Conrad K, Stuck R, Matters M. Theoretical model and Rasch analysis to develop a revised Foot Function Index. Foot Ankle Int. 2006; 27:519–27.
Article37. In TS, Jung JH, Kim K, Jung KS, Cho HY. The reliability and validity of the Korean version of the foot function index for patients with foot complaints. J Phys Ther Sci. 2017; 29:53–56.
Article38. Staheli LT. Planovalgus foot deformity: current status. J Am Podiatr Med Assoc. 1999; 89:94–9.
Article39. Driano AN, Staheli L, Staheli LT. Psychosocial development and corrective shoewear use in childhood. J Pediatr Orthop. 1998; 18:346–9.
Article40. Lee EC, Kim MO, Kim HS, Hong SE. Changes in resting calcaneal stance position angle following insole fitting in children with flexible flatfoot. Ann Rehabil Med. 2017; 41:257–65.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Custom-Molded Foot Orthoses on Foot Pain and Balance in Children With Symptomatic Flexible Flat Feet
- Isokinetic Evaluation of Ankle Invertor and Evertor in Patients with Chronic Ankle Sprain
- Long Term Effect of Custom-Molded Foot Orthoses on Foot Pain and Balance in Children with Symptomatic Flexible Flat Feet
- Calcaneo-stop Procedure for Management of Pediatric Symptomatic Flexible Flatfoot
- Effect of Pressure Based Customized 3-Dimensional Printing Insole in Pediatric Flexible Flat Foot Patients