Korean J Transplant.
2021 Dec;35(4):268-274. 10.4285/kjt.21.0009.
Salvage aorto-hepatic jump graft for hepatic artery thrombosis following living donor liver transplantation: a case report with 10-year follow-up
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2523678
- DOI: http://doi.org/10.4285/kjt.21.0009
Abstract
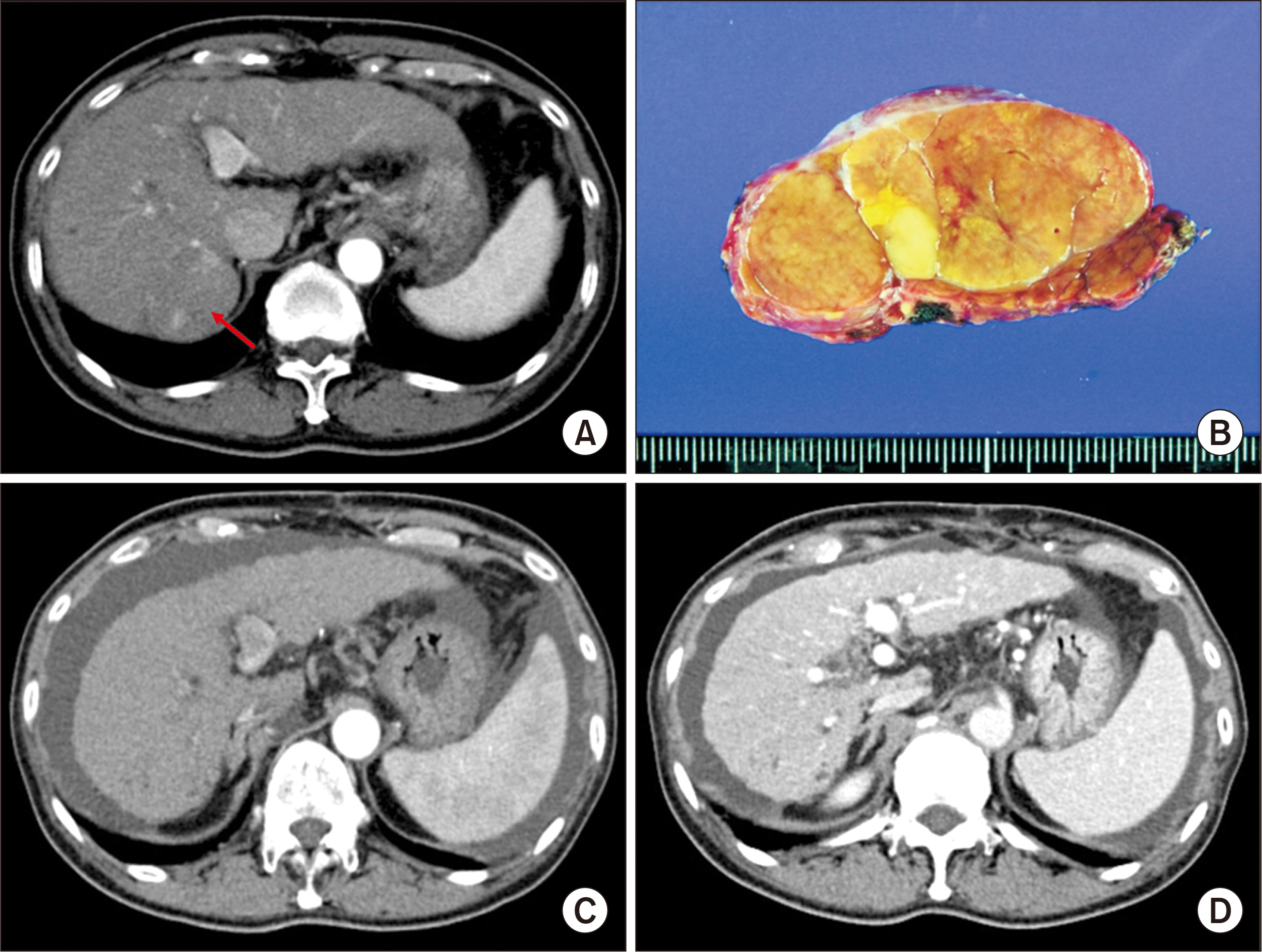
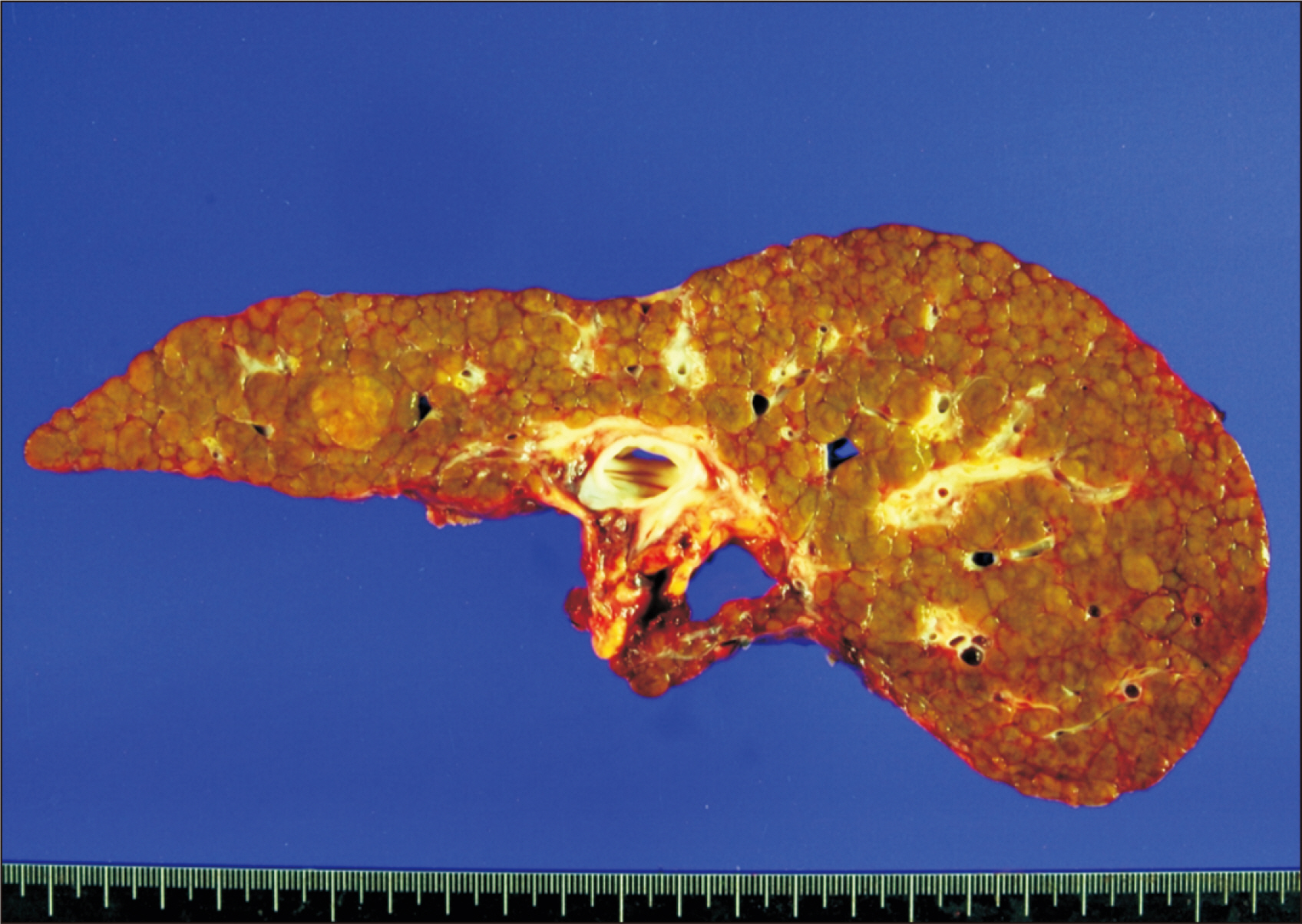
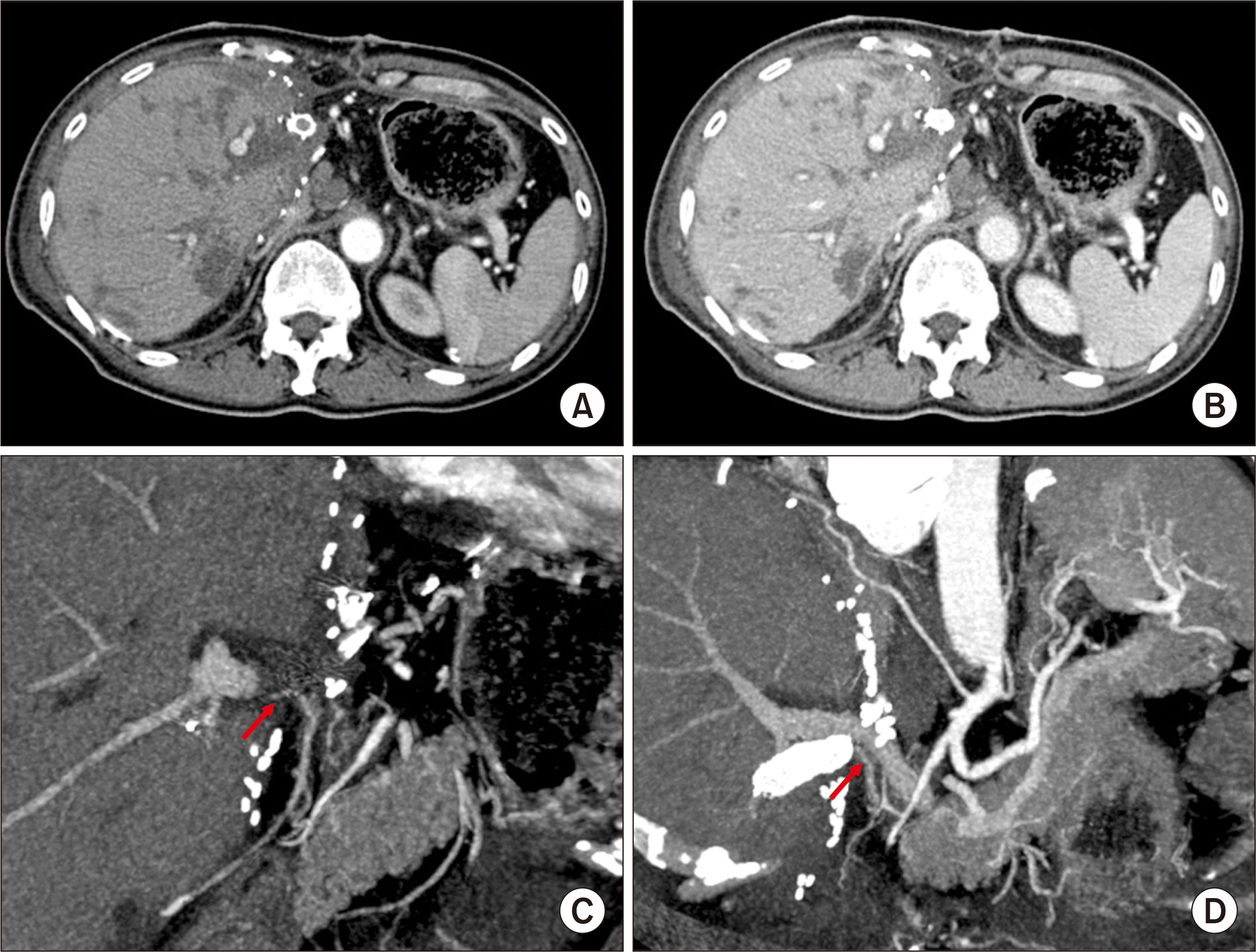
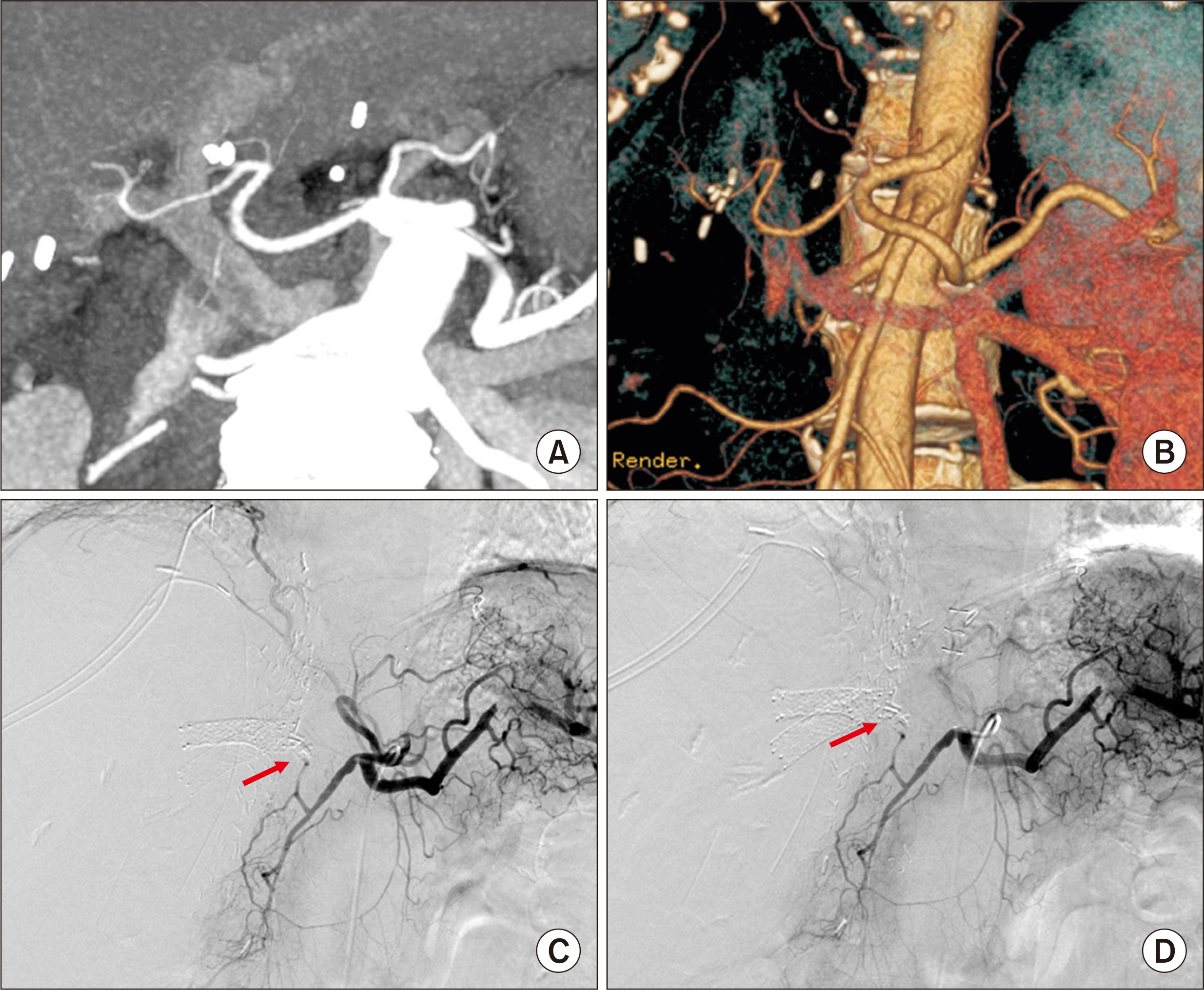
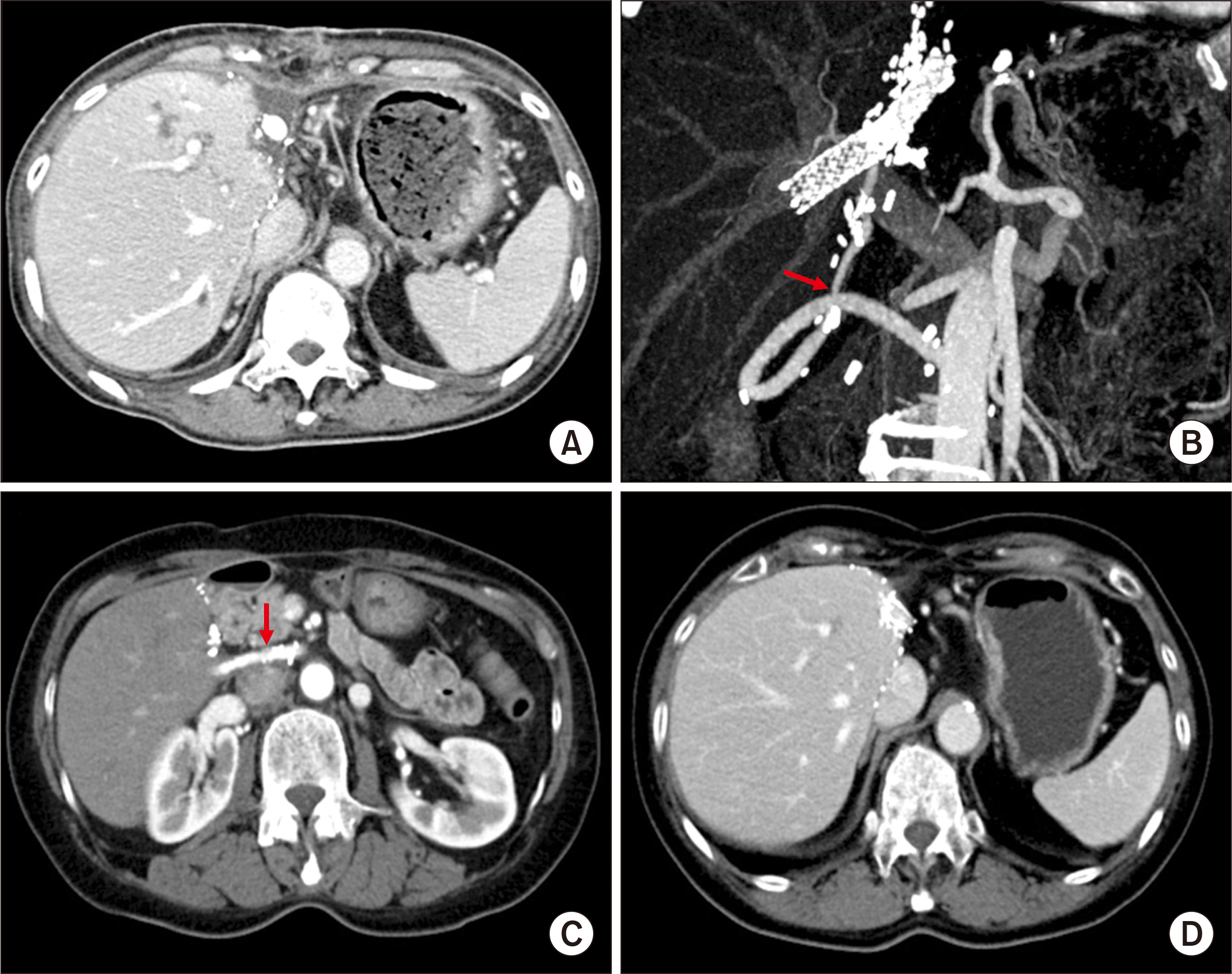
- Hepatic artery thrombosis (HAT) following living donor liver transplantation (LDLT) is a lethal complication. We present the case of a patient who underwent salvage redo hepatic artery reconstruction using an aorto-hepatic jump graft because of HAT following LDLT. A 64-year-old female patient diagnosed with hepatitis C virus-associated liver cirrhosis and hepatocellular carcinoma underwent salvage LDLT using a modified right liver graft. Partial graft infarct was identified at posttransplant day 4, and by day 9, it had spread. Celiac arteriography showed complete occlusion of the graft hepatic artery. We performed redo hepatic artery reconstruction using a fresh iliofemoral artery homograft 10 days after the LDLT operation because such a vessel homograft was available at our institutional tissue bank. The infrarenal aorta was dissected and an iliofemoral artery graft was anastomosed. Soon after hepatic artery revascularization, liver function progressively improved, and the infarct area at the liver graft was reduced. The patient has been doing well for 10 years without any vascular complications. In conclusion, our experience with this case suggests that salvage redo hepatic artery reconstruction using an aorto-hepatic jump graft is a feasible option to treat HAT following LDLT, as in deceased donor liver transplantation.
Keyword
Figure
Reference
-
1. Stange BJ, Glanemann M, Nuessler NC, Settmacher U, Steinmüller T, Neuhaus P. 2003; Hepatic artery thrombosis after adult liver transplantation. Liver Transpl. 9:612–20. DOI: 10.1053/jlts.2003.50098. PMID: 12783404.2. Abou El-Ella K, Al Sebayel M, Ramirez C, Hussien R. 2001; Outcome and risk factors of hepatic artery thrombosis after orthotopic liver transplantation in adults. Transplant Proc. 33:2712–3. DOI: 10.1016/S0041-1345(01)02157-1. PMID: 11498135.
Article3. Song S, Kwon CH, Moon HH, Lee S, Kim JM, Joh JW, et al. 2015; Single-center experience of consecutive 522 cases of hepatic artery anastomosis in living-donor liver transplantation. Transplant Proc. 47:1905–11. DOI: 10.1016/j.transproceed.2015.06.014. PMID: 26293071.
Article4. Ahn CS, Hwang S, Moon DB, Song GW, Ha TY, Park GC, et al. 2012; Right gastroepiploic artery is the first alternative inflow source for hepatic arterial reconstruction in living donor liver transplantation. Transplant Proc. 44:451–3. DOI: 10.1016/j.transproceed.2012.01.057. PMID: 22410041.
Article5. Park GC, Moon DB, Kang SH, Ahn CS, Hwang S, Kim KH, et al. 2019; Overcoming hepatic artery thrombosis after living donor liver transplantations: an experience from Asan Medical Center. Ann Transplant. 24:588–93. DOI: 10.12659/AOT.919650. PMID: 31672958. PMCID: PMC6857352.
Article6. Vivarelli M, Benedetti Cacciaguerra A, Lerut J, Lanari J, Conte G, Pravisan R, et al. 2020; Infrarenal versus supraceliac aorto-hepatic arterial revascularisation in adult liver transplantation: multicentre retrospective study. Updates Surg. 72:659–69. DOI: 10.1007/s13304-020-00839-x. PMID: 32594369.
Article7. Hummel R, Irmscher S, Schleicher C, Senninger N, Brockmann JG, Wolters HH. 2014; Aorto-hepatic bypass in liver transplantation in the MELD-era: outcomes after supraceliac and infrarenal bypasses. Surg Today. 44:626–32. DOI: 10.1007/s00595-013-0513-9. PMID: 23459787.
Article8. Bekker J, Ploem S, de Jong KP. 2009; Early hepatic artery thrombosis after liver transplantation: a systematic review of the incidence, outcome and risk factors. Am J Transplant. 9:746–57. DOI: 10.1111/j.1600-6143.2008.02541.x. PMID: 19298450.
Article9. Ikegami T, Kawasaki S, Hashikura Y, Miwa S, Kubota T, Mita A, et al. 2000; An alternative method of arterial reconstruction after hepatic arterial thrombosis following living-related liver transplantation. Transplantation. 69:1953–5. DOI: 10.1097/00007890-200005150-00036. PMID: 10830238.
Article10. Katz E, Fukuzawa K, Schwartz M, Mor E, Miller C. 1992; The splenic artery as the inflow in arterial revascularization of the liver graft in clinical liver transplantation. Transplantation. 53:1373–4. DOI: 10.1097/00007890-199206000-00041. PMID: 1376505.
Article11. Asakura T, Ohkohchi N, Orii T, Koyamada N, Satomi S. 2000; Arterial reconstruction using vein graft from the common iliac artery after hepatic artery thrombosis in living-related liver transplantation. Transplant Proc. 32:2250–1. DOI: 10.1016/S0041-1345(00)01787-5. PMID: 11120153.
Article12. Vogt PR, Zünd G, Lachat M, Turina MI. 1998; Regarding "early rupture and degeneration of cryopreserved arterial allografts". J Vasc Surg. 27:189–90. DOI: 10.1016/S0741-5214(98)70309-X.13. Bhatti AB, Dar FS, Qureshi AI, Haider S, Khan NA. 2019; Saphenous vein conduits for hepatic arterial reconstruction in living donor liver transplantation. Langenbecks Arch Surg. 404:293–300. DOI: 10.1007/s00423-019-01774-1. PMID: 30859361.
Article14. Li PC, Thorat A, Jeng LB, Yang HR, Li ML, Yeh CC, et al. 2017; Successful application of supraceliac aortohepatic conduit using saphenous venous graft in right Lobe living donor liver transplantation. Liver Transpl. 23:976–80. DOI: 10.1002/lt.24720. PMID: 28073174.
Article15. Baimakhanov Z, Magauina A, Matkerimov A, Kaniev S, Doskhanov M, Serikuly E, et al. 2019; Extra-anatomic jump graft arterial reconstruction using a great saphenous vein autograft during living donor liver transplantation. Transplant Proc. 51:3120–3. DOI: 10.1016/j.transproceed.2019.07.004. PMID: 31611118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Salvage aorto-hepatic jump graft for hepatic artery thrombosis following living donor liver transplantation: a case report with 10-year follow-up
- Hepatic Artery Reconstruction Using the Right Gastroepiploic Artery for Hepatic Artery Inflow in a Living Donor Liver Transplantation
- Variations in the origin of middle hepatic artery: a cadaveric study and implications for living donor liver transplantation
- Endovascular Exclusion of Hepatic Artery Pseudoaneurysm after Living-Donor Liver Transplantation with a Stent-Graft Using Conical Remodeling: A Case Report
- Successful Management of Splenic Artery Steal Syndrome after Living Donor Liver Transplantation