J Korean Med Sci.
2021 Dec;36(50):e334. 10.3346/jkms.2021.36.e334.
Assessment of Perioperative Atelectasis Using Lung Ultrasonography in Patients Undergoing Pneumoperitoneum Surgery in the Trendelenburg Position: Aspects of Differences according to Ventilatory Mode
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, College of medicine, Ewha Womans University, Seoul, Korea
- 3Department of Obstetrics and Gynecology, College of medicine, Ewha Womans University, Seoul, Korea
- KMID: 2523558
- DOI: http://doi.org/10.3346/jkms.2021.36.e334
Abstract
- Background
During robotic gynecologic pneumoperitoneum surgery in the Trendelenburg position, aeration loss leads to perioperative atelectasis. Recently developed ventilator mode pressure-controlled ventilation volume-guaranteed (PCV-VG) mode could provide adequate ventilation with lower inspiratory pressure compared to volume-controlled ventilation (VCV); we hypothesized that PCV-VG mode may be beneficial in reducing perioperative atelectasis via low tidal volume (VT ) of 6 mL/kg ventilation during robotic gynecologic pneumoperitoneum surgery in the Trendelenburg position. We applied lung ultrasound score (LUS) for detecting perioperative atelectasis. We aimed to compare perioperative atelectasis between VCV and PCV-VG with a low VT of 6 mL/kg during pneumoperitoneum surgery in the Trendelenburg position using LUS.
Methods
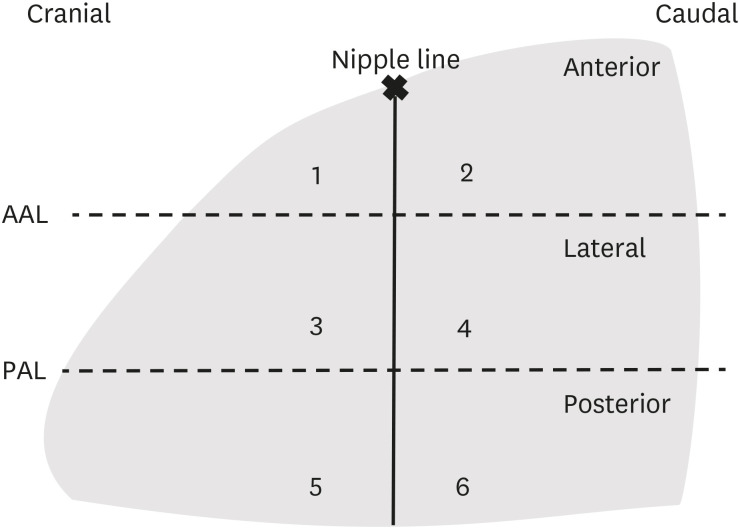
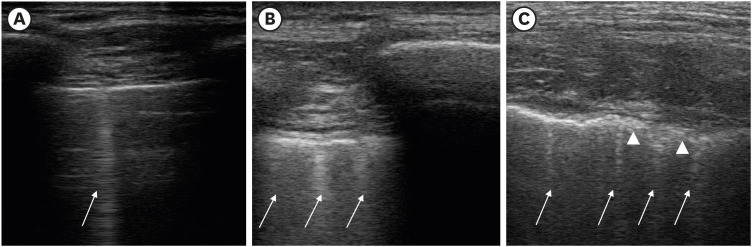
Patients scheduled for robotic gynecologic surgery were randomly allocated to the VCV (n = 41) or PCV-VG group (n = 41). LUS, ventilatory, and hemodynamic parameters were evaluated at T1 (before induction), T2 (10 minutes after induction in the supine position), T3 (10 minutes after desufflation of CO2 in the supine position), and T4 (30 minutes after emergence from anesthesia in the recovery room).
Results
Eighty patients (40 with PCV-VG and 40 with VCV) were included. Demographic data showed no significant differences between the groups. The total LUS has changed from baseline to T4, 0.63 (95% confidence interval [CI], 0.32, 0.94) to 1.77 (95% CI, 1.42, 2.21) in the VCV group and 0.86 (95% CI, 0.56, 1.16) to 1.43 (95% CI, 1.08, 1.78) in the PCV-VG group (P = 0.170). In both groups, total LUS increased significantly compared to the baseline values.
Conclusion
Using a low VT of 6 mL/kg during pneumoperitoneum surgery in the Trendelenburg position, our study showed no evidence that PCV-VG ventilation was superior to VCV in terms of perioperative atelectasis.
Figure
Reference
-
1. Ladha K, Vidal Melo MF, McLean DJ, Wanderer JP, Grabitz SD, Kurth T, et al. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ. 2015; 351:h3646. PMID: 26174419.
Article2. Cai H, Gong H, Zhang L, Wang Y, Tian Y. Effect of low tidal volume ventilation on atelectasis in patients during general anesthesia: a computed tomographic scan. J Clin Anesth. 2007; 19(2):125–129. PMID: 17379125.
Article3. Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. Accuracy of transthoracic lung ultrasound for diagnosing anesthesia-induced atelectasis in children. Anesthesiology. 2014; 120(6):1370–1379. PMID: 24662376.
Article4. Gainsburg DM. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012; 78(5):596–604. PMID: 22415437.5. Andersson LE, Bååth M, Thörne A, Aspelin P, Odeberg-Wernerman S. Effect of carbon dioxide pneumoperitoneum on development of atelectasis during anesthesia, examined by spiral computed tomography. Anesthesiology. 2005; 102(2):293–299. PMID: 15681942.
Article6. Restrepo RD, Braverman J. Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis. Expert Rev Respir Med. 2015; 9(1):97–107. PMID: 25541220.
Article7. Duggan M, Kavanagh BP, Warltier DC. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005; 102(4):838–854. PMID: 15791115.8. Güldner A, Kiss T, Serpa Neto A, Hemmes SN, Canet J, Spieth PM, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015; 123(3):692–713. PMID: 26120769.9. Schick V, Dusse F, Eckardt R, Kerkhoff S, Commotio S, Hinkelbein J, et al. Comparison of volume-guaranteed or -targeted, pressure-controlled ventilation with volume-controlled ventilation during elective surgery: a systematic review and meta-analysis. J Clin Med. 2021; 10(6):1276. PMID: 33808607.
Article10. Choi EM, Na S, Choi SH, An J, Rha KH, Oh YJ. Comparison of volume-controlled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth. 2011; 23(3):183–188. PMID: 21377341.
Article11. Lee JM, Lee SK, Rhim CC, Seo KH, Han M, Kim SY, et al. Comparison of volume-controlled, pressure-controlled, and pressure-controlled volume-guaranteed ventilation during robot-assisted laparoscopic gynecologic surgery in the Trendelenburg position. Int J Med Sci. 2020; 17(17):2728–2734. PMID: 33162800.
Article12. Assad OM, El Sayed AA, Khalil MA. Comparison of volume-controlled ventilation and pressure-controlled ventilation volume guaranteed during laparoscopic surgery in Trendelenburg position. J Clin Anesth. 2016; 34:55–61. PMID: 27687346.
Article13. Balick-Weber CC, Nicolas P, Hedreville-Montout M, Blanchet P, Stéphan F. Respiratory and haemodynamic effects of volume-controlled vs pressure-controlled ventilation during laparoscopy: a cross-over study with echocardiographic assessment. Br J Anaesth. 2007; 99(3):429–435. PMID: 17626027.
Article14. Park JH, Park IK, Choi SH, Eum D, Kim MS. Volume-controlled versus dual-controlled ventilation during robot-assisted laparoscopic prostatectomy with steep trendelenburg position: a randomized-controlled trial. J Clin Med. 2019; 8(12):E2032. PMID: 31766358.
Article15. Bouhemad B, Mongodi S, Via G, Rouquette I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology. 2015; 122(2):437–447. PMID: 25501898.
Article16. Yu X, Zhai Z, Zhao Y, Zhu Z, Tong J, Yan J, et al. Performance of lung ultrasound in detecting peri-operative atelectasis after general anesthesia. Ultrasound Med Biol. 2016; 42(12):2775–2784. PMID: 27639431.
Article17. Monastesse A, Girard F, Massicotte N, Chartrand-Lefebvre C, Girard M. Lung ultrasonography for the assessment of perioperative atelectasis: a pilot feasibility study. Anesth Analg. 2017; 124(2):494–504. PMID: 27669555.18. El-Khatib MF, Jamaleddine GW. A new oxygenation index for reflecting intrapulmonary shunting in patients undergoing open-heart surgery. Chest. 2004; 125(2):592–596. PMID: 14769743.
Article19. Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38(4):577–591. PMID: 22392031.
Article20. Kim YS, Won YJ, Lee DK, Lim BG, Kim H, Lee IO, et al. Lung ultrasound score-based perioperative assessment of pressure-controlled ventilation-volume guaranteed or volume-controlled ventilation in geriatrics: a prospective randomized controlled trial. Clin Interv Aging. 2019; 14:1319–1329. PMID: 31409981.21. Valenza F, Chevallard G, Fossali T, Salice V, Pizzocri M, Gattinoni L. Management of mechanical ventilation during laparoscopic surgery. Best Pract Res Clin Anaesthesiol. 2010; 24(2):227–241. PMID: 20608559.
Article22. Cinnella G, Grasso S, Spadaro S, Rauseo M, Mirabella L, Salatto P, et al. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2013; 118(1):114–122. PMID: 23196259.
Article23. Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RR, et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019; 123(6):898–913. PMID: 31587835.
Article24. Lian M, Zhao X, Wang H, Chen L, Li S. Respiratory dynamics and dead space to tidal volume ratio of volume-controlled versus pressure-controlled ventilation during prolonged gynecological laparoscopic surgery. Surg Endosc. 2017; 31(9):3605–3613. PMID: 28039643.
Article25. Toker MK, Altıparmak B, Uysal AI, Demirbilek SG. Comparison of pressure-controlled volume-guaranteed ventilation and volume-controlled ventilation in obese patients during gynecologic laparoscopic surgery in the Trendelenburg position. Braz J Anesthesiol. 2019; 69(6):553–560. PMID: 31836201.
Article26. Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, et al. Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and Volume-Limited Ventilation Strategy Group. N Engl J Med. 1998; 338(6):355–361. PMID: 9449728.27. Jiang J, Li B, Kang N, Wu A, Yue Y. Pressure-controlled versus volume-controlled ventilation for surgical patients: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2016; 30(2):501–514. PMID: 26395394.
Article28. Ahn HJ, Park M, Kim JA, Yang M, Yoon S, Kim BR, et al. Driving pressure guided ventilation. Korean J Anesthesiol. 2020; 73(3):194–204. PMID: 32098009.
Article29. Rozé H, Lafargue M, Batoz H, Picat MQ, Perez P, Ouattara A, et al. Pressure-controlled ventilation and intrabronchial pressure during one-lung ventilation. Br J Anaesth. 2010; 105(3):377–381. PMID: 20554634.30. Kim MS, Kim NY, Lee KY, Choi YD, Hong JH, Bai SJ. The impact of two different inspiratory to expiratory ratios (1:1 and 1:2) on respiratory mechanics and oxygenation during volume-controlled ventilation in robot-assisted laparoscopic radical prostatectomy: a randomized controlled trial. Can J Anaesth. 2015; 62(9):979–987. PMID: 25869025.
Article31. Marini JJ, Ravenscraft SA. Mean airway pressure: physiologic determinants and clinical importance--part 2: clinical implications. Crit Care Med. 1992; 20(11):1604–1616. PMID: 1424706.32. Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014; 12(1):25. PMID: 24993976.
Article33. Mongodi S, Bouhemad B, Orlando A, Stella A, Tavazzi G, Via G, et al. Modified lung ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med. 2017; 38(5):530–537. PMID: 28291991.
Article34. Cho S, Oh HW, Choi MH, Lee HJ, Woo JH. Effects of intraoperative ventilation strategy on perioperative atelectasis assessed by lung ultrasonography in patients undergoing open abdominal surgery: a prospective randomized controlled study. J Korean Med Sci. 2020; 35(39):e327. PMID: 33045769.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery
- Arterial to end-tidal carbon dioxide pressure gradient increases with age in the steep Trendelenburg position with pneumoperitoneum
- The effect of Trendelenburg position and pneumoperitoneum on regional cerebral oxygen saturation during gynecological laparoscopic surgery
- Position does not affect the optic nerve sheath diameter during laparoscopy
- The Effect of the Body Position and CO2 Gas Insufflation on Airway Pressure and Compliance in Normal Subjects during Laparoscopy or Pelviscopy