Development of the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) Scale for Assessing Work-related Stress and Anxiety in Healthcare Workers in Response to Viral Epidemics
- Affiliations
-
- 1Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Division of Psychiatry, Health Screening and Promotion Center, Asan Medical Center, Seoul, Korea
- 4Department of Psychology, Sungshin Women's University, Seoul, Korea
- KMID: 2523239
- DOI: http://doi.org/10.3346/jkms.2021.36.e319
Abstract
- Background
The coronavirus disease 2019, or COVID-19, has had a major psychological impact on healthcare workers. However, very few scales are available to specifically assess work-related stress and anxiety in healthcare workers responding to a viral epidemic. This study developed a new assessment tool, the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) and aimed to validate it among healthcare workers directly affected by COVID-19 in Korea.
Methods
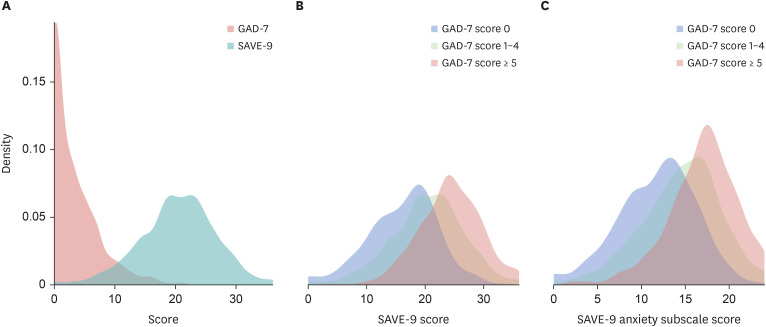
A total of 1,019 healthcare workers responded through anonymous questionnaires during April 20–30, 2020. Exploratory factor analysis (EFA) was conducted to explore the construct validity, and the reliability was assessed using internal consistency measures of Cronbach's alpha coefficients. Receiver operating characteristic analysis was conducted to define the most appropriate cut-off point of SAVE-9 using the Generalized Anxiety Disorder-7 scale (GAD-7; ≥ 5). Second, Spearman's rank correlation coefficient was used to establish convergent validity for the SAVE-9 questionnaire with GAD-7 and the Patient Health Questionnaire-9.
Results
The nine-item scale had satisfactory internal consistency (Cronbach's α = 0.795). It adopted a two-factor structure: 1) anxiety regarding viral epidemics and 2) work-related stress associated with viral epidemics. A cut-off score of 22 for the SAVE-9 ascertained levels of stress and anxiety in response to a viral epidemic in healthcare workers that warranted clinical attention. Correlations between the SAVE-9 and the other scales were statistically significant (P < 0.05).
Conclusion
The results suggest that the SAVE-9 is a useful, reliable, and valid tool to evaluate stress and anxiety responses in healthcare workers during viral epidemics.
Keyword
Figure
Cited by 3 articles
-
How COVID-19 Affected Healthcare Workers in the Hospital Locked Down due to Early COVID-19 Cases in Korea
Hyeon-Ah Lee, Myung Hee Ahn, Seonjeong Byun, Hae-Kook Lee, Yong-Sil Kweon, Seockhoon Chung, Yong-Wook Shin, Kyoung-Uk Lee
J Korean Med Sci. 2021;36(47):e325. doi: 10.3346/jkms.2021.36.e325.Adherence to Physical Distancing and Health Beliefs About COVID-19 Among Patients With Cancer
Sajida Fawaz Hammoudi, Oli Ahmed, Hoyoung An, Youjin Hong, Myung Hee Ahn, Seockhoon Chung
J Korean Med Sci. 2023;38(43):e336. doi: 10.3346/jkms.2023.38.e336.Mediating Role of Viral Anxiety and Insomnia in Relationship Between Work-Related Stress and Depression Among Cold Chain Workers During COVID-19 Pandemic
Du Xinjie, He Runlian, Oli Ahmed, Eulah Cho, Seockhoon Chung
J Korean Med Sci. 2023;38(43):e338. doi: 10.3346/jkms.2023.38.e338.
Reference
-
1. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020; 395(10223):514–523. PMID: 31986261.
Article2. Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004; 170(5):793–798. PMID: 14993174.
Article3. Zhou Y, Wang W, Sun Y, Qian W, Liu Z, Wang R, et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: Workload should be concerned. J Affect Disord. 2020; 277:510–514. PMID: 32882508.
Article4. Guo WP, Min Q, Gu WW, Yu L, Xiao X, Yi WB, et al. Prevalence of mental health problems in frontline healthcare workers after the first outbreak of COVID-19 in China: a cross-sectional study. Health Qual Life Outcomes. 2021; 19(1):103. PMID: 33752686.
Article5. Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiatr. 2020; 33(5):e100284. PMID: 34192235.
Article6. Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. 2004; 359(1447):1117–1125. PMID: 15306398.
Article7. Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004; 185(2):127–133. PMID: 15286063.
Article8. Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018; 87:123–127. PMID: 30343247.
Article9. An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020; 276:312–315. PMID: 32871661.
Article10. Anmella G, Fico G, Roca A, Gómez-Ramiro M, Vázquez M, Murru A, et al. Unravelling potential severe psychiatric repercussions on healthcare professionals during the COVID-19 crisis. J Affect Disord. 2020; 273:422–424. PMID: 32425275.
Article11. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2021; 126:252–264. PMID: 33774085.
Article12. Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016; 14(1):7–14. PMID: 26847480.
Article13. Hagino C. A brief overview of the development process for written, self-report, health-related surveys. J Can Chiropr Assoc. 2002; 46(1):11–21.14. Kim JS, Choi JS. Factors influencing emergency nurses' burnout during an outbreak of Middle East respiratory syndrome coronavirus in Korea. Asian Nurs Res. 2016; 10(4):295–299.
Article15. Park JS, Lee EH, Park NR, Choi YH. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: a cross-sectional study. Arch Psychiatr Nurs. 2018; 32(1):2–6. PMID: 29413067.
Article16. Lehmann M, Bruenahl CA, Löwe B, Addo MM, Schmiedel S, Lohse AW, et al. Ebola and psychological stress of health care professionals. Emerg Infect Dis. 2015; 21(5):913–914. PMID: 25897490.
Article17. Ji D, Ji YJ, Duan XZ, Li WG, Sun ZQ, Song XA, et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014–2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. 2017; 8(8):12784–12791. PMID: 28061463.
Article18. Cénat JM, Balayulu-Makila O, Derivois D, Felix N, Mukunzi JN, Bukaka J, et al. The mental health professional at the feet of the Ebola virus: individual treatment and global mental challenges. Br J Psychiatry. 2019; 215(4):577–578.
Article19. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009; 54(5):302–311. PMID: 19497162.
Article20. Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006; 12(12):1924–1932. PMID: 17326946.
Article21. Chua SE, Cheung V, Cheung C, McAlonan GM, Wong JW, Cheung EP, et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004; 49(6):391–393. PMID: 15283534.
Article22. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.23. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166(10):1092–1097. PMID: 16717171.24. Gravetter F, Wallnau L. Essentials of Statistics for the Behavioral Sciences. 8th ed. Wadsworth, OH, USA: Cengage Learning;2014.25. Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018; 60(3):248–257. PMID: 29252922.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessing Stress and Anxiety in Firefighters During the Coronavirus Disease-2019 Pandemic: A Comparative Adaptation of the Stress and Anxiety in the Viral Epidemic–9 Items and Stress and Anxiety in the Viral Epidemics–6 Items Scales
- Resilience and Work-Related Stress May Affect Depressive Symptoms in Nursing Professionals during the COVID-19 Pandemic Era
- Factorial Validity of the Arabic Version of the Stress and Anxiety to Viral Epidemics-6 Items (SAVE-6) Scale among the General Population in Lebanon
- Application of Stress and Anxiety to Viral Epidemics-6 to Measure the Anxiety Response of Cold Chain Practitioners During the COVID-19 Post-Pandemic Era in China
- Mediating Role of Viral Anxiety and Insomnia in Relationship Between Work-Related Stress and Depression Among Cold Chain Workers During COVID-19 Pandemic