Neonatal Med.
2021 Nov;28(4):149-152. 10.5385/nm.2021.28.4.149.
Hypernatremia in Newborn Due to Uncontrolled Maternal Diabetes Insipidus
- Affiliations
-
- 1Department of Pediatrics, Kangwon National University Hospital, Chuncheon, Korea
- 2Department of Pediatrics, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2522851
- DOI: http://doi.org/10.5385/nm.2021.28.4.149
Abstract
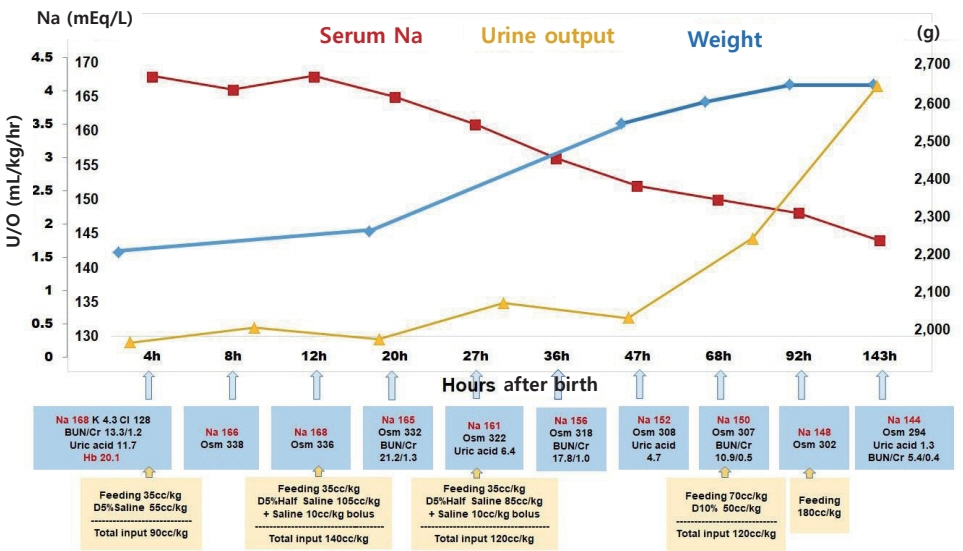
- Neonatal hypernatremia often occurs in poorly breastfeeding infants, and rehydration without complications is the primary treatment. However, the etiologies and management for neonates who present with hypernatremia immediately after birth are not well reported. In this case report, we describe a neonate with hypernatremia and hyperosmolality, born to a mother with oligohydramnios of unknown etiology. Meticulous fluid therapies considering the time to physiologic diuresis were successfully performed, and the underlying cause was determined to be an uncontrolled maternal central diabetes insipidus.
Figure
Reference
-
1. Lavagno C, Camozzi P, Renzi S, Lava SA, Simonetti GD, Bianchetti MG, et al. Breastfeeding-associated hypernatremia: a systematic review of the literature. J Hum Lact. 2016; 32:67–74.2. Tomarelli G, Arriagada D, Donoso A, Diaz F. Extreme neonatal hypernatremia and acute kidney injury associated with failure of lactation. J Pediatr Intensive Care. 2020; 9:124–7.3. Sarin A, Thill A, Yaklin CW. Neonatal hypernatremic dehydration. Pediatr Ann. 2019; 48:e197–200.4. Sha XY, Xiong ZF, Liu HS, Di XD, Ma TH. Maternal-fetal fluid balance and aquaporins: from molecule to physiology. Acta Pharmacol Sin. 2011; 32:716–20.5. Shennan DB, Boyd CA. Ion transport by the placenta: a review of membrane transport systems. Biochim Biophys Acta. 1987; 906:437–57.6. Schreyer P, Sherman DJ, Ervin MG, Day L, Ross MG. Maternal dehydration: impact on ovine amniotic fluid volume and composition. J Dev Physiol. 1990; 13:283–7.7. Bidiwala KS, Lorenz JM, Kleinman LI. Renal function correlates of postnatal diuresis in preterm infants. Pediatrics. 1988; 82:50–8.8. Marques P, Gunawardana K, Grossman A. Transient diabetes insipidus in pregnancy. Endocrinol Diabetes Metab Case Rep. 2015; 2015:150078.9. Sum M, Fleischer JB, Khandji AG, Wardlaw SL. Pitfall in the diagnosis of diabetes insipidus and pregnancy. Case Rep Obstet Gynecol. 2017; 2017:7879038.10. Lamas C, del Pozo C, Villabona C; Neuroendocrinology Group of the SEEN. Clinical guidelines for management of diabetes insipidus and syndrome of inappropriate antidiuretic hormone secretion after pituitary surgery. Endocrinol Nutr. 2014; 61:e15–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Hypernatremia with Craniopharyngioma - A Case Report -
- A Case of Obstructive Uropathy Accompanied with Severe Hypernatremia
- Unexpected Fatal Hypernatremia after Successful Cardiopulmonary Resuscitation with Therapeutic Hypothermia: A Case Report
- A case of Sheehan's syndrome with central diabetes insipidus showing hemorrhagic pituitary apoplexy
- Management of diabetes insipidus during anesthesia for brain germinoma resection in a child : A case report