J Korean Med Sci.
2021 Nov;36(46):e293. 10.3346/jkms.2021.36.e293.
Prevalence of Bladder Pain Syndromelike Symptoms: a Population-based Study in Korea
- Affiliations
-
- 1Department of Urology, Kyung Hee University Medical Center, Kyung Hee University College of Medicine, Seoul, Korea
- 2Department of Urology, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea
- 3Department of Urology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- KMID: 2522878
- DOI: http://doi.org/10.3346/jkms.2021.36.e293
Abstract
Objectives
To investigate the prevalence of bladder pain syndrome (BPS)-like symptoms in the general population of South Korea.
Methods
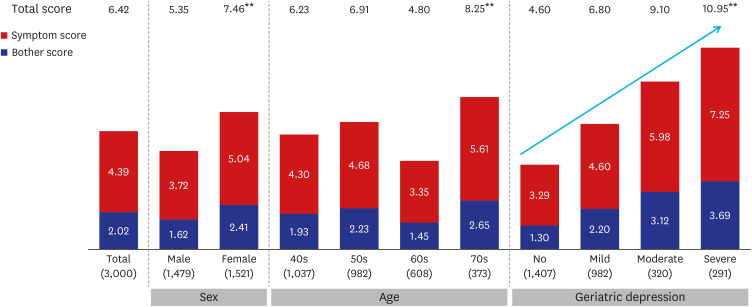
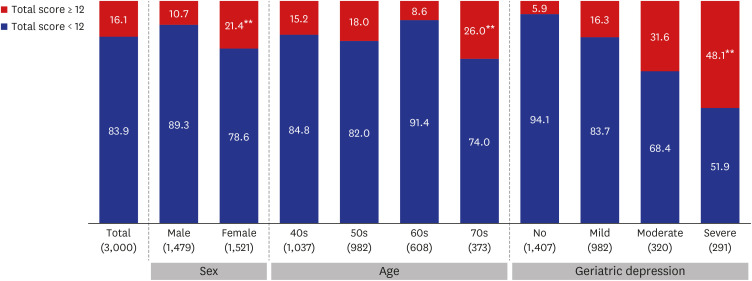
Between April 16, 2016 and April 29, 2016, we conducted an online survey and computer-assisted personal interviews with adults aged 40–79 years in Korea using structured questionnaires. The sample size was 3,000 (95% confidence level standard error ± 1.79%), and the sampling method was simple randomization according to sex, age, and residential area in proportion to the resident registration demographics of the Korean Ministry of Interior and Safety as of March 2016. All participants were surveyed using the Korean version of the Pelvic Pain and Urgency/Frequency (PUF) Patient Symptom Scale and Geriatric Depression Scale (GDS). The primary outcome was the prevalence of BPS-like symptoms, defined as a total PUF score of ≥ 12.
Results
Overall, the prevalence of BPS-like symptoms was 16.4% (483 of 3,000 participants). Women (21.4%) had a significantly higher prevalence of BPS-like symptoms than men (10.7%) (P < 0.01). The prevalence by age was significantly higher in the 70s group than in the other age groups (P < 0.01), and increased significantly with the increasing severity of depression on the GDS (P < 0.01). The prevalence of BPS-like symptoms according to the marital status was significantly different, that is, the prevalence among divorced/bereaved individuals was higher than those of married or unmarried individuals (P < 0.01).
Conclusion
Our large, representative population-based study showed that BPS-like symptoms are widespread among the general population of South Korea. BPS is considered a disease that deserves greater attention as it is far more common than previously thought and can negatively affect many people's quality of life.
Keyword
Figure
Reference
-
1. Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018; 122(5):729–743. PMID: 29777618.
Article2. Doggweiler R, Whitmore KE, Meijlink JM, Drake MJ, Frawley H, Nordling J, et al. A standard for terminology in chronic pelvic pain syndromes: a report from the chronic pelvic pain working group of the international continence society. Neurourol Urodyn. 2017; 36(4):984–1008. PMID: 27564065.
Article3. Kim YH. Diagnosis and management of interstitial cystitis/ painful bladder syndrome. J Korean Continence Soc. 2008; 12(2):99–113.
Article4. Leppilahti M, Sairanen J, Tammela TL, Aaltomaa S, Lehtoranta K, Auvinen A, et al. Prevalence of clinically confirmed interstitial cystitis in women: a population based study in Finland. J Urol. 2005; 174(2):581–583. PMID: 16006902.
Article5. Bade JJ, Rijcken B, Mensink HJ. Interstitial cystitis in The Netherlands: prevalence, diagnostic criteria and therapeutic preferences. J Urol. 1995; 154:2035–2037. PMID: 7500452.
Article6. Jones CA, Nyberg L. Epidemiology of interstitial cystitis. Urology. 1997; 49(5A):Suppl. 2–9.
Article7. Curhan GC, Speizer FE, Hunter DJ, Curhan SG, Stampfer MJ. Epidemiology of interstitial cystitis: a population based study. J Urol. 1999; 161(2):549–552. PMID: 9915446.
Article8. Leppilahti M, Tammela TL, Huhtala H, Auvinen A. Prevalence of symptoms related to interstitial cystitis in women: a population based study in Finland. J Urol. 2002; 168(1):139–143. PMID: 12050508.
Article9. Roberts RO, Bergstralh EJ, Bass SE, Lightner DJ, Lieber MM, Jacobsen SJ. Incidence of physician-diagnosed interstitial cystitis in Olmsted County: a community-based study. BJU Int. 2003; 91(3):181–185. PMID: 12581000.
Article10. Clemens JQ, Meenan RT, Rosetti MC, Gao SY, Calhoun EA. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol. 2005; 173:98–102. PMID: 15592041.
Article11. Rosenberg MT, Hazzard M. Prevalence of interstitial cystitis symptoms in women: a population based study in the primary care office. J Urol. 2005; 174(6):2231–2234. PMID: 16280776.
Article12. Temml C, Wehrberger C, Riedl C, Penholzer A, Marszalek M, Madersbacher S. Prevalence and correlates for interstitial cystitis symptoms in women participating in a health screening project. Eur Urol. 2007; 51:803–808. PMID: 16979286.
Article13. Inoue Y, Mita K, Kakehashi M, Kato M, Usui T. Prevalence of painful bladder syndrome (PBS) symptoms in adult women in the general population in Japan. Neurourol Urodyn. 2009; 28(3):214–218. PMID: 19260086.
Article14. Choe JH, Son H, Song YS, Kim JC, Lee JZ, Lee KS. Prevalence of painful bladder syndrome/interstitial cystitis-like symptoms in women: a population-based study in Korea. World J Urol. 2011; 29(1):103–108. PMID: 20340026.
Article15. Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011; 186(2):540–544. PMID: 21683389.
Article16. Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002; 60(4):573–578. PMID: 12385909.
Article17. Son HC, Jung YJ, Chang JS, Kim SH, Hong SK, Oh SJ, et al. Translation and linguistic validation of the Korean version of the pelvic pain and urgency/frequency patient symptom scale. Int Neurourol J. 2010; 14(2):112–121. PMID: 21120221.
Article18. Shalom DF, Klapper A, Lin S, Gurshumov E. Use of the pain urgency frequency (PUF) questionnaire to measure response of patients with interstitial cystitis/painful bladder syndrome to a treatment regimen of intravesical DMSO and 1% lidocaine solution. J Pelvic Med Surg. 2009; 15(1):5–10.
Article19. Parsons CL, Greenberger M, Gabal L, Bidair M, Barme G. The role of urinary potassium in the pathogenesis and diagnosis of interstitial cystitis. J Urol. 1998; 159(6):1862–1866. PMID: 9598476.
Article20. Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology. 2001; 57(3):428–432. PMID: 11248610.
Article21. Parsons CL, Forrest J, Nickel JC, Evans R, Lloyd LK, Barkin J, et al. Effect of pentosan polysulfate therapy on intravesical potassium sensitivity. Urology. 2002; 59(3):329–333. PMID: 11880064.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Urethral Pain Syndrome Really Part of Bladder Pain Syndrome?
- Prevalence of Stress Urinary Incontinence and Bladder Irritative Symptoms in Women: A Community Based Survey
- The Prevalence of Lower Urinary Tract Symptoms and Overactive Bladder in South Korea: A Cross-Sectional, Population-Based Study
- Epidemiology of underactive bladder: Common but underresearched
- Non-cardiac Chest Pain in Japan: Prevalence, Impact, and Consultation Behavior - A Population-based Study