J Korean Med Sci.
2021 Nov;36(42):e258. 10.3346/jkms.2021.36.e258.
Pilot Project of Special Emergency Medical Service Team for Anaphylaxis in Gangwon-do, Korea: Results from an Online Questionnaire Survey
- Affiliations
-
- 1Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Division of Allergy and Clinical Immunology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 3Department of Information and Statistics, Yonsei University, Wonju, Korea
- KMID: 2522113
- DOI: http://doi.org/10.3346/jkms.2021.36.e258
Abstract
- Background
Early recognition and prompt intramuscular epinephrine administration are critical for the treatment of anaphylaxis. The special emergency medical service team (SEMST) is a reorganization plan that incorporates first-level emergency medical technicians (EMTs) and nurses from Korea to give the authority to administer epinephrine. This study evaluates the experience of SEMST and aims to investigate further needs in the pre-hospital management of anaphylaxis.
Methods
An online survey of 29 questions on the Gangwon-do 119 EMST was conducted. IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) and R ver.4.0.3. were used for statistical analysis.
Results
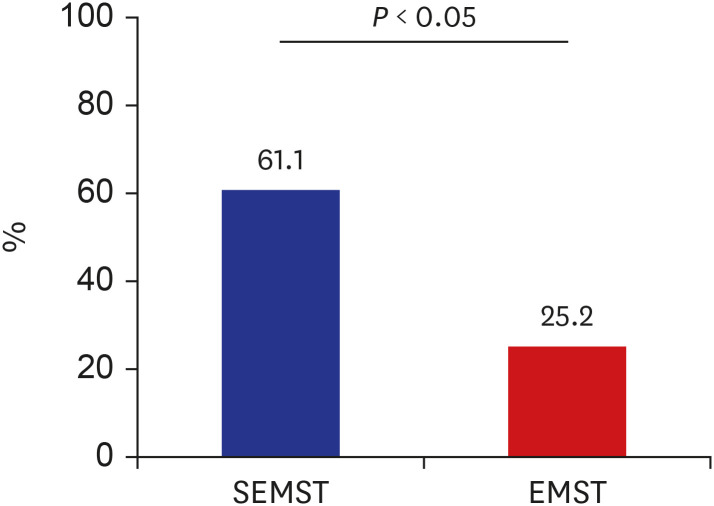
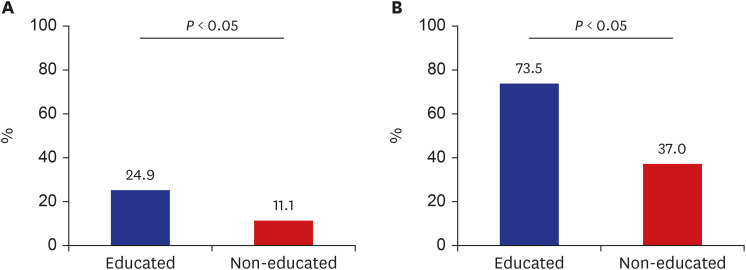
A total of 428 (44.6%) participants responded to the questionnaire, and 55.6% (238/428) experienced anaphylaxis. The common presumed cause was insect sting/animal bites at 84.5% (201/238), followed by food (7.6%, 18/238), and drugs (6.3%, 15/238). The frequency of occurrence was highest for tourist attractions (58.6%, 167/285), followed by homes (31.9%, 91/285) and workplace (3.5%, 10/285). Among 136 medical personnel (31.8%) who were currently active or had been active as the SEMST, 95 (70.0%) experienced anaphylaxis, and 58 (61.1%) used epinephrine, which was significantly lower in the nonSEMST group (n = 36, 25.2%). The biggest difficulty in pre-hospital treatment was the limitation of drug administration authority (23.4%, 22/95). The lack of experience and tricky treatment are the chief difficulties in pediatric anaphylaxis. The percentage of correct answers regarding anaphylaxis awareness was significantly higher in the educated (n = 374) than in the non-educated group (n = 54), both for diagnosis (24.9% vs. 11.1%) and treatment (73.5% vs. 37.0%).
Conclusion
Proper administration of epinephrine is particularly important for pre-hospital anaphylaxis management in rural areas. Expanding SEMST and conducting periodic education using virtual experiences is necessary.
Keyword
Figure
Reference
-
1. Simons FE, Ardusso LR, Dimov V, Ebisawa M, El-Gamal YM, Lockey RF, et al. World Allergy Organization anaphylaxis guidelines: 2013 update of the evidence base. Int Arch Allergy Immunol. 2013; 162(3):193–204. PMID: 24008815.
Article2. Yang MS, Kim JY, Kim BK, Park HW, Cho SH, Min KU, et al. True rise in anaphylaxis incidence: epidemiologic study based on a national health insurance database. Medicine (Baltimore). 2017; 96(5):e5750. PMID: 28151851.3. Yu JE, Lin RY. The epidemiology of anaphylaxis. Clin Rev Allergy Immunol. 2018; 54(3):366–374. PMID: 26357949.
Article4. Jeong K, Ye YM, Kim SH, Kim KW, Kim JH, Kwon JW, et al. A multicenter anaphylaxis registry in Korea: clinical characteristics and acute treatment details from infants to older adults. World Allergy Organ J. 2020; 13(8):100449. PMID: 32817782.
Article5. Jiang N, Yin J, Wen L, Li H. Characteristics of anaphylaxis in 907 Chinese patients referred to a tertiary allergy center: a retrospective study of 1,952 episodes. Allergy Asthma Immunol Res. 2016; 8(4):353–361. PMID: 27126729.
Article6. Lee SY, Ahn K, Kim J, Jang GC, Min TK, Yang HJ, et al. A multicenter retrospective case study of anaphylaxis triggers by age in Korean children. Allergy Asthma Immunol Res. 2016; 8(6):535–540. PMID: 27582405.
Article7. Cardona V, Ansotegui IJ, Ebisawa M, El-Gamal Y, Fernandez Rivas M, Fineman S, et al. World allergy organization anaphylaxis guidance 2020. World Allergy Organ J. 2020; 13(10):100472. PMID: 33204386.
Article8. Shaker MS, Wallace DV, Golden DB, Oppenheimer J, Bernstein JA, Campbell RL, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020; 145(4):1082–1123. PMID: 32001253.
Article9. Oriel RC, Wang J. How to manage food allergy in nursery or school. Curr Opin Allergy Clin Immunol. 2018; 18(3):258–264. PMID: 29561357.
Article10. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000; 30(8):1144–1150. PMID: 10931122.
Article11. Sicherer SH, Simons FE. Section on Allergy and Immunology. Epinephrine for first-aid management of anaphylaxis. Pediatrics. 2017; 139(3):e20164006. PMID: 28193791.
Article12. Dubus JC, Lê MS, Vitte J, Minodier P, Boutin A, Carsin A, et al. Use of epinephrine in emergency department depends on anaphylaxis severity in children. Eur J Pediatr. 2019; 178(1):69–75. PMID: 30269250.
Article13. Sicherer SH, Simons FE. Quandaries in prescribing an emergency action plan and self-injectable epinephrine for first-aid management of anaphylaxis in the community. J Allergy Clin Immunol. 2005; 115(3):575–583. PMID: 15753907.
Article14. Korea Ministry of Government Legislation. Enforcement decree of the Act on 119 Rescue and Emergency Medical Services: Article 11. Updated 2019. Accessed April 29, 2021. https://elaw.klri.re.kr/kor_service/lawView.do?hseq=46887&lang=ENG.15. Korea Ministry of Government Legislation. Enforcement rule of the Emergency Medical Service Act: Article 33. Updated 2019. Accessed April 29, 2021. http://www.law.go.kr.16. Baek HS, Park SS. The emergency medical services system of South Korea: the present and future of emergency medical technicians. Medico Leg Update. 2019; 19(2):688–692.
Article17. Han SY, Ji HK, Yoon SW, Lee CH. Legislation feasibility studies for expanding the business scope of paramedics: focused on high level task in importance, need and allowance. Korean J Emerg Med Serv. 2015; 19(3):117–138.
Article18. Fleming JT, Clark S, Camargo CA Jr, Rudders SA. Early treatment of food-induced anaphylaxis with epinephrine is associated with a lower risk of hospitalization. J Allergy Clin Immunol Pract. 2015; 3(1):57–62. PMID: 25577619.
Article19. Turner PJ, Jerschow E, Umasunthar T, Lin R, Campbell DE, Boyle RJ. Fatal anaphylaxis: mortality rate and risk factors. J Allergy Clin Immunol Pract. 2017; 5(5):1169–1178. PMID: 28888247.
Article20. Park SW, Lee BK, Yun SW. Necessity of epinephrine in pre-hospital stage: in the early management of anaphylaxis following a bee sting. J Korean Soc Emerg Med. 2012; 23(5):578–583.21. Choi JH, Jo YH, Choi ES. Prehospital care status and improvement plan of 119 emergency medical technician to anaphylaxis patients. Korean J Emerg Med Serv. 2016; 20(1):57–70.
Article22. Rea TD, Edwards C, Murray JA, Cloyd DJ, Eisenberg MS. Epinephrine use by emergency medical technicians for presumed anaphylaxis. Prehosp Emerg Care. 2004; 8(4):405–410. PMID: 15626002.23. Campbell RL, Bellolio MF, Knutson BD, Bellamkonda VR, Fedko MG, Nestler DM, et al. Epinephrine in anaphylaxis: higher risk of cardiovascular complications and overdose after administration of intravenous bolus epinephrine compared with intramuscular epinephrine. J Allergy Clin Immunol Pract. 2015; 3(1):76–80. PMID: 25577622.
Article24. Levis JT, Ford JB, Kuo AM. Intracranial hemorrhage after prehospital administration of intramuscular epinephrine. J Emerg Med. 2011; 40(6):e107–e110. PMID: 18757151.
Article25. Wood JP, Traub SJ, Lipinski C. Safety of epinephrine for anaphylaxis in the emergency setting. World J Emerg Med. 2013; 4(4):245–251. PMID: 25215127.
Article26. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100(1):31–36. PMID: 18254479.
Article27. Statistics Korea. Population density 2019–2020. Updated 2021. Accessed April 30, 2021. https://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1007.28. Grabenhenrich LB, Dölle S, Moneret-Vautrin A, Köhli A, Lange L, Spindler T, et al. Anaphylaxis in children and adolescents: the European Anaphylaxis Registry. J Allergy Clin Immunol. 2016; 137(4):1128–1137.e1. PMID: 26806049.
Article29. Jahnz-Rozyk K, Raciborski F, Śliwczyński AM, Kłak A, Pinkas J. Anaphylaxis in Poland: the epidemiology and direct costs. Postepy Dermatol Alergol. 2017; 34(6):573–579. PMID: 29422823.
Article30. Cho H, Kim SH, Lee JH, Kim BS, Lee J, Kim JK, et al. Awareness of anaphylaxis among community and emergency responders in Korea. Allergy Asthma Respir Dis. 2020; 8(3):127–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Awareness of anaphylaxis among community and emergency responders in Korea
- Proposal to establish a hospital dedicated for surgical essential medicines: a pilot project to strengthen the essential medical service in Korea
- Anaphylaxis-related interventional demand and the response status of pediatric and youth educational institutions in Gangwon-do Province, South Korea: A school nurse and childcare teacher survey
- Survey on the needs and satisfaction of special emergency medical service providers for education program in Gangwon province
- Determinants of Nutrition Service Utilization in Health Centers