Korean J Transplant.
2021 Dec;35(4):275-280. 10.4285/kjt.21.0021.
Careful neurologic examination and treatment for intracranial hemorrhage after liver transplantation in patients with alcoholic cirrhosis: case reports
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Pusan National University Hospital, Busan, Korea
- 2Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Veterans Health Service Medical Center, Seoul, Korea
- 3Department of Neurosurgery, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 4Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2523679
- DOI: http://doi.org/10.4285/kjt.21.0021
Abstract
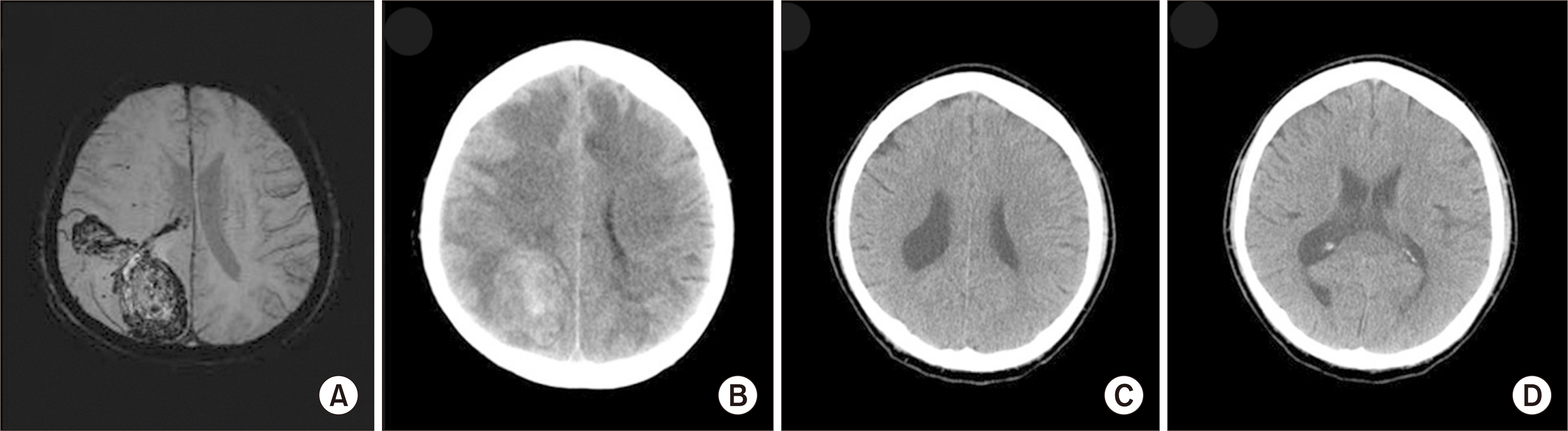
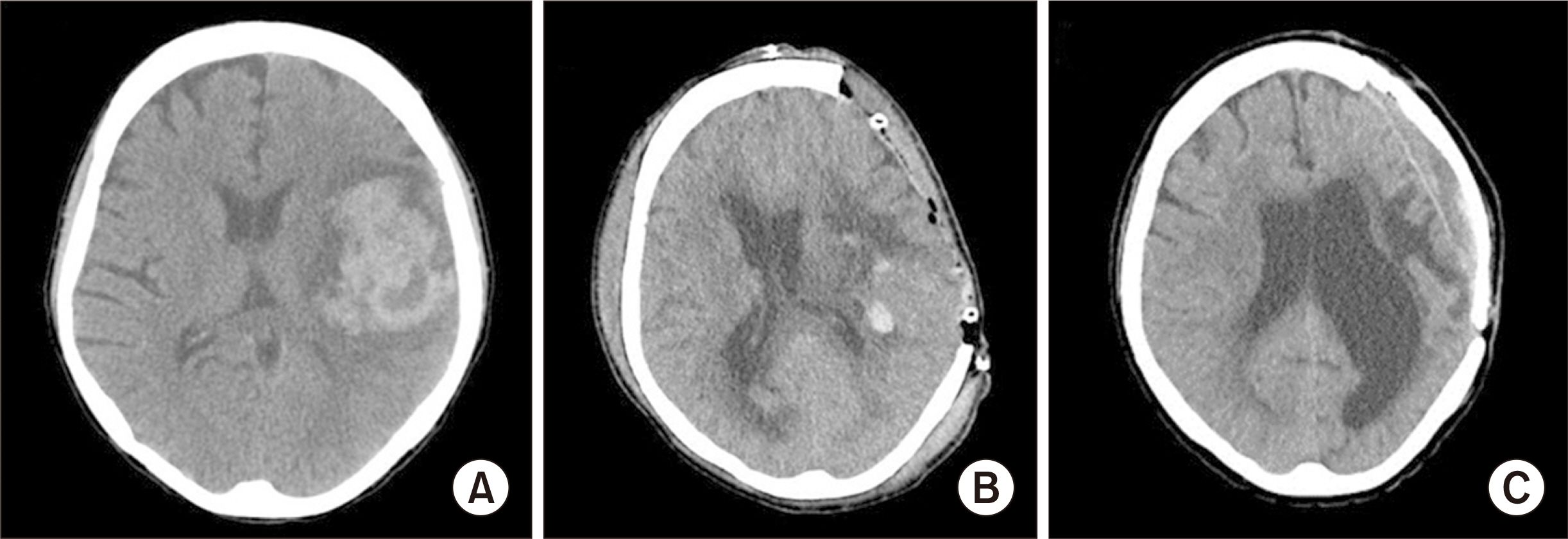
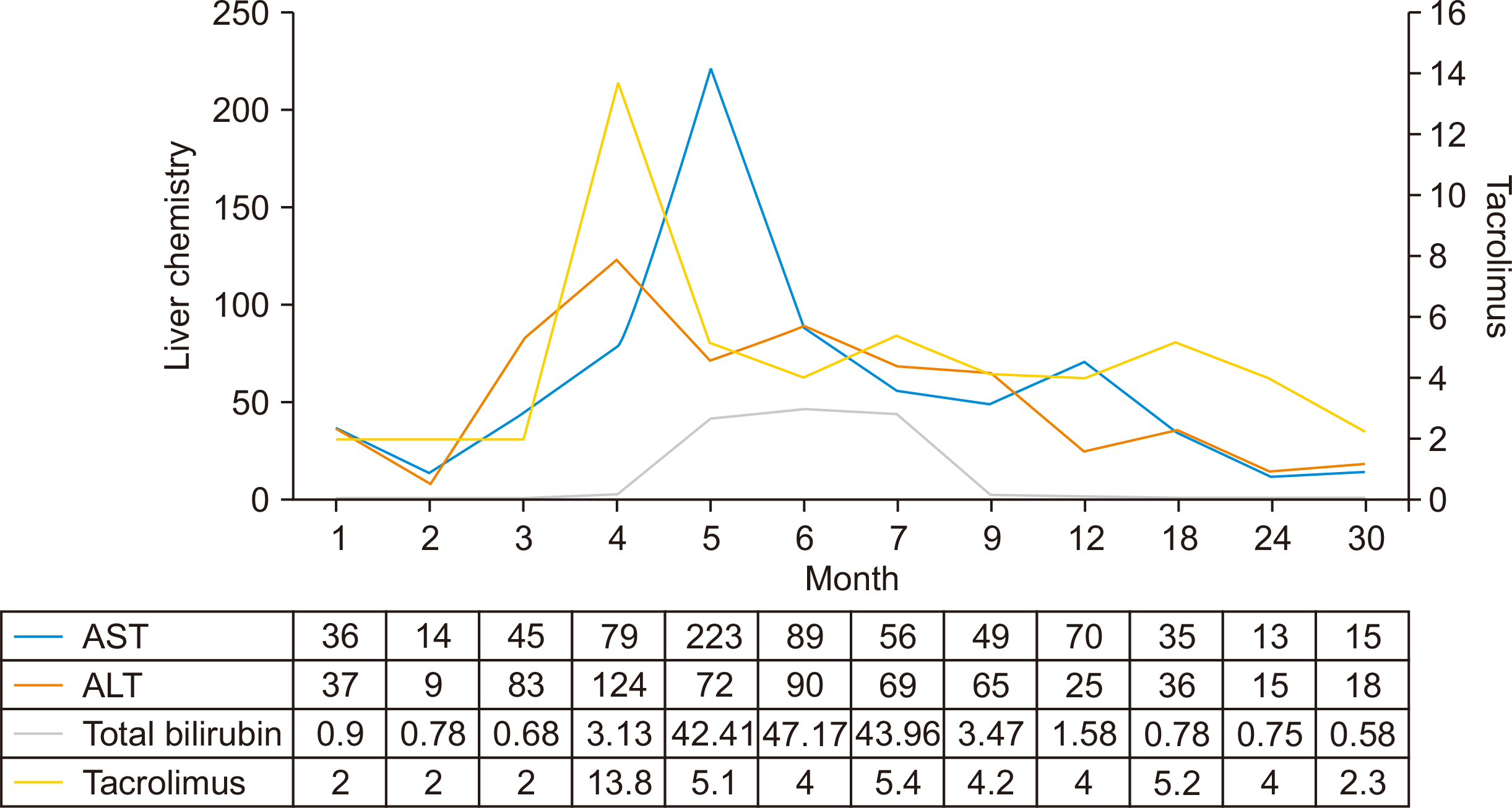
- Intracranial hemorrhage (ICH) following liver transplantation is a potentially devastating complication. Although hypertension and thrombocytopenia are well-known risk factors for ICH in the general population, their roles in ICH after liver transplantation have not been well established. ICH occurred in two patients with alcoholic cirrhosis after deceased donor liver transplantation. A 38-year-old man presented with acute ICH in the right parietal lobe on day 16 after transplantation, with decreased level of consciousness and seizure. His mental status improved with immediate neurological treatment without surgery. In the second case, a 42-year-old woman had acute ICH in the left frontoparietal lobes on day 9 after transplantation, with generalized tonic-clonic seizures. Urgent cerebral decompression was performed. The patient’s neurological symptoms gradually recovered. In both cases, the blood platelet count was less than 50,000/mm 3 . Monitoring cerebral pressure for ICH is an invasive and challenging method, especially in patients with cirrhosis who have issues with hemostasis. Surgeons should be critically mindful of the risk of rapid neurological deterioration in patients with cirrhosis. Careful neurologic examination and immediate treatment to lower intracranial pressure for ICH after liver transplantation in patients with alcoholic cirrhosis are very important.
Figure
Reference
-
1. Menegaux F, Keeffe EB, Andrews BT, Egawa H, Monge H, Concepcion W, et al. 1994; Neurological complications of liver transplantation in adult versus pediatric patients. Transplantation. 58:447–50. DOI: 10.1097/00007890-199408270-00010. PMID: 8073514.
Article2. Bronster DJ, Emre S, Boccagni P, Sheiner PA, Schwartz ME, Miller CM. 2000; Central nervous system complications in liver transplant recipients: incidence, timing, and long-term follow-up. Clin Transplant. 14:1–7. DOI: 10.1034/j.1399-0012.2000.140101.x. PMID: 10693627.3. Ghaus N, Bohlega S, Rezeig M. 2001; Neurological complications in liver transplantation. J Neurol. 248:1042–8. DOI: 10.1007/s004150170023. PMID: 12013580.
Article4. Chabolla DR, Wszolek ZK. 2006; Pharmacologic management of seizures in organ transplant. Neurology. 67(12 Suppl 4):S34–8. DOI: 10.1212/WNL.67.12_suppl_4.S34. PMID: 17190920.
Article5. Mirski MA, Varelas PN. 2008; Seizures and status epilepticus in the critically ill. Crit Care Clin. 24:115–47. ixDOI: 10.1016/j.ccc.2007.11.005. PMID: 18241782.
Article6. Shepard PW, St Louis EK. 2012; Seizure treatment in transplant patients. Curr Treat Options Neurol. 14:332–47. DOI: 10.1007/s11940-012-0180-y. PMID: 22660960. PMCID: PMC3656593.
Article7. Gao W, Li J, Nguyen-Buckley C, Nguyen-Lee J, Wray C, Agopian V, et al. 2020; Intraoperative hypertension and thrombocytopenia associated with intracranial hemorrhage after liver transplantation. Transplantation. 104:535–41. DOI: 10.1097/TP.0000000000002899. PMID: 31397798.
Article8. Yoon J, Jung Y, Kim H, Park B, Choi D. 2020; Cause-specific mortality and associated factors related to death after kidney and liver transplantation: a Korean nationwide study. Korean J Transplant. 34(Suppl 1):S119. DOI: 10.4285/ATW2020.OR-1070.
Article9. Wang WL, Yang ZF, Lo CM, Liu CL, Fan ST. 2000; Intracerebral hemorrhage after liver transplantation. Liver Transpl. 6:345–8. DOI: 10.1053/lv.2000.6138. PMID: 10827237.
Article10. Wijdicks EF, de Groen PC, Wiesner RH, Krom RA. 1995; Intracerebral hemorrhage in liver transplant recipients. Mayo Clin Proc. 70:443–6. DOI: 10.4065/70.5.443. PMID: 7731253.
Article11. Oh SY, Lee H, Park YH, Ryu HG. 2016; Intracranial hemorrhage induced uncontrolled seizure in a deceased donor liver transplant patient: a case report. Korean J Anesthesiol. 69:527–31. DOI: 10.4097/kjae.2016.69.5.527. PMID: 27703637. PMCID: PMC5047992.
Article12. Takahashi K, Nagai S, Safwan M, Liang C, Ohkohchi N. 2018; Thrombocytopenia after liver transplantation: should we care? World J Gastroenterol. 24:1386–97. DOI: 10.3748/wjg.v24.i13.1386. PMID: 29632420. PMCID: PMC5889819.
Article13. Gallagher TK, Thomas KA, Ladner DP, Ganger D, Sorond FA, Prabhakaran S, et al. 2018; Incidence and risk factors of intracranial hemorrhage in liver transplant recipients. Transplantation. 102:448–53. DOI: 10.1097/TP.0000000000002005. PMID: 29189631. PMCID: PMC5820203.
Article14. Bianchini A, DʼAndrea R, Lepic B, Querci L, Laici C, Siniscalchi A. 2019; Intracranial hemorrhage diagnosed with transcranial ultrasound in a comatose, postliver transplant patient. J Stroke Cerebrovasc Dis. 28:104357. DOI: 10.1016/j.jstrokecerebrovasdis.2019.104357. PMID: 31495670.
Article15. Steiner T, Al-Shahi Salman R, Beer R, Christensen H, Cordonnier C, Csiba L, et al. 2014; European Stroke Organisation (ESO) guidelines for the management of spontaneous intracerebral hemorrhage. Int J Stroke. 9:840–55. DOI: 10.1111/ijs.12309. PMID: 25156220.
Article16. Toyoda K, Steiner T, Epple C, Kern R, Nagayama M, Shinohara Y, et al. 2013; Comparison of the European and Japanese guidelines for the acute management of intracerebral hemorrhage. Cerebrovasc Dis. 35:419–29. DOI: 10.1159/000351754. PMID: 23712243.
Article17. Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. 2015; Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 46:2032–60. DOI: 10.1161/STR.0000000000000069. PMID: 26022637.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Retinal Hemorrhage in Alcoholic Cirrhosis
- Unexpected Death due to Massive Nontraumatic Intraabdominal Hemorrhage in association with Liver Cirrhosis
- Massive bleeding from a rectal Dieulafoy lesion in a patient with alcoholic cirrhosis
- Indication and Prognosis of Liver Transplantation
- Three Cases of Spontaneous Muscle Hematoma in Alcoholic Liver Cirrhosis