Int J Thyroidol.
2021 Nov;14(2):81-86. 10.11106/ijt.2021.14.2.81.
Optimal Surgical Extent of Therapeutic Lateral Neck Dissection in Well-Differentiated Thyroid Carcinoma Patients with Clinical Lateral Lymph Node Metastasis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2522911
- DOI: http://doi.org/10.11106/ijt.2021.14.2.81
Abstract
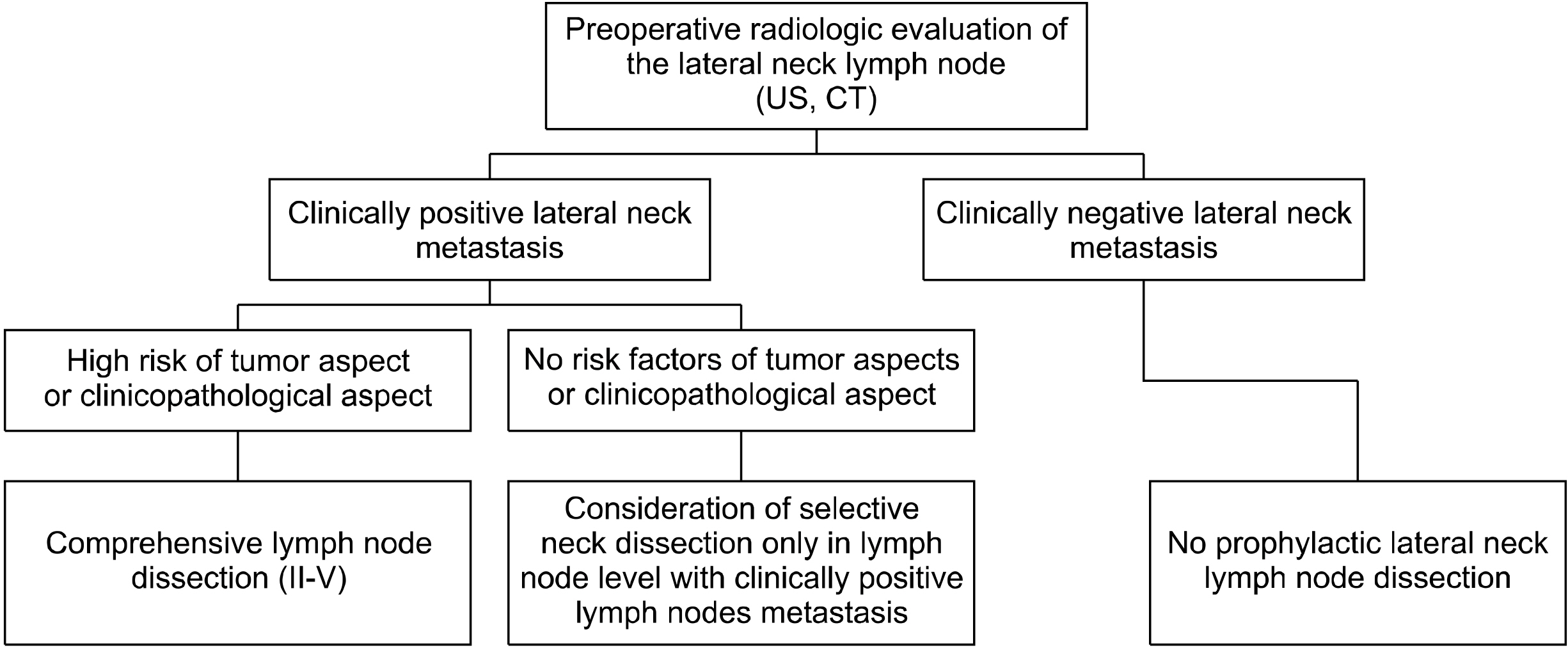
- Regional neck metastases in well-differentiated thyroid carcinoma (WDTC) are relatively frequent. The prognostic effects of lymph node (LN) metastases remain controversial. However, it is well known that lateral LN metastasis is related to the recurrence of the disease. In general, when lateral neck LN metastasis is confirmed in WDTC patients, therapeutic lateral neck dissection is recommended. However, the optimal surgical extent of therapeutic lateral neck dissection in WDTC patients with clinical lateral LN metastasis is not clearly presented. Traditional comprehensive neck dissection including level II, III, IV and V even in patients with minimal lateral neck metastases may not be reasonable when considering both oncologic safety and functional aspects. There is controversy whether it is always necessary to perform level II and V LN dissection for all WDTC patients with clinical lateral LN metastasis. This is due to the fact that the likelihood of postoperative complications by the damage of the spinal accessory nerve increases with level II and level V dissection. Therefore, many studies have been reported on the possibility of omitting levels II (especially IIb) and V during therapeutic comprehensive lateral neck dissection. However, there have been no definite conclusions about it, and it is still debate. In this article, we reviewed to find out optimal lateral neck dissection range for WDTC patients with clinical lateral neck metastasis.
Figure
Reference
-
References
1. Mulla MG, Knoefel WT, Gilbert J, McGregor A, Schulte KM. 2012; Lateral cervical lymph node metastases in papillary thyroid cancer: a systematic review of imaging-guided and prophylactic removal of the lateral compartment. Clin Endocrinol (Oxf). 77(1):126–31. DOI: 10.1111/j.1365-2265.2012.04336.x. PMID: 22233478.
Article2. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. 2012; The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 22(11):1144–52. DOI: 10.1089/thy.2012.0043. PMID: 23083442.
Article3. Qubain SW, Nakano S, Baba M, Takao S, Aikou T. 2002; Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 131(3):249–56. DOI: 10.1067/msy.2002.120657. PMID: 11894028.
Article4. Ito Y, Fukushima M, Tomoda C, Inoue H, Kihara M, Higashiyama T, et al. 2009; Prognosis of patients with papillary thyroid carcinoma having clinically apparent metastasis to the lateral compartment. Endocr J. 56(6):759–66. DOI: 10.1507/endocrj.K09E-025. PMID: 19506324.
Article5. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2016; 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. DOI: 10.1089/thy.2015.0020. PMID: 26462967. PMCID: PMC4739132.
Article6. Nixon IJ, Wang LY, Palmer FL, Tuttle RM, Shaha AR, Shah JP, et al. 2014; The impact of nodal status on outcome in older patients with papillary thyroid cancer. Surgery. 156(1):137–46. DOI: 10.1016/j.surg.2014.03.027. PMID: 24878458.
Article7. Kim SK, Park I, Hur N, Choe JH, Kim JH, Kim JS. 2017; Patterns, predictive factors and prognostic impact of multilevel metastasis in N1b papillary thyroid carcinoma. Br J Surg. 104(7):857–67. DOI: 10.1002/bjs.10514. PMID: 28295219.
Article8. Heaton CM, Chang JL, Orloff LA. 2016; Prognostic implications of lymph node yield in central and lateral neck dissections for well-differentiated papillary thyroid carcinoma. Thyroid. 26(3):434–40. DOI: 10.1089/thy.2015.0318. PMID: 26825749.
Article9. Joo JY, Jin J, Seo ST, Lim YC, Rha KS, Koo BS. 2015; Recurrence in regional lymph nodes after total thyroidectomy and neck dissection in patients with papillary thyroid cancer. Oral Oncol. 51(2):164–9. DOI: 10.1016/j.oraloncology.2014.11.004. PMID: 25435434.
Article10. Terrell JE, Welsh DE, Bradford CR, Chepeha DB, Esclamado RM, Hogikyan ND, et al. 2000; Pain, quality of life, and spinal accessory nerve status after neck dissection. Laryngoscope. 110(4):620–6. DOI: 10.1097/00005537-200004000-00016. PMID: 10764008.
Article11. Inoue H, Nibu K, Saito M, Otsuki N, Ishida H, Onitsuka T, et al. 2006; Quality of life after neck dissection. Arch Otolaryngol Head Neck Surg. 132(6):662–6. DOI: 10.1001/archotol.132.6.662. PMID: 16785413.
Article12. Lee BJ, Wang SG, Lee JC, Son SM, Kim IJ, Kim YK. 2007; Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 133(10):1028–30. DOI: 10.1001/archotol.133.10.1028. PMID: 17938327.
Article13. Lee J, Sung TY, Nam KH, Chung WY, Soh EY, Park CS. 2008; Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients? World J Surg. 32(5):716–21. DOI: 10.1007/s00268-007-9381-z. PMID: 18087766.
Article14. Koo BS, Yoon YH, Kim JM, Choi EC, Lim YC. 2009; Predictive factors of level IIb lymph node metastasis in patients with papillary thyroid carcinoma. Ann Surg Oncol. 16(5):1344–7. DOI: 10.1245/s10434-009-0367-y. PMID: 19224280.
Article15. Kupferman ME, Weinstock YE, Santillan AA, Mishra A, Roberts D, Clayman GL, et al. 2008; Predictors of level V metastasis in well-differentiated thyroid cancer. Head Neck. 30(11):1469–74. DOI: 10.1002/hed.20904. PMID: 18704973.
Article16. Kupferman ME, Patterson M, Mandel SJ, LiVolsi V, Weber RS. 2004; Patterns of lateral neck metastasis in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 130(7):857–60. DOI: 10.1001/archotol.130.7.857. PMID: 15262763.
Article17. Eskander A, Merdad M, Freeman JL, Witterick IJ. 2013; Pattern of spread to the lateral neck in metastatic well-differentiated thyroid cancer: a systematic review and meta-analysis. Thyroid. 23(5):583–92. DOI: 10.1089/thy.2012.0493. PMID: 23148663.
Article18. Lombardi D, Paderno A, Giordano D, Barbieri D, Taboni S, Piazza C, et al. 2018; Therapeutic lateral neck dissection in well-differentiated thyroid cancer: analysis on factors predicting distribution of positive nodes and prognosis. Head Neck. 40(2):242–50. DOI: 10.1002/hed.24936. PMID: 28963802.
Article19. Kim SK, Park I, Hur N, Lee JH, Choe JH, Kim JH, et al. 2017; Should level V be routinely dissected in N1b papillary thyroid carcinoma? Thyroid. 27(2):253–60. DOI: 10.1089/thy.2016.0364. PMID: 27762727.
Article20. Won HR, Chang JW, Kang YE, Kang JY, Koo BS. 2018; Optimal extent of lateral neck dissection for well-differentiated thyroid carcinoma with metastatic lateral neck lymph nodes: a systematic review and meta-analysis. Oral Oncol. 87:117–25. DOI: 10.1016/j.oraloncology.2018.10.035. PMID: 30527226.
Article21. Roh JL, Kim JM, Park CI. 2008; Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol. 15(4):1177–82. DOI: 10.1245/s10434-008-9813-5. PMID: 18253801.
Article22. King JM, Corbitt C, Miller FR. 2011; Management of lateral cervical metastases in papillary thyroid cancer: patterns of lymph node distribution. Ear Nose Throat J. 90(8):386–9. DOI: 10.1177/014556131109000814. PMID: 21853444.
Article23. Farrag T, Lin F, Brownlee N, Kim M, Sheth S, Tufano RP. 2009; Is routine dissection of level II-B and V-A necessary in patients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. World J Surg. 33(8):1680–3. DOI: 10.1007/s00268-009-0071-x. PMID: 19506945.
Article24. McNamara WF, Wang LY, Palmer FL, Nixon IJ, Shah JP, Patel SG, et al. 2016; Pattern of neck recurrence after lateral neck dissection for cervical metastases in papillary thyroid cancer. Surgery. 159(6):1565–71. DOI: 10.1016/j.surg.2016.02.005. PMID: 26994486. PMCID: PMC5138026.
Article25. Turanli S. 2007; Is the type of dissection in lateral neck metastasis for differentiated thyroid carcinoma important? Otolaryngol Head Neck Surg. 136(6):957–60. DOI: 10.1016/j.otohns.2006.12.013. PMID: 17547987.
Article26. Strajina V, Dy BM, McKenzie TJ, Al-Hilli Z, Ryder M, Farley DR, et al. 2019; Comprehensive lateral neck dissection in papillary thyroid carcinoma may reduce lateral neck recurrence rates. Ann Surg Oncol. 26(1):86–92. DOI: 10.1245/s10434-018-6871-1. PMID: 30411267.
Article27. Javid M, Graham E, Malinowski J, Quinn CE, Carling T, Udelsman R, et al. 2016; Dissection of levels II through V is required for optimal outcomes in patients with lateral neck lymph node metastasis from papillary thyroid carcinoma. J Am Coll Surg. 222(6):1066–73. DOI: 10.1016/j.jamcollsurg.2016.02.006. PMID: 27049777.
Article28. Zhang D, Gao L, Xie L, He G, Chen J, Fang L, et al. 2017; Comparison between video-assisted and open lateral neck dissection for papillary thyroid carcinoma with lateral neck lymph node metastasis: a prospective randomized study. J Laparoendosc Adv Surg Tech A. 27(11):1151–7. DOI: 10.1089/lap.2016.0650. PMID: 28488911.
Article29. Kupferman ME, Patterson DM, Mandel SJ, LiVolsi V, Weber RS. 2004; Safety of modified radical neck dissection for differentiated thyroid carcinoma. Laryngoscope. 114(3):403–6. DOI: 10.1097/00005537-200403000-00002. PMID: 15091209.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lateral Neck Node Dissection in Differentiated Thyroid Carcinoma
- Extent of Prophylactic Neck Dissection in Sporadic Medullary Thyroid Cancer
- Optimal Neck Dissection Extent for Metastatic Lymph Nodes in Papillary Thyroid Cancer
- Central Neck Dissection for Papillary Thyroid Carcinoma
- Chyle Leakage After Right Selective Lymph Node Dissection in a Patient With Papillary Thyroid Cancer: A Case Report