Obstet Gynecol Sci.
2021 Nov;64(6):555-559. 10.5468/ogs.21190.
Rectal mobilization for laparoscopic pelvic lymphadenectomy of the lower paracervical pathway in patients with uterine cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Federation of National Public Service Personnel Mutual Aid Associations, Tachikawa Hospital, Tokyo, Japan
- 2Department of Obstetrics and Gynecology, Keio University School of Medicine, Tokyo, Japan
- 3Department of Gynecologic Oncology, Cancer Institute Hospital, Tokyo, Japan
- KMID: 2522481
- DOI: http://doi.org/10.5468/ogs.21190
Abstract
Objective
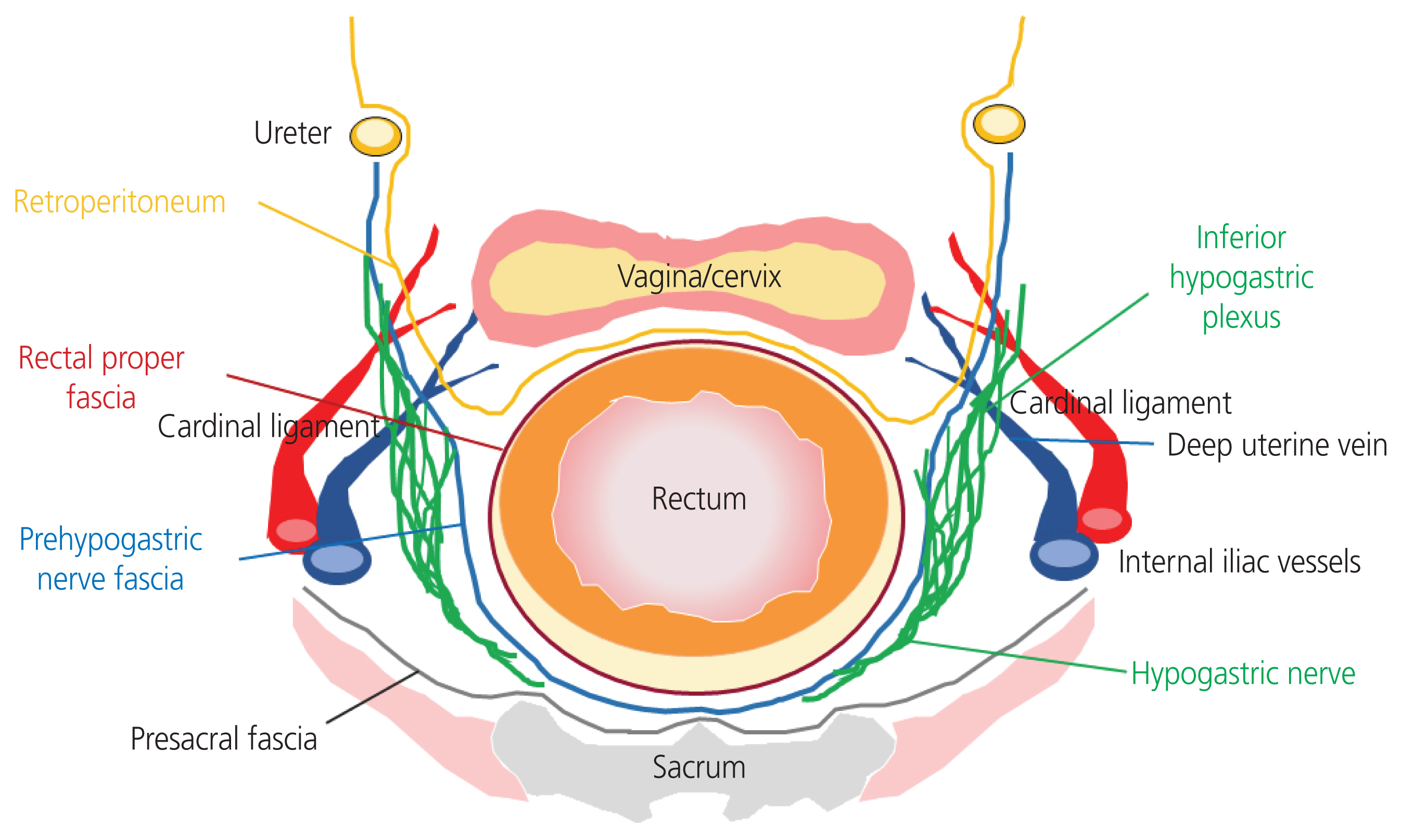
The pelvic lymphatic drainage system comprises the upper and lower paracervical pathways (LPPs). Lymph node dissection of the LPP, including the cardinal ligament, internal iliac, internal common iliac, and presacral lymph nodes, requires higher surgical skills because of the anatomical limitations of the pelvic cavity and the dissection of vessels while preserving the nerves in the pelvic floor. In this video, we demonstrate rectal mobilization for laparoscopic complete pelvic lymph node dissection of the LPP in patients with uterine cancer.
Methods
Rectal mobilization was performed before complete pelvic lymph node dissection of the LPP. The pararectal space was opened widely and the connective tissue between the presacral fascia and prehypogastric nerve fascia was dissected bilaterally, allowing the rectum to be pulled.
Results
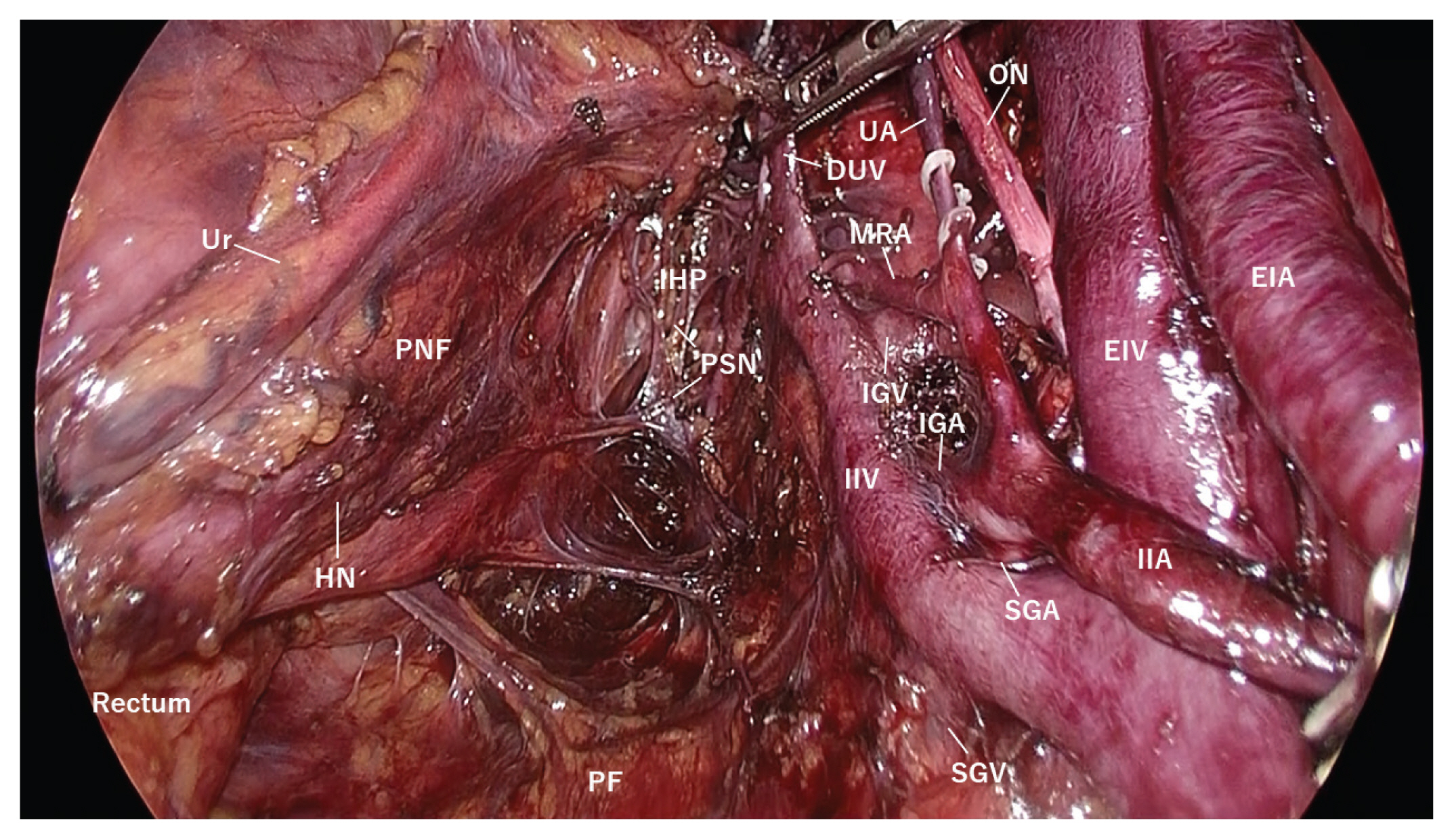
This procedure created a wide-open space in the pelvic floor, allowing clear visualization of the nerves and lymph nodes of the LPP. Laparoscopic complete lymph node dissection of the LPP was performed in the open space while preserving the hypogastric and pelvic splanchnic nerves and isolating the extensive network of blood vessels in the pelvic cavity.
Conclusion
Rectal mobilization enabled the safe execution of laparoscopic complete pelvic lymph node dissection of the LPP in patients with uterine cancer.
Figure
Reference
-
References
1. Geppert B, Lönnerfors C, Bollino M, Arechvo A, Persson J. A study on uterine lymphatic anatomy for standardization of pelvic sentinel lymph node detection in endometrial cancer. Gynecol Oncol. 2017; 145:256–61.
Article2. Persson J, Geppert B, Lönnerfors C, Bollino M, Måsbäck A. Description of a reproducible anatomically based surgical algorithm for detection of pelvic sentinel lymph nodes in endometrial cancer. Gynecol Oncol. 2017; 147:120–5.
Article3. Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008; 9:297–303.
Article4. Van den Tillaart SA, Trimbos JB, Dreef EJ, Jordanova ES, Fleuren GJ. Patterns of parametrial involvement in radical hysterectomy specimens of cervical cancer patients. Int J Gynecol Pathol. 2011; 30:185–92.
Article5. Zhao D, Li B, Zheng S, Ou Z, Zhang Y, Wang Y, et al. Separate lateral parametrial lymph node dissection improves detection rate of parametrial lymph node metastasis in early-stage cervical cancer: 10-year clinical evaluation in a single center in China. Chin J Cancer Res. 2020; 32:804–14.
Article6. Kanao H, Matsuo K, Aoki Y, Tanigawa T, Nomura H, Okamoto S, et al. Feasibility and outcome of total laparoscopic radical hysterectomy with no-look no-touch technique for FIGO IB1 cervical cancer. J Gynecol Oncol. 2019; 30:e71.
Article7. Odagiri T, Watari H, Kato T, Mitamura T, Hosaka M, Sudo S, et al. Distribution of lymph node metastasis sites in endometrial cancer undergoing systematic pelvic and para-aortic lymphadenectomy: a proposal of optimal lymphadenectomy for future clinical trials. Ann Surg Oncol. 2014; 21:2755–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Pelvic Lymphadenectomy in Cervical Cancer
- The Comparison of Minilaparotomy to Laparoscopic Surgery as Staging Pelvic Lymphadenectomy in Prostate Cancer
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Effect on the Local Recurrence and the Survival of Lateral Pelvic Node Dissection in Advanced Lower Rectal Cancer
- Laparoscopic Surgery for Rectal Cancer