Ann Hepatobiliary Pancreat Surg.
2021 Nov;25(4):536-543. 10.14701/ahbps.2021.25.4.536.
Patch venoplasty for resecting tumor invading the retrohepatic inferior vena cava using total and selective hepatic vascular exclusion
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2523060
- DOI: http://doi.org/10.14701/ahbps.2021.25.4.536
Abstract
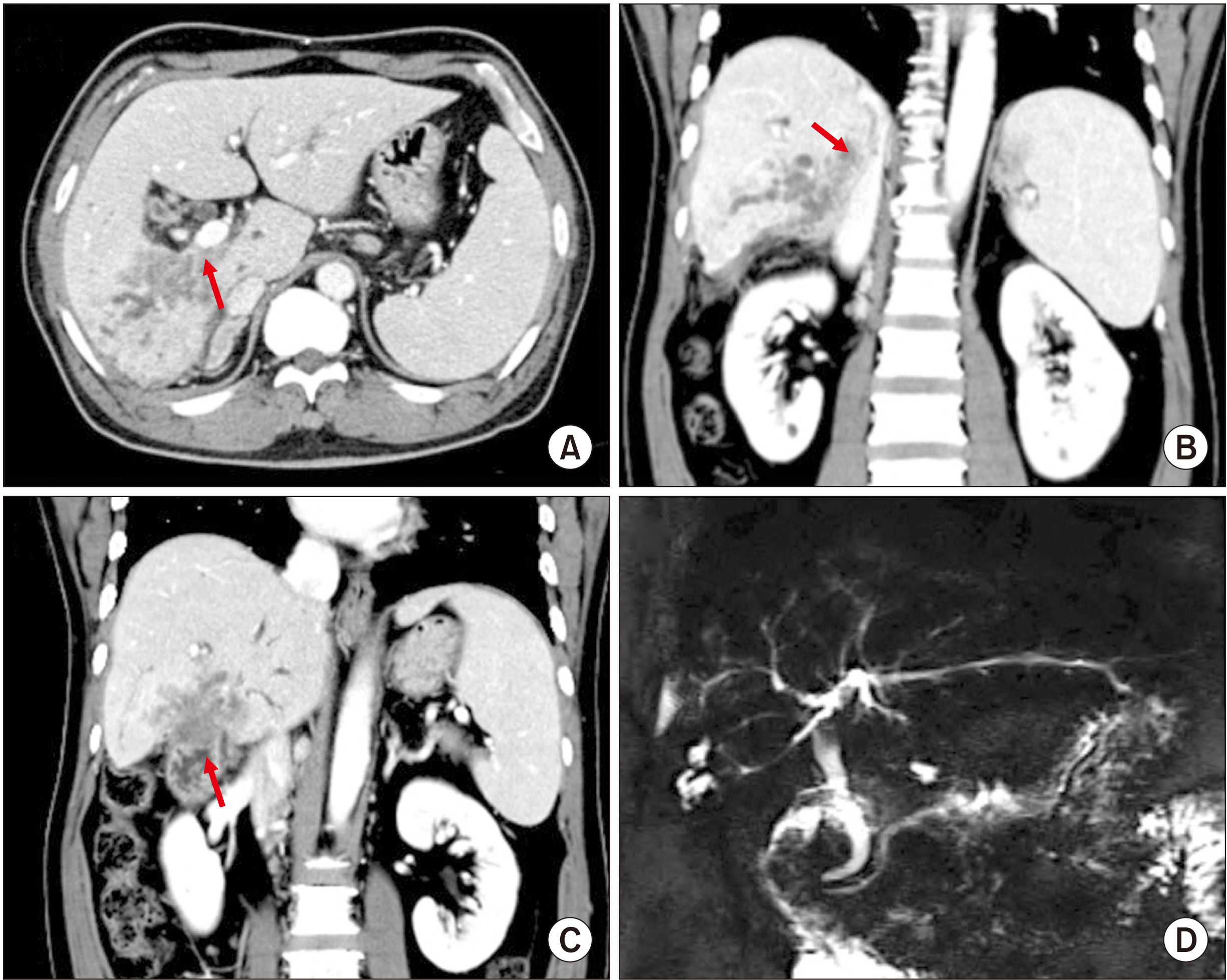
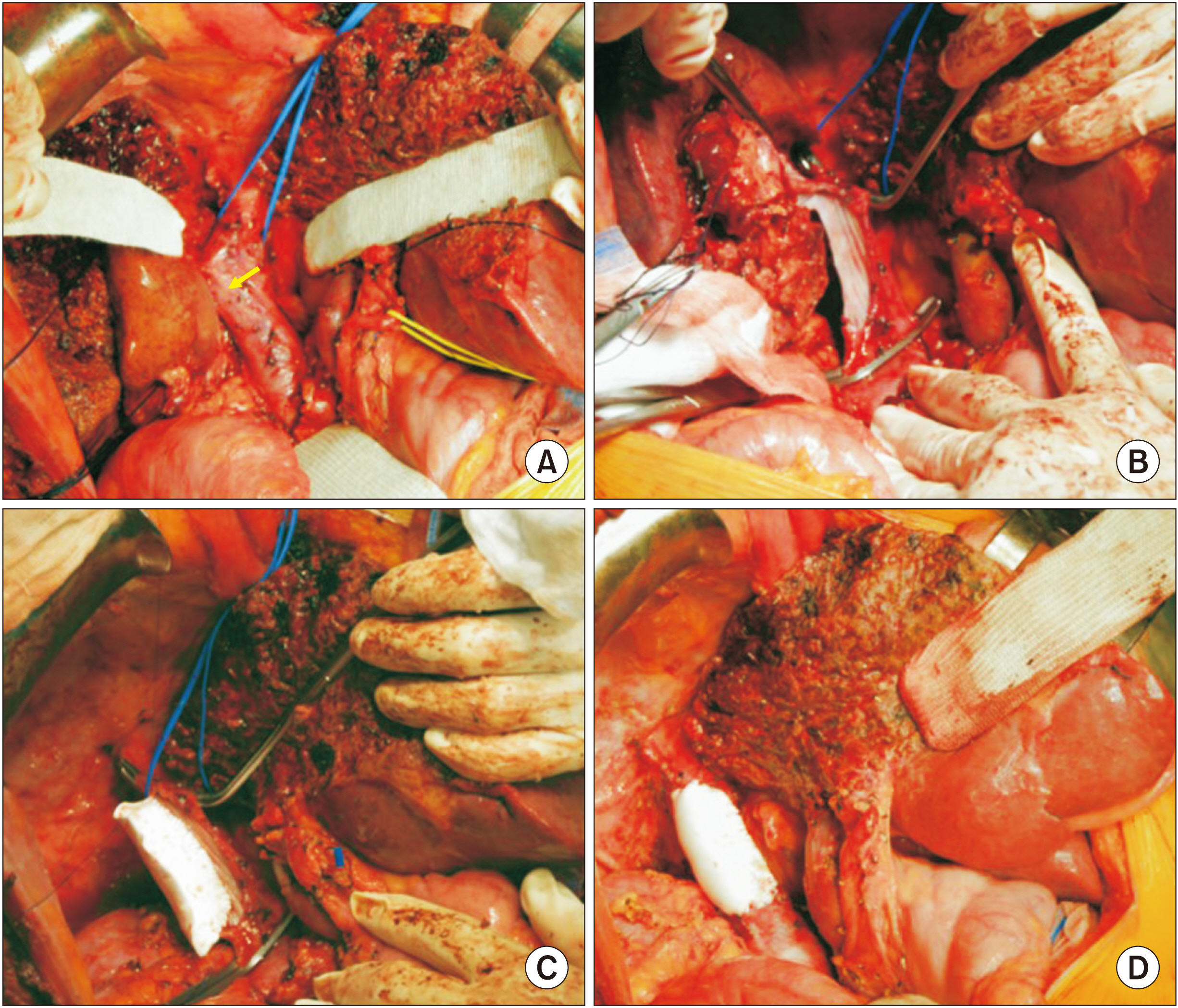
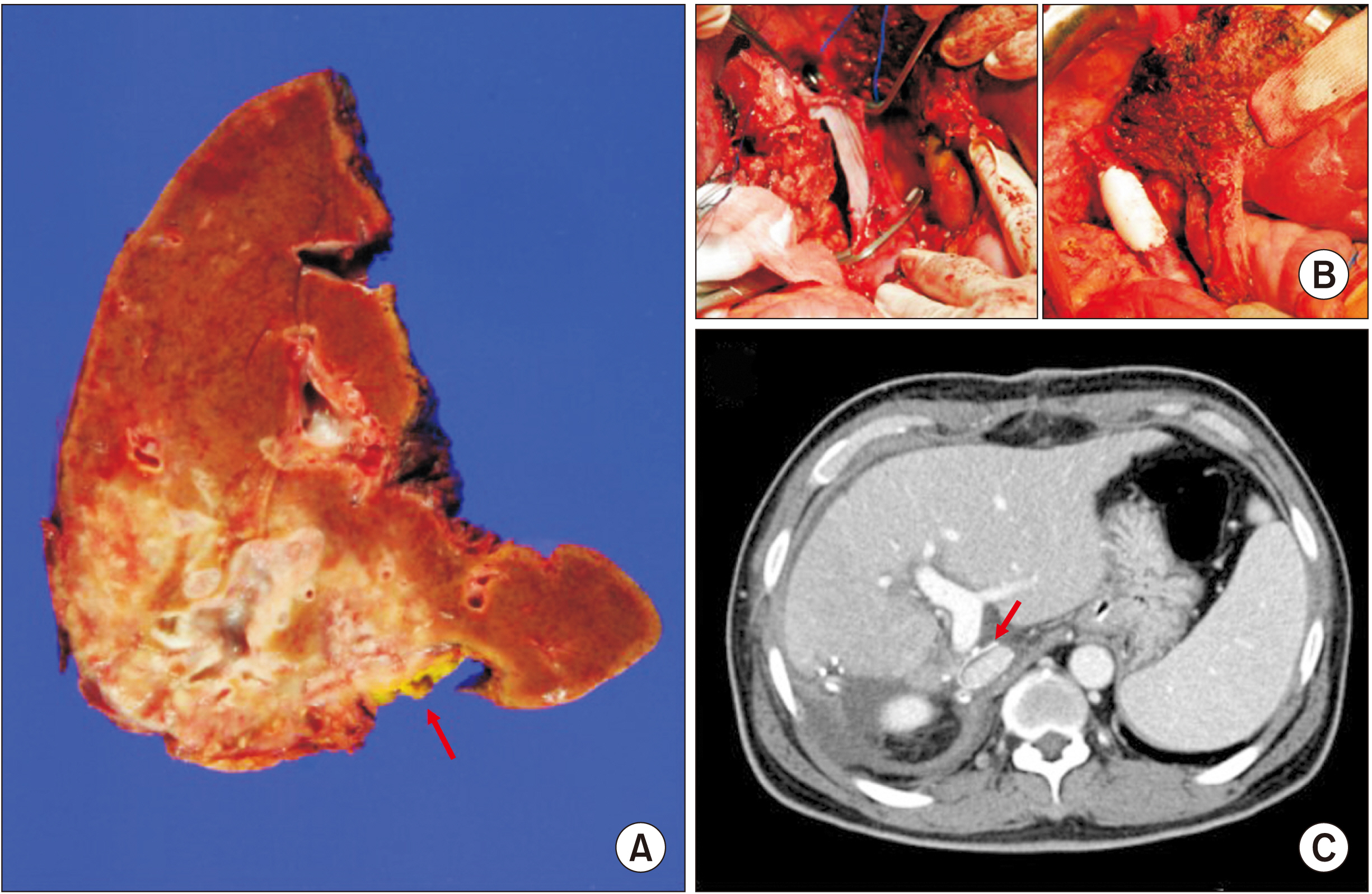
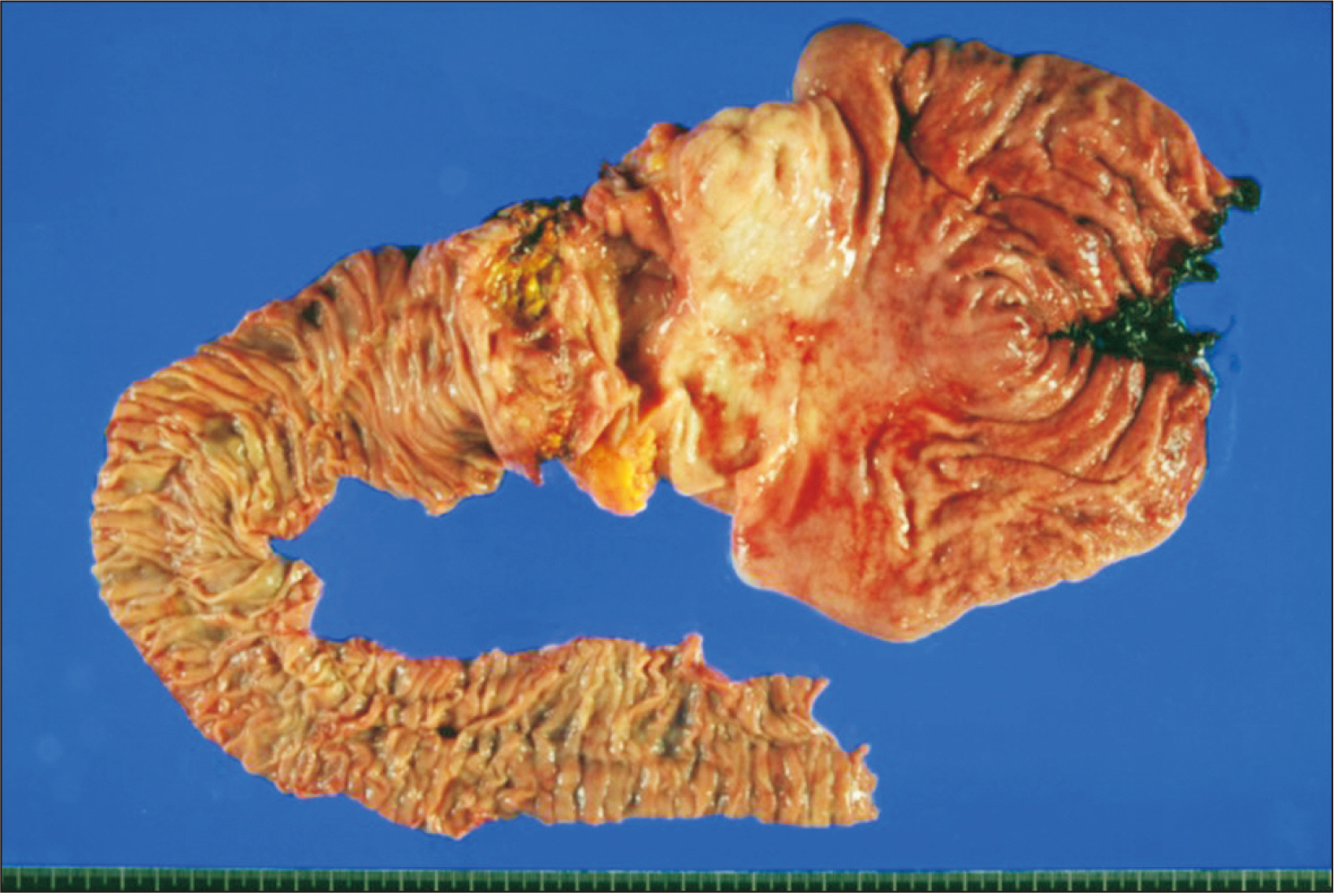
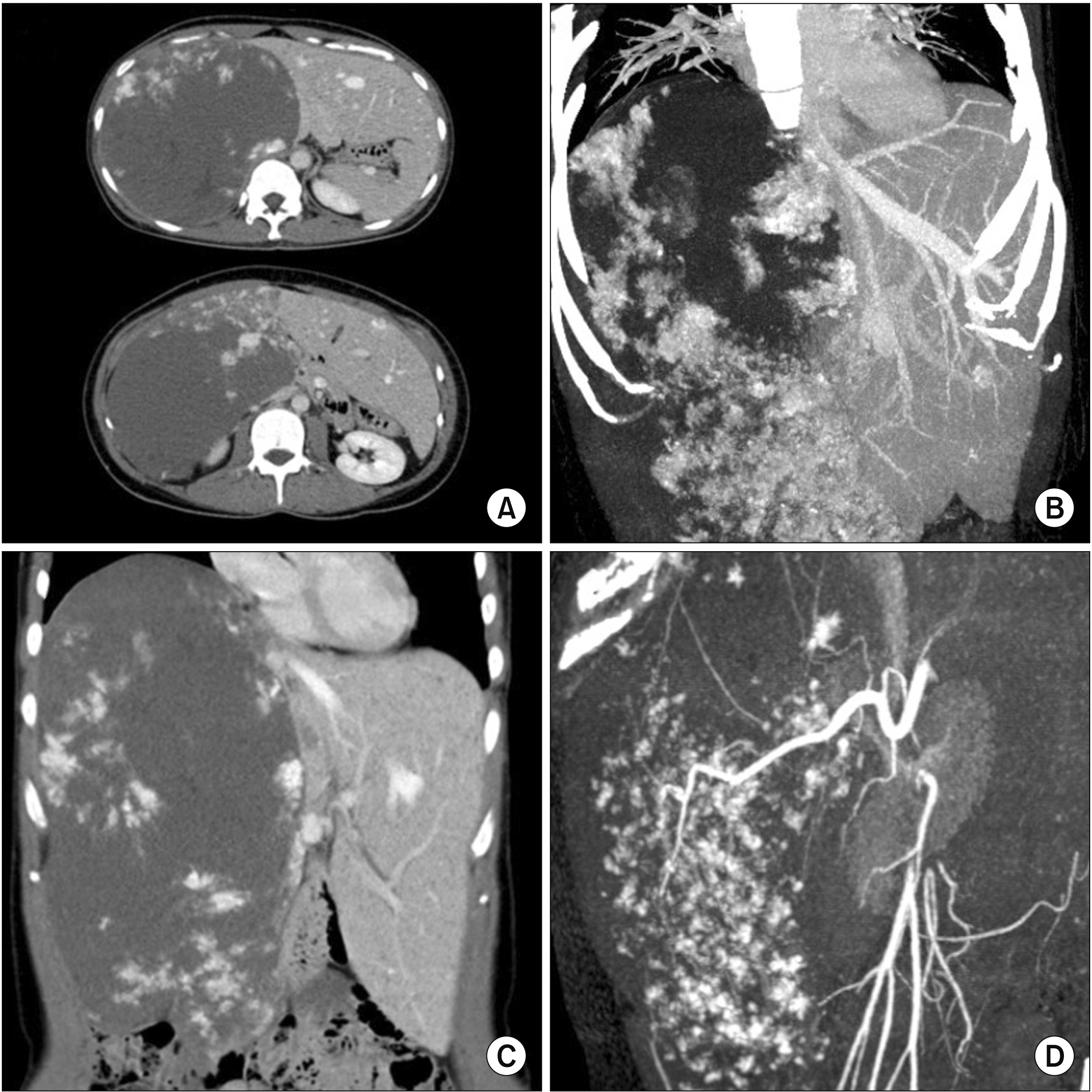
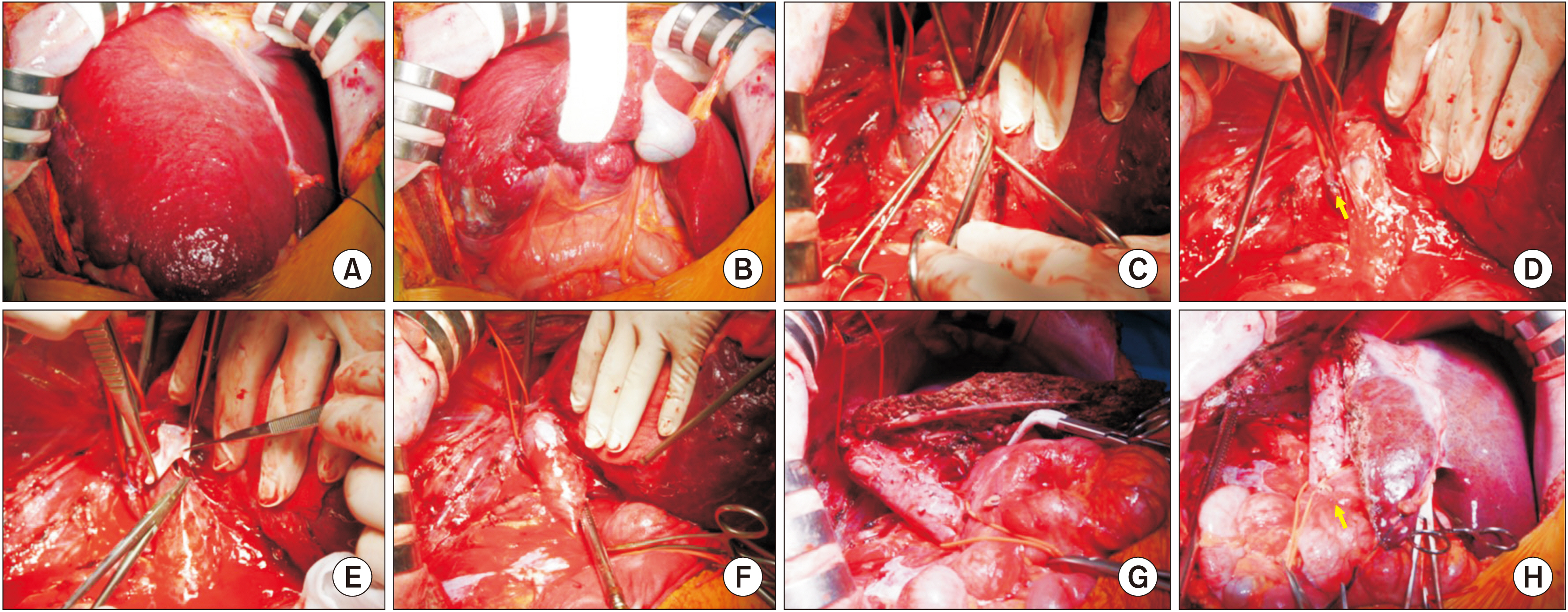
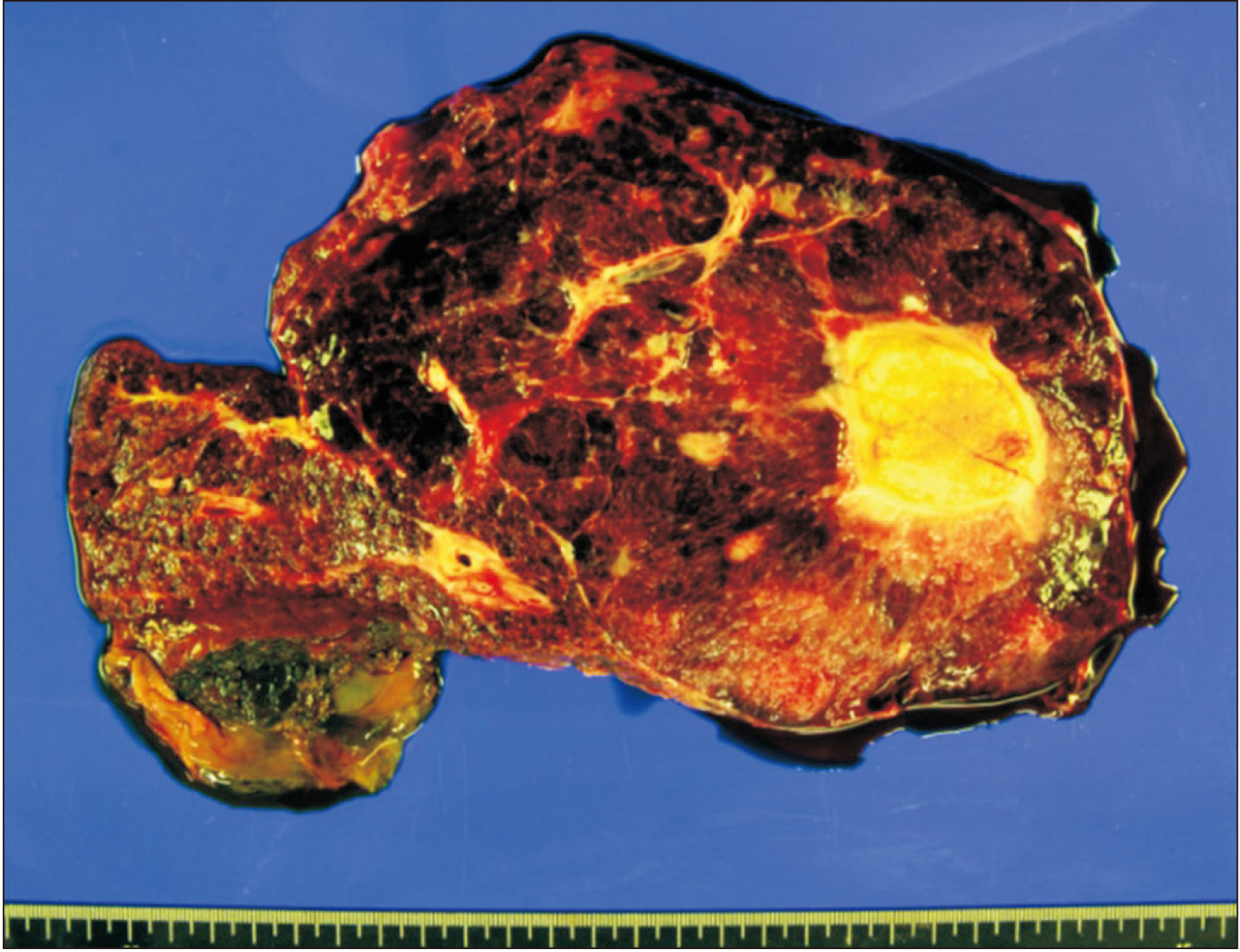
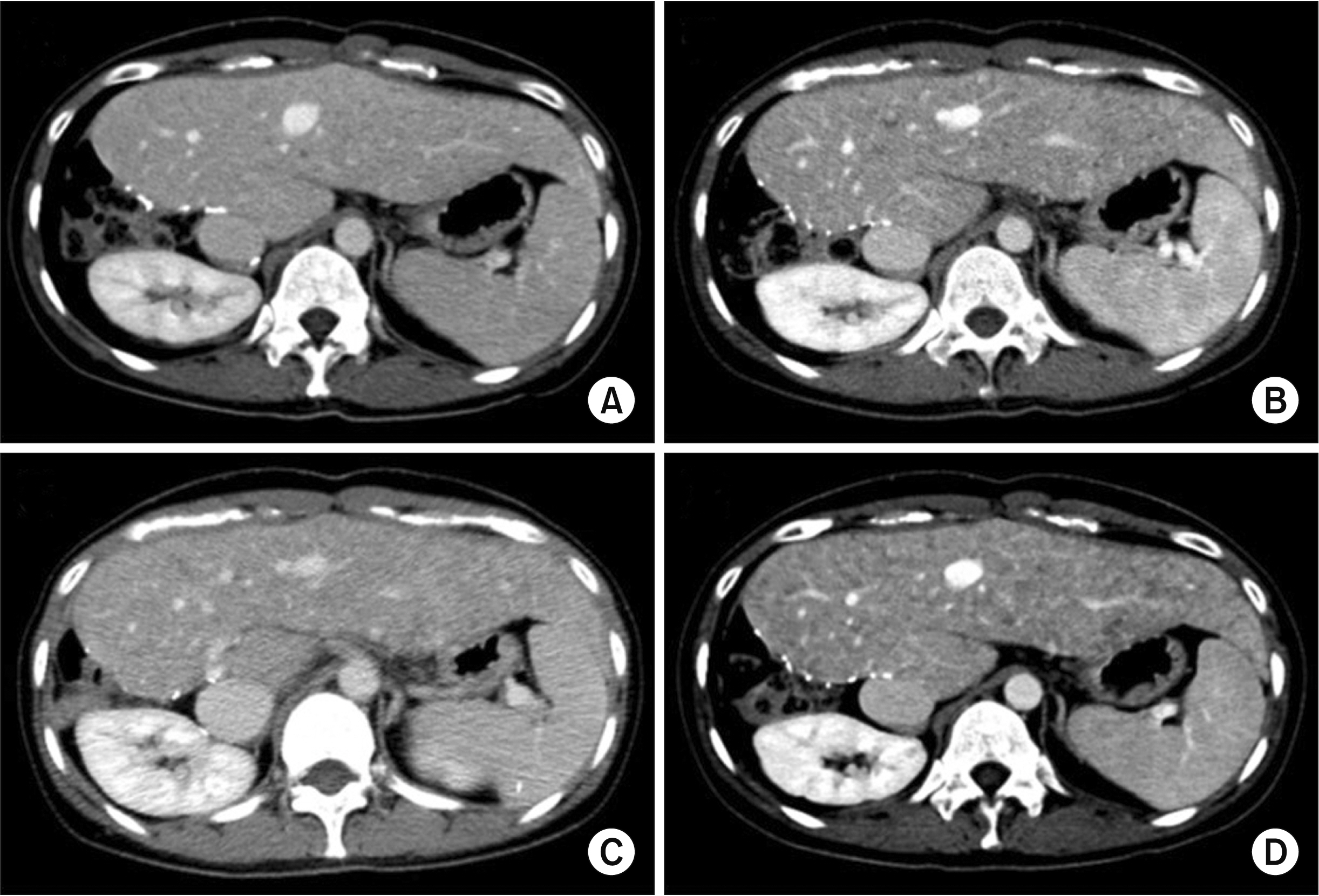
- Large hepatic tumors can invade the retrohepatic inferior vena cava (IVC). Resecting the involved IVC wall is necessary to achieve complete tumor resection. We present detailed surgical procedures of IVC resection and patch venoplasty under the standard and modified total hepatic vascular exclusion (THVE) techniques applied to two patients who underwent aggressive surgery for hepatic tumors. The first case was a 55-year-old male with advanced intrahepatic cholangiocarcinoma. The extent of resection was extended right hepatectomy with caudate lobe resection, right adrenalectomy, and portal vein segmental resection-anastomosis. The invasion site at the IVC was excised and repaired with an expanded polytetraf luoroethylene patch under modified THVE. This patient recovered uneventfully. At postoperative 10 months, second primary cancer occurred in the duodenum. The patient underwent pancreaticoduodenectomy but passed away at post-surgery 6 weeks due to pneumonia-associated sepsis. The second case was a 35-year-old female with giant cavernous hemangioma. As separating the right liver from the IVC was infeasible through conventional dissection techniques, standard THVE was performed. The short hepatic vein was too large to repair directly without risk of IVC stenosis. Thus, a cryopreserve iliac vein allograft patch was applied to repair the defect. The patient recovered uneventfully from the operation. The patient is currently doing well for 6 years. However, progressive hemangiomatosis occurred. In conclusion, standard and modified THVE techniques are proposed as useful techniques to achieve complete tumor resection in patients with large liver tumors invading the retrohepatic IVC.
Keyword
Figure
Reference
-
1. Hwang S, Moon DB, Lee SG. 2010; Liver transplantation and conventional surgery for advanced hepatocellular carcinoma. Transpl Int. 23:723–727. DOI: 10.1111/j.1432-2277.2010.01103.x. PMID: 20477996.
Article2. Ko S, Kirihataya Y, Matsumoto Y, Takagi T, Matsusaka M, Mukogawa T, et al. 2016; Retrocaval liver lifting maneuver and modifications of total hepatic vascular exclusion for liver tumor resection. World J Hepatol. 8:411–420. DOI: 10.4254/wjh.v8.i8.411. PMID: 27004089. PMCID: PMC4794531.
Article3. Smyrniotis VE, Kostopanagiotou GG, Gamaletsos EL, Vassiliou JG, Voros DC, Fotopoulos AC, et al. 2002; Total versus selective hepatic vascular exclusion in major liver resections. Am J Surg. 183:173–178. DOI: 10.1016/S0002-9610(01)00864-9. PMID: 11918884.
Article4. Zografos GN, Kakaviatos ND, Skiathitis S, Habib N. 1999; Total vascular exclusion for liver resections: pros and cons. J Surg Oncol. 72:50–55. DOI: 10.1002/(SICI)1096-9098(199909)72:1<50::AID-JSO14>3.0.CO;2-A. PMID: 10477880.
Article5. Fu SY, Lau WY, Li AJ, Yang Y, Pan ZY, Sun YM, et al. 2010; Liver resection under total vascular exclusion with or without preceding Pringle manoeuvre. Br J Surg. 97:50–55. DOI: 10.1002/bjs.6841. PMID: 20013928.
Article6. Azoulay D, Lim C, Salloum C, Andreani P, Maggi U, Bartelmaos T, et al. 2015; Complex liver resection using standard total vascular exclusion, venovenous bypass, and in situ hypothermic portal perfusion: an audit of 77 consecutive cases. Ann Surg. 262:93–104. DOI: 10.1097/SLA.0000000000000787. PMID: 24950284.7. Cherqui D, Malassagne B, Colau PI, Brunetti F, Rotman N, Fagniez PL. 1999; Hepatic vascular exclusion with preservation of the caval flow for liver resections. Ann Surg. 230:24–30. DOI: 10.1097/00000658-199907000-00004. PMID: 10400032. PMCID: PMC1420840.
Article8. Azoulay D, Andreani P, Maggi U, Salloum C, Perdigao F, Sebagh M, et al. 2006; Combined liver resection and reconstruction of the supra-renal vena cava: the Paul Brousse experience. Ann Surg. 244:80–88. DOI: 10.1097/01.sla.0000218092.83675.bc. PMID: 16794392. PMCID: PMC1570596.9. Belghiti J, Noun R, Zante E, Ballet T, Sauvanet A. 1996; Portal triad clamping or hepatic vascular exclusion for major liver resection. A controlled study. Ann Surg. 224:155–161. DOI: 10.1097/00000658-199608000-00007. PMID: 8757378. PMCID: PMC1235336.10. Emre S, Schwartz ME, Katz E, Miller CM. 1993; Liver resection under total vascular isolation. Variations on a theme. Ann Surg. 217:15–19. DOI: 10.1097/00000658-199301000-00004. PMID: 8424696. PMCID: PMC1242728.
Article11. Malde DJ, Khan A, Prasad KR, Toogood GJ, Lodge JP. 2011; Inferior vena cava resection with hepatectomy: challenging but justified. HPB (Oxford). 13:802–810. DOI: 10.1111/j.1477-2574.2011.00364.x. PMID: 21999594. PMCID: PMC3238015.
Article12. Lodge JP, Ammori BJ, Prasad KR, Bellamy MC. 2000; Ex vivo and in situ resection of inferior vena cava with hepatectomy for colorectal metastases. Ann Surg. 231:471–479. DOI: 10.1097/00000658-200004000-00004. PMID: 10749606. PMCID: PMC1421021.
Article13. Gonultas F, Akbulut S, Barut B, Usta S, Kutluturk K, Kutlu R, et al. 2020; Usability of inferior vena cava interposition graft during living donor liver transplantation: is this approach always necessary? J Gastrointest Surg. 24:1540–1551. DOI: 10.1007/s11605-019-04342-6. PMID: 31385171.
Article14. Yoon YI, Lee SG, Moon DB, Ahn CS, Hwang S, Kim KH, et al. 2019; Surgical techniques and long-term outcomes of living-donor liver transplantation with inferior vena cava replacement using atriocaval synthetic interposition graft for Budd-Chiari syndrome. Ann Surg. 269:e43–e45. DOI: 10.1097/SLA.0000000000002847. PMID: 30080720.
Article15. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. 2013; No-touch en bloc right lobe living-donor liver transplantation with inferior vena cava replacement for hepatocellular carcinoma close to retrohepatic inferior vena cava: case report. Transplant Proc. 45:3135–3139. DOI: 10.1016/j.transproceed.2013.08.052. PMID: 24157050.
Article16. Namgoong JM, Choi JU, Hwang S, Oh SH, Park GC. 2019; Pediatric living donor liver transplantation with homograft replacement of retrohepatic inferior vena cava for advanced hepatoblastoma. Ann Hepatobiliary Pancreat Surg. 23:178–182. DOI: 10.14701/ahbps.2019.23.2.178. PMID: 31225421. PMCID: PMC6558128.
Article17. Namgoong JM, Hwang S, Oh SH, Kim KM, Park GC, Ahn CS, et al. 2020; Living-donor liver transplantation with inferior vena cava replacement in an infant recipient with advanced hepatoblastoma. Ann Hepatobiliary Pancreat Surg. 24:72–77. DOI: 10.14701/ahbps.2020.24.1.72. PMID: 32181433. PMCID: PMC7061035.
Article18. Franko J, Hsu HW, Thirunavukarasu P, Frankova D, Goldman CD. 2017; Chemotherapy and radiation components of neoadjuvant treatment of pancreatic head adenocarcinoma: impact on perioperative mortality and long-term survival. Eur J Surg Oncol. 43:351–357. DOI: 10.1016/j.ejso.2016.10.021. PMID: 27863846.
Article19. Lehmann FS, Beglinger C, Schnabel K, Terracciano L. 1999; Progressive development of diffuse liver hemangiomatosis. J Hepatol. 30:951–954. DOI: 10.1016/S0168-8278(99)80152-4. PMID: 10365825.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Resection for HCC invading the Inferior Vena Cava: using veno-venous bypass and saphenous vein patch graft
- Experience of an En Bloc Resection of Right Lobe of Liver, Adrenal, Kidney and Infrahepatic Vena Cava with the Aid of Veno-venous Bypass
- A Successful Management of the Renal Sarcoma with an Extension of the Tumor into the Inferior Vena Cava and the Right Ventricle Progressing Multi-Organ Failure Using a Deep Hypothermic Circulatory Arrest
- Suprarenal Filter Placement in the Inferior Vena Cava to Prevent Tumor Emboli During Radical Nephrectomy in Renal Cell Carcinoma Invading the Inferior Vena Cava
- Obstruction of the Hepatic Portion of the Inferior Vena Cava