J Korean Foot Ankle Soc.
2021 Dec;25(4):149-156. 10.14193/jkfas.2021.25.4.149.
Current Trends in the Treatment of Osteochondral Lesion of the Talus: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungbuk National University Hospital, Cheongju, Korea
- 2Department of Orthopedic Surgery, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea
- 3Department of Foot and Ankle Surgery, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 4Department of Orthopedic Surgery, Seoul National University Hospital, Seoul, Korea
- 5Department of Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, Korea
- KMID: 2523295
- DOI: http://doi.org/10.14193/jkfas.2021.25.4.149
Abstract
- Purpose
Given the lack of definite evidence-based guidelines in clinical practice, there may be a wide variation in treatment protocols for osteochondral lesions of the talus (OLT). Based on the Korean Foot and Ankle Society (KFAS) member survey, this study aimed to report the current trends in the management of OLT.
Materials and Methods
A web-based questionnaire containing 30 questions was sent to all KFAS members in September 2021. The questions were mainly related to clinical experience and preferences in diagnosis, conservative, and surgical treatments for patients with OLT. Answers with a prevalence of ≥50% of respondents were considered a tendency.
Results
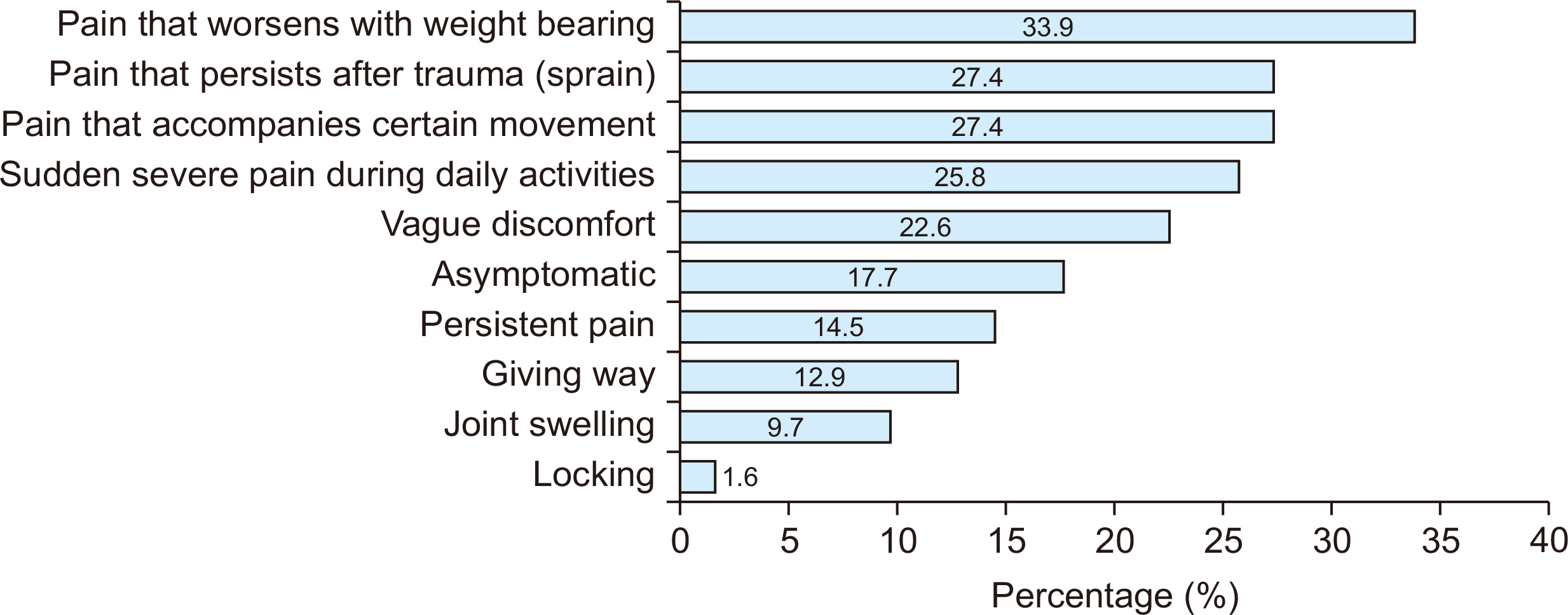
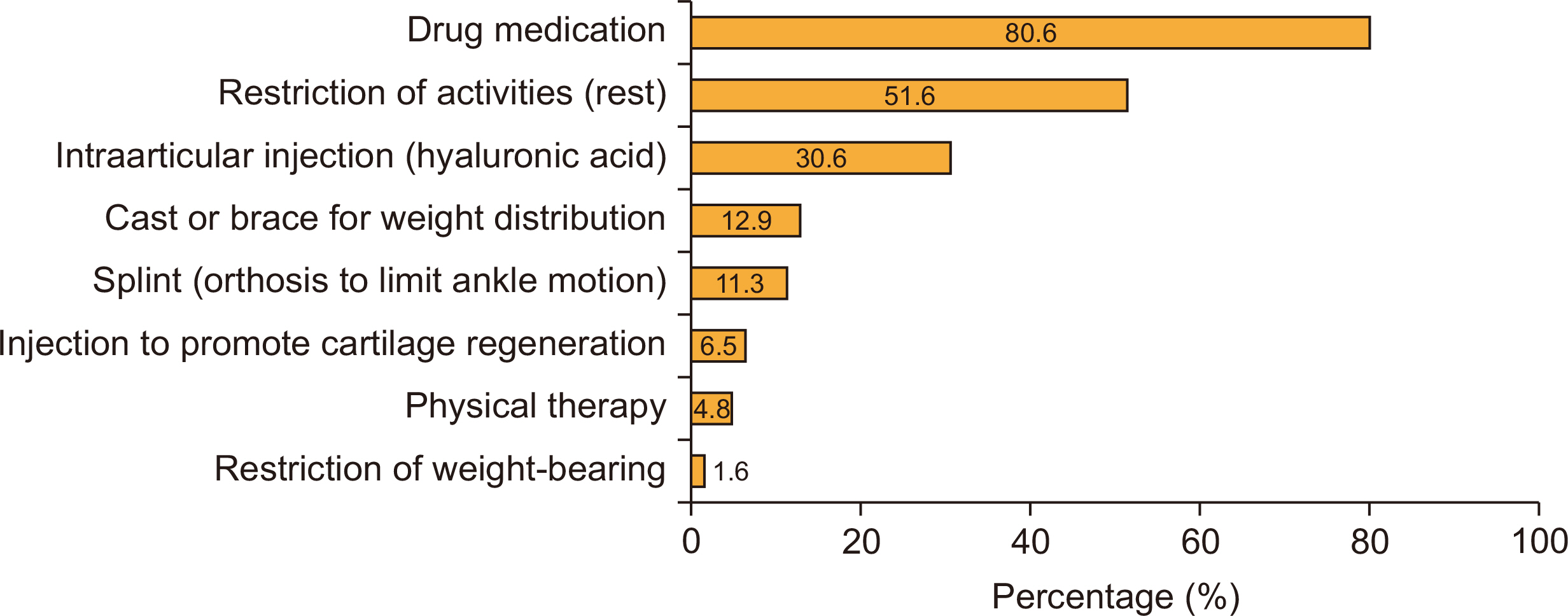
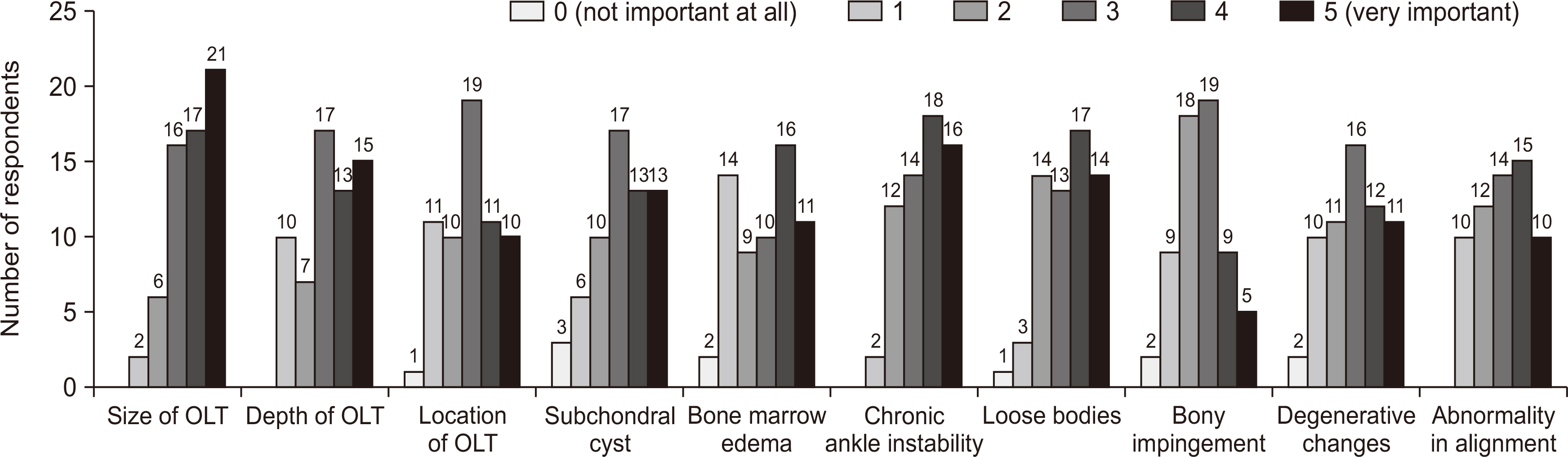
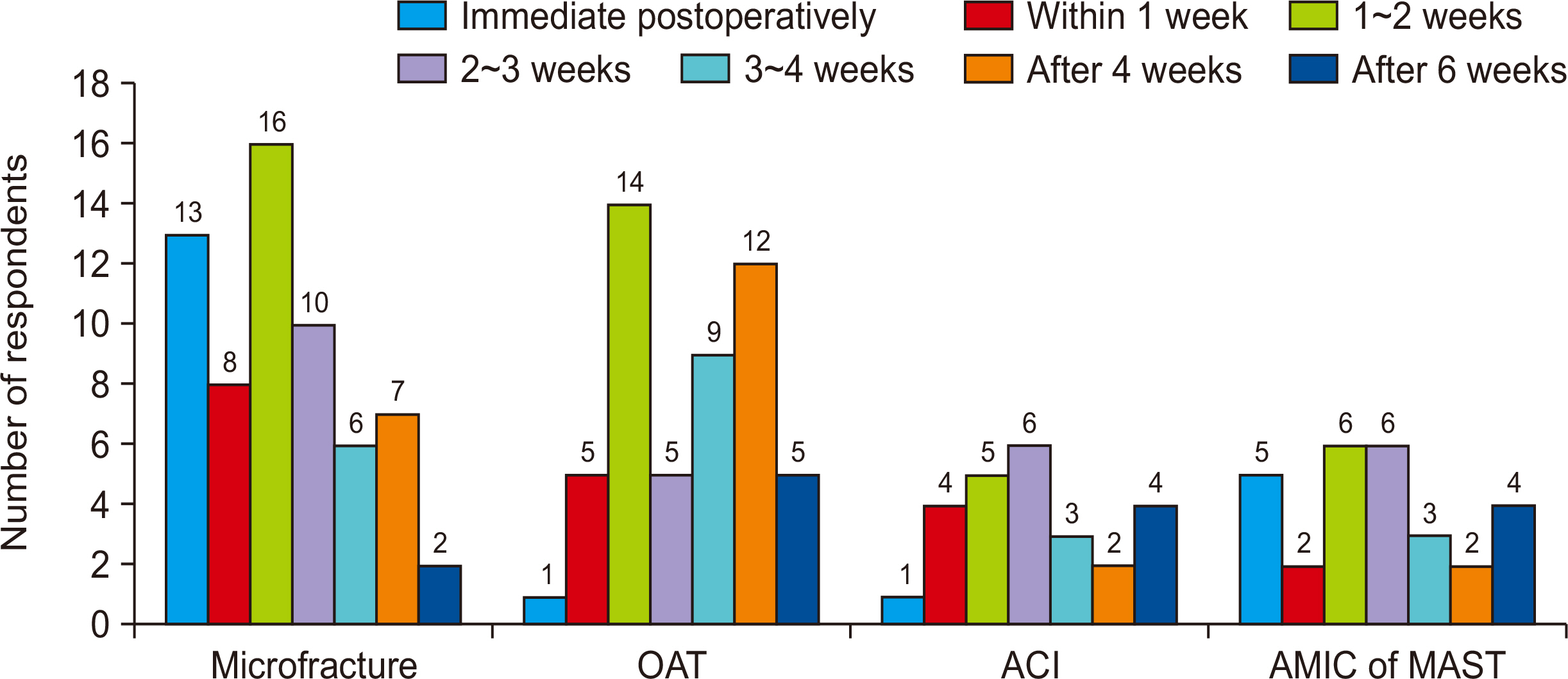
Sixty-two (11.3%) of the 550 surgeons queried responded to the survey. The responses to 9 (30.0%) of the total of 30 questions established a tendency. Answers exhibiting a tendency were as follows; additional diagnostic tools except for plain radiograph (magnetic resonance imaging), most common conservative treatment method (oral medication, rest), most important radiological factor in decision making for surgical treatment and method (size of the lesion, ankle instability, loose bodies), most important patient factors in decision making for surgical treatment and method (age, activity or occupation), infrequently requiring posterior arthroscopy (less than 3%), most common revision surgery for failed bone marrow stimulation procedure (osteochondral autograft transplantation [OAT]), not requiring additional procedure for donor site in OAT, the main reason for unsatisfactory result after OAT (persistent pain without radiological abnormality), no generalization of autologous chondrocyte implantation or chondrogenesis using stem cells.
Conclusion
This study presents updated information on current trends in the management of OLT in Korea. Both consensus and variations in the approach to patients with OLT were revealed through this survey. Since recent biologic efforts to regenerate cartilage have been unsuccessful, further studies to identify clinical evidence would be needed.
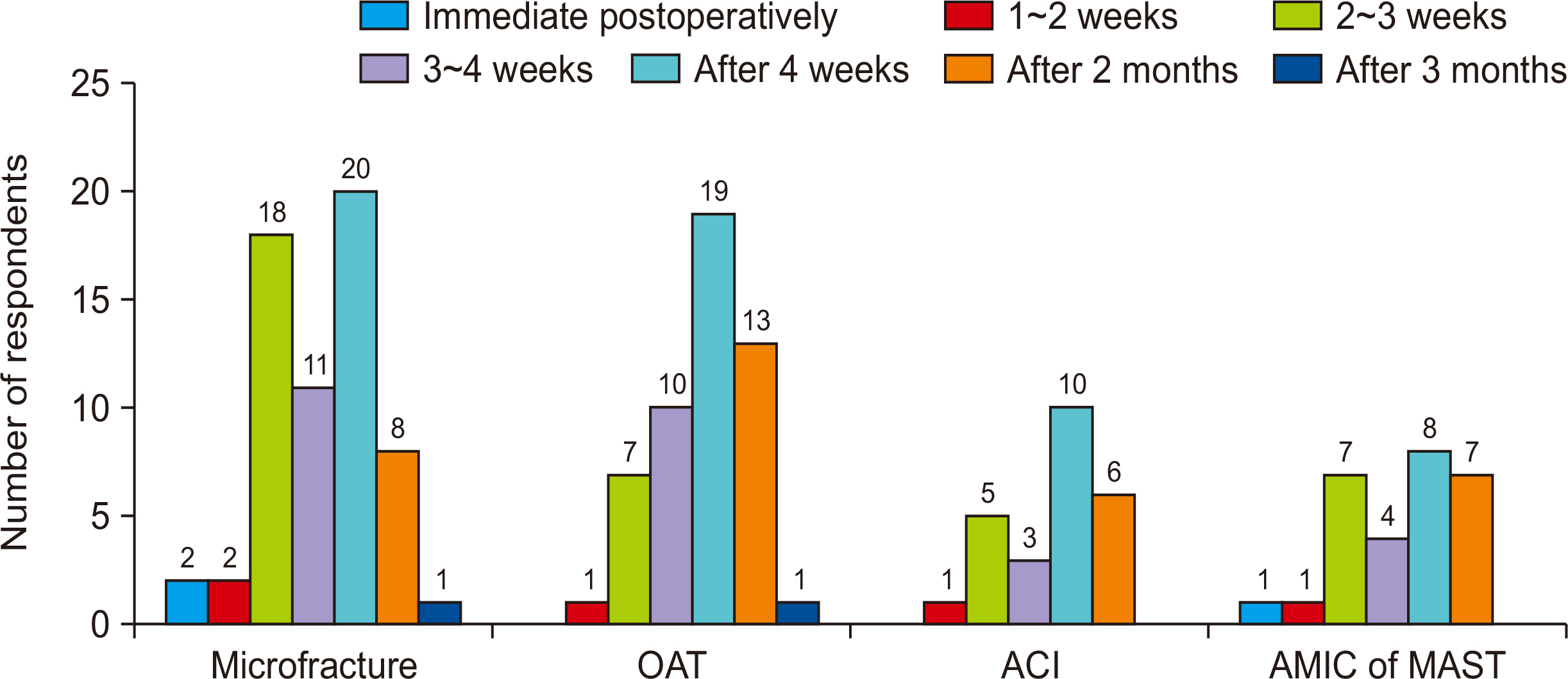
Figure
Reference
-
1. O'Loughlin PF, Heyworth BE, Kennedy JG. 2010; Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 38:392–404. doi: 10.1177/0363546509336336. DOI: 10.1177/0363546509336336. PMID: 19561175.2. McGahan PJ, Pinney SJ. 2010; Current concept review: osteochondral lesions of the talus. Foot Ankle Int. 31:90–101. doi: 10.3113/FAI.2010.0090. DOI: 10.3113/FAI.2010.0090. PMID: 20067729.
Article3. Gianakos AL, Yasui Y, Hannon CP, Kennedy JG. 2017; Current management of talar osteochondral lesions. World J Orthop. 8:12–20. doi: 10.5312/wjo.v8.i1.12. DOI: 10.5312/wjo.v8.i1.12. PMID: 28144574. PMCID: PMC5241540.
Article4. Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014; 96-B:164–71. doi: 10.1302/0301-620X.96B2.31637. DOI: 10.1302/0301-620X.96B2.31637. PMID: 24493179.5. Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN. 2006; Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin. 11:331–59. vidoi: 10.1016/j.fcl.2006.03.008. DOI: 10.1016/j.fcl.2006.03.008. PMID: 16798515.
Article6. Dekker TJ, Dekker PK, Tainter DM, Easley ME, Adams SB. 2017; Treatment of osteochondral lesions of the talus: a critical analysis review. JBJS Rev. 5:e4. doi: 10.2106/JBJS.RVW.16.00065. DOI: 10.2106/JBJS.RVW.16.00065. PMID: 28359070.7. Guney A, Yurdakul E, Karaman I, Bilal O, Kafadar IH, Oner M. 2016; Medium-term outcomes of mosaicplasty versus arthroscopic microfracture with or without platelet-rich plasma in the treatment of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 24:1293–8. doi: 10.1007/s00167-015-3834-y. DOI: 10.1007/s00167-015-3834-y. PMID: 26493549.
Article8. Hannon CP, Ross KA, Murawski CD, Deyer TW, Smyth NA, Hogan MV, et al. 2016; Arthroscopic bone marrow stimulation and concentrated bone marrow aspirate for osteochondral lesions of the talus: a case-control study of functional and magnetic resonance observation of cartilage repair tissue outcomes. Arthroscopy. 32:339–47. doi: 10.1016/j.arthro.2015.07.012. DOI: 10.1016/j.arthro.2015.07.012. PMID: 26395409.
Article9. Tan H, Li A, Qiu X, Cui Y, Tang W, Wang G, et al. 2021; Operative treatments for osteochondral lesions of the talus in adults: a systematic review and meta-analysis. Medicine (Baltimore). 100:e26330. doi: 10.1097/MD.0000000000026330. DOI: 10.1097/MD.0000000000026330. PMID: 34160396. PMCID: PMC8238309.10. Guelfi M, DiGiovanni CW, Calder J, Malagelada F, Cordier G, Takao M, et al. 2021; Large variation in management of talar osteochondral lesions among foot and ankle surgeons: results from an international survey. Knee Surg Sports Traumatol Arthrosc. 29:1593–603. doi: 10.1007/s00167-020-06370-1. DOI: 10.1007/s00167-020-06370-1. PMID: 33221934.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Autologous Osteochondral Transplantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Redomicrofracture as a Treatment for Osteochondral Lesion of Talus after the Failure of Arthroscopic Microfracture
- Autologous Chondrocyte Implantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey