Yeungnam Univ J Med.
2021 Oct;38(4):289-307. 10.12701/yujm.2021.01102.
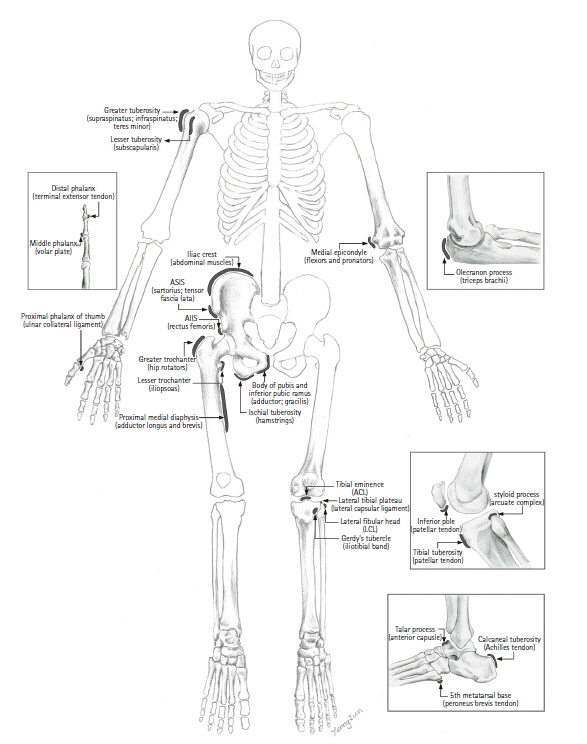
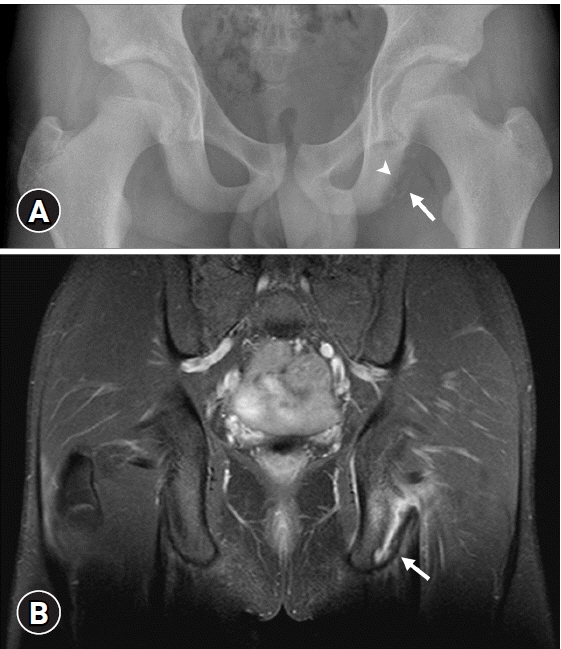
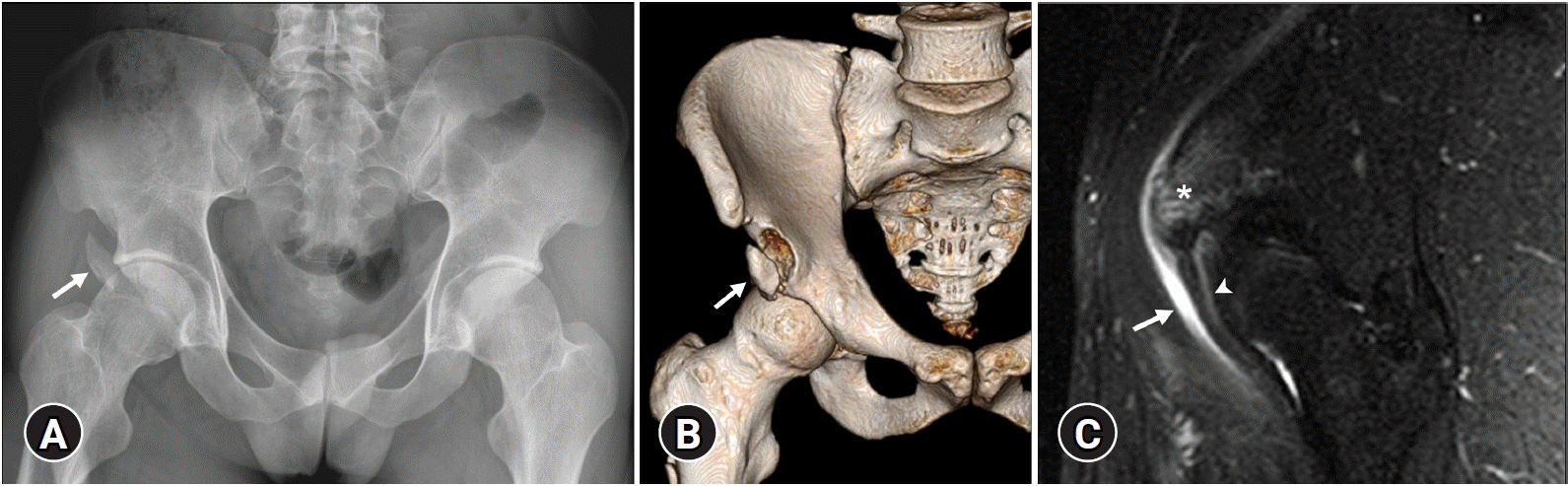
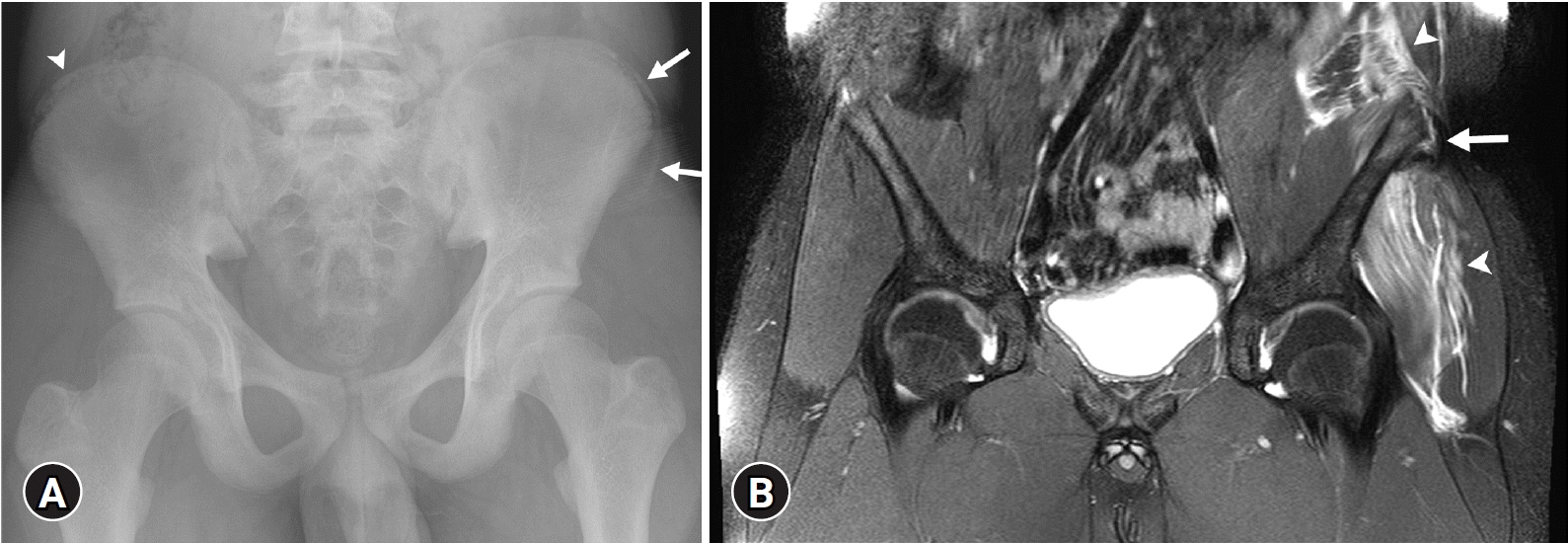
Avulsion injuries: an update on radiologic findings
- Affiliations
-
- 1Department of Radiology, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Radiology, Busan National University Hospital, Busan, Korea
- 3Biomedical Research Institute, Busan National University School of Medicine, Busan, Korea
- 4Department of Radiology, Busan Himchan Hospital, Busan, Korea
- KMID: 2521709
- DOI: http://doi.org/10.12701/yujm.2021.01102
Abstract
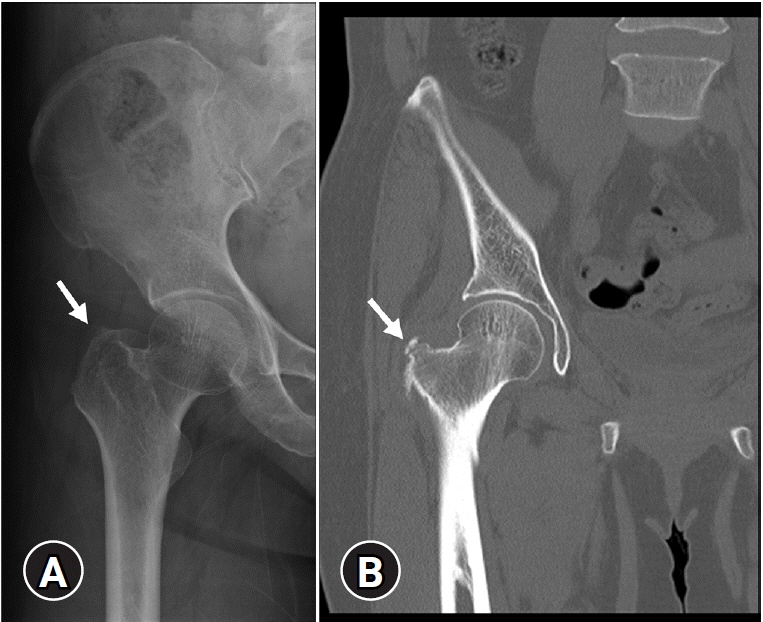
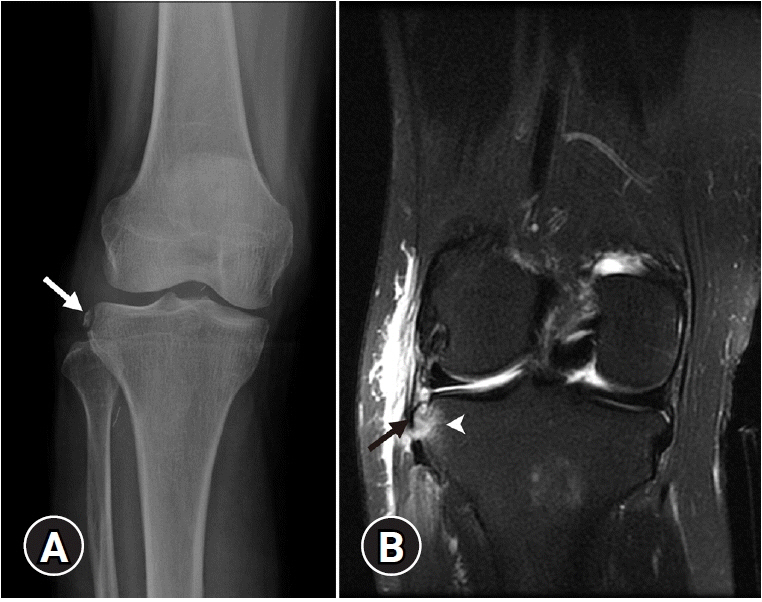
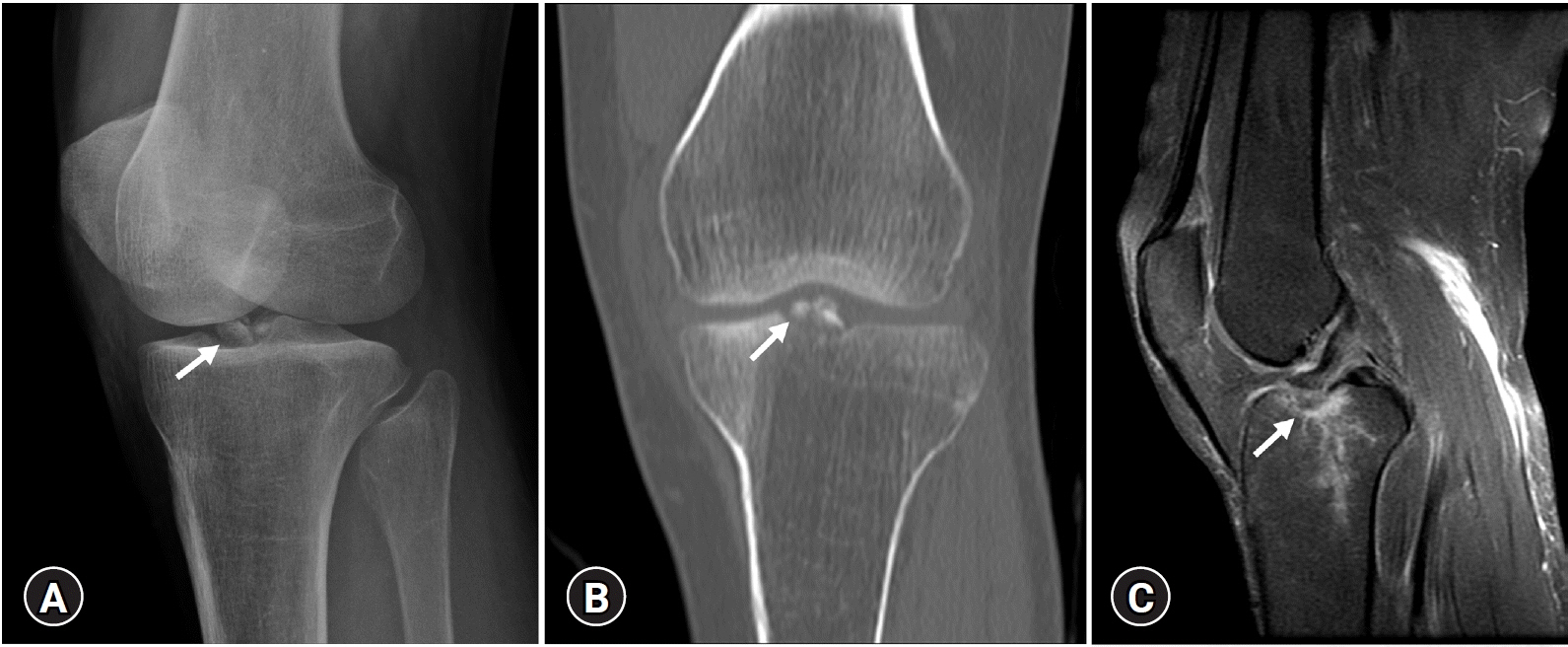
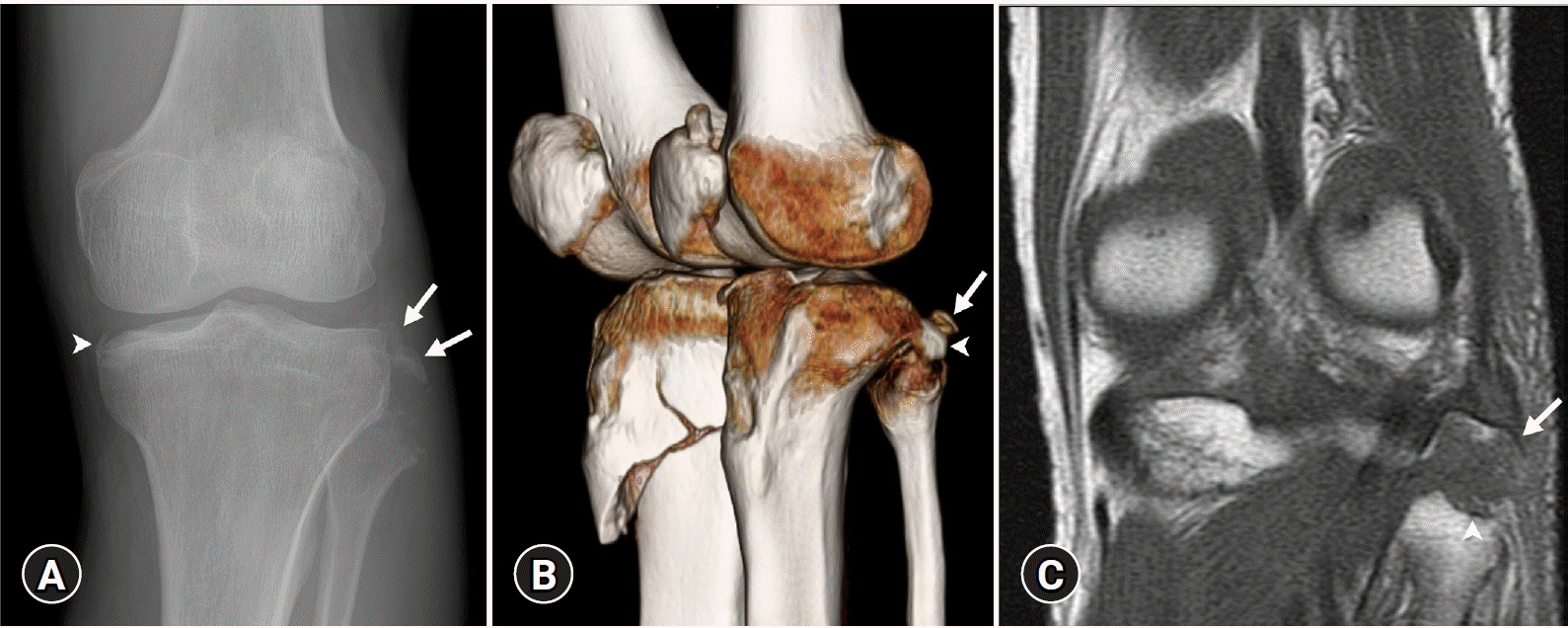
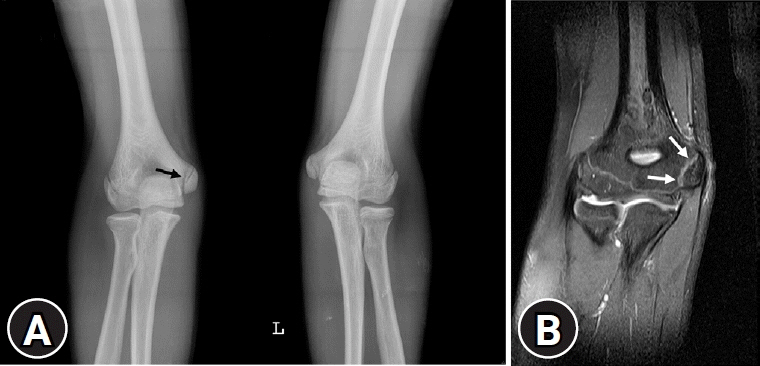
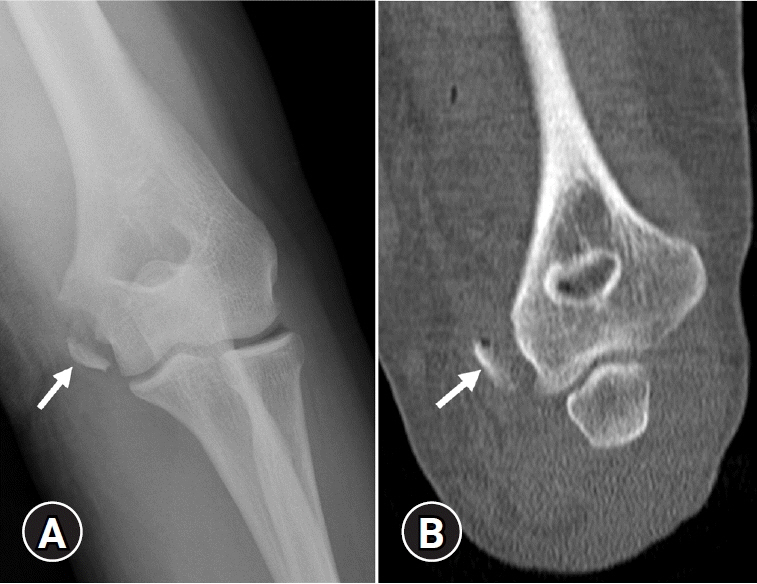
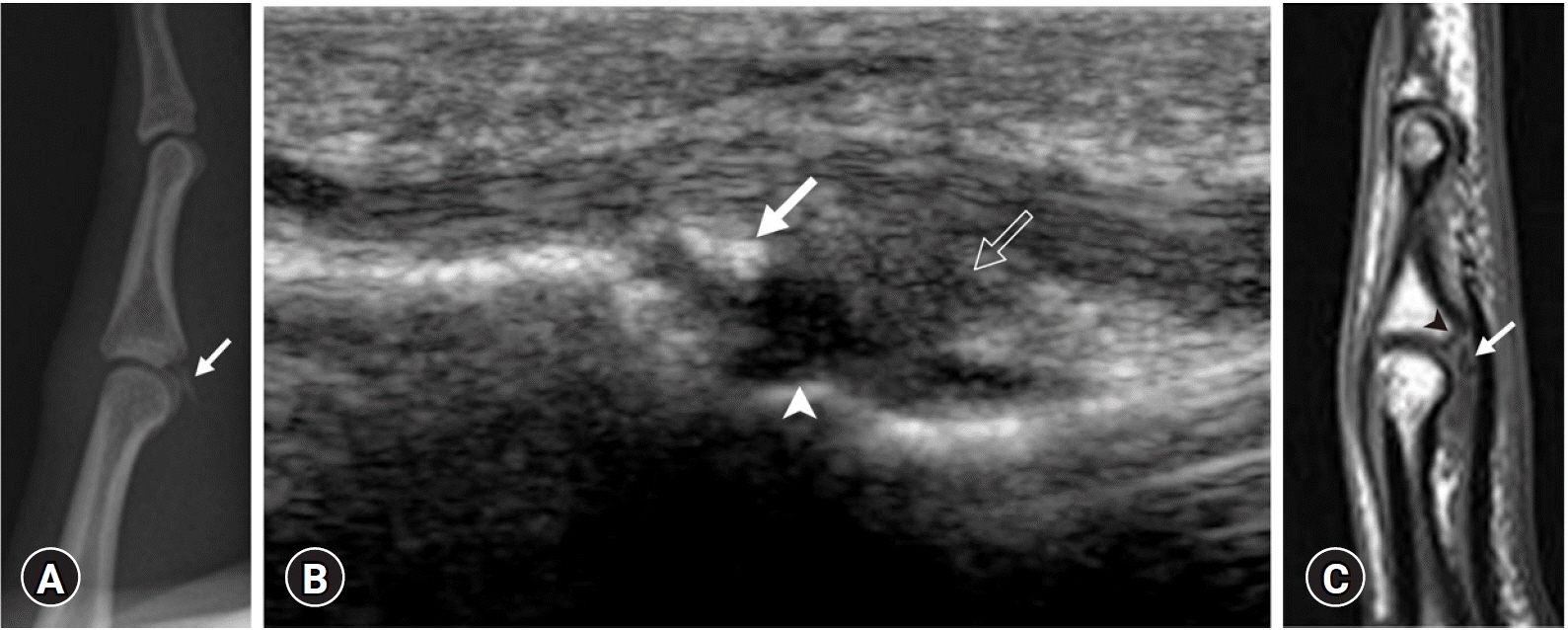
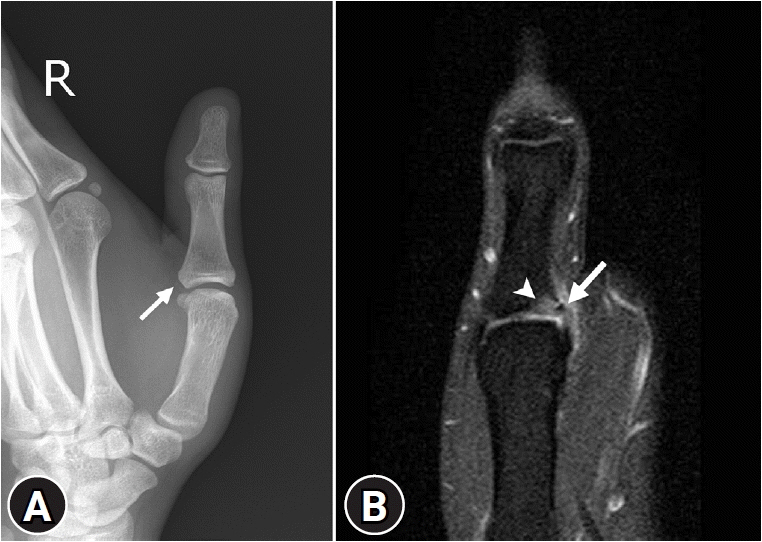
- Avulsion injuries result from the application of a tensile force to a musculoskeletal unit or ligament. Although injuries tend to occur more commonly in skeletally immature populations due to the weakness of their apophysis, adults may also be subject to avulsion fractures, particularly those with osteoporotic bones. The most common sites of avulsion injuries in adolescents and children are apophyses of the pelvis and knee. In adults, avulsion injuries commonly occur within the tendon due to underlying degeneration or tendinosis. However, any location can be involved in avulsion injuries. Radiography is the first imaging modality to diagnose avulsion injury, although advanced imaging modalities are occasionally required to identify subtle lesions or to fully delineate the extent of the injury. Ultrasonography has a high spatial resolution with a dynamic assessment potential and allows the comparison of a bone avulsion with the opposite side. Computed tomography is more sensitive for depicting a tiny osseous fragment located adjacent to the expected attachment site of a ligament, tendon, or capsule. Moreover, magnetic resonance imaging is the best imaging modality for the evaluation of soft tissue abnormalities, especially the affected muscles, tendons, and ligaments. Acute avulsion injuries usually manifest as avulsed bone fragments. In contrast, chronic injuries can easily mimic other disease processes, such as infections or neoplasms. Therefore, recognizing the vulnerable sites and characteristic imaging features of avulsion fractures would be helpful in ensuring accurate diagnosis and appropriate patient management. To this end, familiarity with musculoskeletal anatomy and mechanism of injury is necessary.
Figure
Reference
-
References
1. Stevens MA, El-Khoury GY, Kathol MH, Brandser EA, Chow S. Imaging features of avulsion injuries. Radiographics. 1999; 19:655–72.
Article2. Squires B, Allen PE, Livingstone J, Atkins RM. Fractures of the tuberosity of the calcaneus. J Bone Joint Surg Br. 2001; 83:55–61.
Article3. Sanders TG, Zlatkin MB. Avulsion injuries of the pelvis. Semin Musculoskelet Radiol. 2008; 12:42–53.
Article4. Vandervliet EJ, Vanhoenacker FM, Snoeckx A, Gielen JL, Van Dyck P, Parizel PM. Sports-related acute and chronic avulsion injuries in children and adolescents with special emphasis on tennis. Br J Sports Med. 2007; 41:827–31.
Article5. Lazović D, Wegner U, Peters G, Gossé F. Ultrasound for diagnosis of apophyseal injuries. Knee Surg Sports Traumatol Arthrosc. 1996; 3:234–7.
Article6. Fernbach SK, Wilkinson RH. Avulsion injuries of the pelvis and proximal femur. Am J Roentgenol. 1981; 137:581–4.
Article7. Orava S, Ala-Ketola L. Avulsion fractures in athletes. Br J Sports Med. 1977; 11:65–71.
Article8. Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med. 1985; 13:349–58.
Article9. Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001; 30:127–31.
Article10. Abebe ES, Moorman CT, Garrett WE. Proximal hamstring avulsion injuries: injury mechanism, diagnosis and disease course. Oper Tech Sports Med. 2012; 20:2–6.
Article11. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008; 90:2365–74.
Article12. Brandser EA, el-Khoury GY, Kathol MH, Callaghan JJ, Tearse DS. Hamstring injuries: radiographic, conventional tomographic, CT, and MR imaging characteristics. Radiology. 1995; 197:257–62.
Article13. Ferlic PW, Sadoghi P, Singer G, Kraus T, Eberl R. Treatment for ischial tuberosity avulsion fractures in adolescent athletes. Knee Surg Sports Traumatol Arthrosc. 2014; 22:893–7.
Article14. Schiller J, DeFroda S, Blood T. Lower extremity avulsion fractures in the pediatric and adolescent athlete. J Am Acad Orthop Surg. 2017; 25:251–9.
Article15. Singer G, Eberl R, Wegmann H, Marterer R, Kraus T, Sorantin E. Diagnosis and treatment of apophyseal injuries of the pelvis in adolescents. Semin Musculoskelet Radiol. 2014; 18:498–504.
Article16. Saluan PM, Weiker GG. Avulsion of the anterior inferior iliac spine. Orthopedics. 1997; 20:558–9.
Article17. Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol. 2006; 35:665–72.
Article18. Rajasekhar C, Kumar KS, Bhamra MS. Avulsion fractures of the anterior inferior iliac spine: the case for surgical intervention. Int Orthop. 2001; 24:364–5.
Article19. Hébert KJ, Laor T, Divine JG, Emery KH, Wall EJ. MRI appearance of chronic stress injury of the iliac crest apophysis in adolescent athletes. Am J Roentgenol. 2008; 190:1487–91.
Article20. Steerman JG, Reeder MT, Udermann BE, Pettitt RW, Murray SR. Avulsion fracture of the iliac crest apophysis in a collegiate wrestler. Clin J Sport Med. 2008; 18:102–3.
Article21. Schlegel TF, Bushnell BD, Godfrey J, Boublik M. Success of nonoperative management of adductor longus tendon ruptures in National Football League athletes. Am J Sports Med. 2009; 37:1394–9.
Article22. Ueblacker P, English B, Mueller-Wohlfahrt HW. Nonoperative treatment and return to play after complete proximal adductor avulsion in high-performance athletes. Knee Surg Sports Traumatol Arthrosc. 2016; 24:3927–33.
Article23. O’Rourke MR, Weinstein SL. Osteonecrosis following isolated avulsion fracture of the greater trochanter in children. A report of two cases. J Bone Joint Surg Am. 2003; 85:2000–5.24. James SL, Davies AM. Atraumatic avulsion of the lesser trochanter as an indicator of tumour infiltration. Eur Radiol. 2006; 16:512–4.
Article25. Theologis TN, Epps H, Latz K, Cole WG. Isolated fractures of the lesser trochanter in children. Injury. 1997; 28:363–4.
Article26. Freitas A, Macedo SL Sr. Apophyseal fracture or avulsion of the greater trochanter. Acta Ortop Bras. 2016; 24:164–6.
Article27. Weaver JS, Jacobson JA, Jamadar DA, Hayes CW. Sonographic findings of adductor insertion avulsion syndrome with magnetic resonance imaging correlation. J Ultrasound Med. 2003; 22:403–7.
Article28. Anderson MW, Kaplan PA, Dussault RG. Adductor insertion avulsion syndrome (thigh splints): spectrum of MR imaging features. Am J Roentgenol. 2001; 177:673–5.29. Tshering-Vogel D, Waldherr C, Schindera ST, Steinbach LS, Stauffer E, Anderson SE. Adductor insertion avulsion syndrome, “thigh splints”: relevance of radiological follow-up. Skeletal Radiol. 2005; 34:355–8.
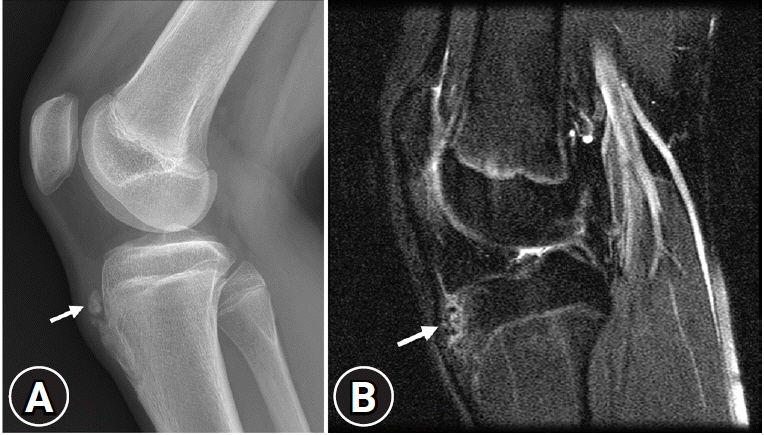
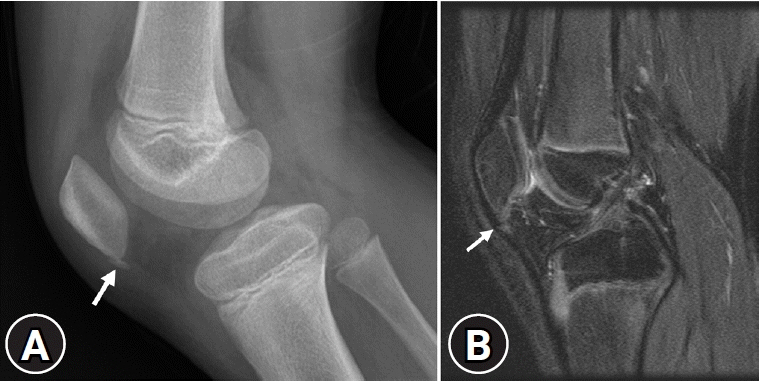
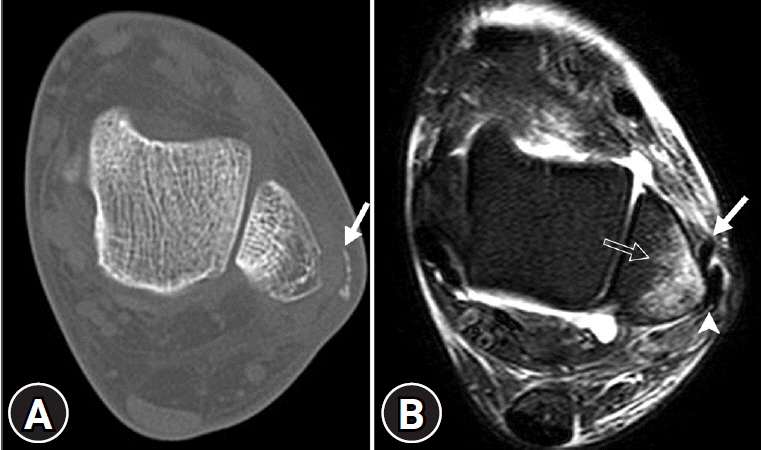
Article30. Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics. 2008; 28:1755–70.
Article31. Hayes CW, Brigido MK, Jamadar DA, Propeck T. Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiographics. 2000; 20 Spec No:S121–34.
Article32. Weber WN, Neumann CH, Barakos JA, Petersen SA, Steinbach LS, Genant HK. Lateral tibial rim (Segond) fractures: MR imaging characteristics. Radiology. 1991; 180:731–4.
Article33. Haims AH, Medvecky MJ, Pavlovich R Jr, Katz LD. MR imaging of the anatomy of and injuries to the lateral and posterolateral aspects of the knee. Am J Roentgenol. 2003; 180:647–53.
Article34. Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J, et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001; 219:381–6.
Article35. Terry GC, Hughston JC, Norwood LA. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986; 14:39–45.
Article36. Porrino J Jr, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS. The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. Am J Roentgenol. 2015; 204:367–73.
Article37. De Maeseneer M, Boulet C, Willekens I, Lenchik L, De Mey J, Cattrysse E, et al. Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skeletal Radiol. 2015; 44:413–21.
Article38. Stallenberg B, Gevenois PA, Sintzoff SA Jr, Matos C, Andrianne Y, Struyven J. Fracture of the posterior aspect of the lateral tibial plateau: radiographic sign of anterior cruciate ligament tear. Radiology. 1993; 187:821–5.
Article39. Ringenberg J, Sealy D, Tiller R. Isolated Segond fracture in a pediatric patient. Phys Sportsmed. 2015; 43:188–91.
Article40. Hall FM, Hochman MG. Medial Segond-type fracture: cortical avulsion off the medial tibial plateau associated with tears of the posterior cruciate ligament and medial meniscus. Skeletal Radiol. 1997; 26:553–5.
Article41. Remer EM, Fitzgerald SW, Friedman H, Rogers LF, Hendrix RW, Schafer MF. Anterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiographics. 1992; 12:901–15.
Article42. Capps GW, Hayes CW. Easily missed injuries around the knee. Radiographics. 1994; 14:1191–210.
Article43. Delzell PB, Schils JP, Recht MP. Subtle fractures about the knee: innocuous-appearing yet indicative of significant internal derangement. Am J Roentgenol. 1996; 167:699–703.
Article44. Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children. A review of 31 cases. J Bone Joint Surg Br. 1992; 74:848–52.
Article45. Recondo JA, Salvador E, Villanúa JA, Barrera MC, Gervás C, Alústiza JM. Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiographics. 2000; 20 Spec No:S91–102.
Article46. Huang GS, Yu JS, Munshi M, Chan WP, Lee CH, Chen CY, et al. Avulsion fracture of the head of the fibula (the “arcuate” sign): MR imaging findings predictive of injuries to the posterolateral ligaments and posterior cruciate ligament. Am J Roentgenol. 2003; 180:381–7.
Article47. Lee J, Papakonstantinou O, Brookenthal KR, Trudell D, Resnick DL. Arcuate sign of posterolateral knee injuries: anatomic, radiographic, and MR imaging data related to patterns of injury. Skeletal Radiol. 2003; 32:619–27.
Article48. Flato R, Passanante GJ, Skalski MR, Patel DB, White EA, Matcuk GR Jr. The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skeletal Radiol. 2017; 46:605–22.
Article49. Bates DG, Hresko MT, Jaramillo D. Patellar sleeve fracture: demonstration with MR imaging. Radiology. 1994; 193:825–7.
Article50. Hunt DM, Somashekar N. A review of sleeve fractures of the patella in children. Knee. 2005; 12:3–7.
Article51. Dupuis CS, Westra SJ, Makris J, Wallace EC. Injuries and conditions of the extensor mechanism of the pediatric knee. Radiographics. 2009; 29:877–86.
Article52. Jalgaonkar AA, Dachepalli S, Al-Wattar Z, Rao S, Kochhar T. Atypical tibial tuberosity fracture in an adolescent. Orthopedics. 2011; 34:215.
Article53. Rosenberg ZS, Kawelblum M, Cheung YY, Beltran J, Lehman WB, Grant AD. Osgood-Schlatter lesion: fracture or tendinitis? Scintigraphic, CT, and MR imaging features. Radiology. 1992; 185:853–8.
Article54. Yablon CM, Pai D, Dong Q, Jacobson JA. Magnetic resonance imaging of the extensor mechanism. Magn Reson Imaging Clin N Am. 2014; 22:601–20.
Article55. Hirano A, Fukubayashi T, Ishii T, Ochiai N. Magnetic resonance imaging of Osgood-Schlatter disease: the course of the disease. Skeletal Radiol. 2002; 31:334–42.
Article56. Ekrol I, Court-Brown CM. Fractures of the base of the 5th metatarsal. Foot. 2004; 14:96–8.
Article57. Gu YD, Ren XJ, Li JS, Lake MJ, Zhang QY, Zeng YJ. Computer simulation of stress distribution in the metatarsals at different inversion landing angles using the finite element method. Int Orthop. 2010; 34:669–76.
Article58. Theodorou DJ, Theodorou SJ, Kakitsubata Y, Botte MJ, Resnick D. Fractures of proximal portion of fifth metatarsal bone: anatomic and imaging evidence of a pathogenesis of avulsion of the plantar aponeurosis and the short peroneal muscle tendon. Radiology. 2003; 226:857–65.
Article59. Polzer H, Polzer S, Mutschler W, Prall WC. Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence. Injury. 2012; 43:1626–32.
Article60. Chuckpaiwong B, Queen RM, Easley ME, Nunley JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008; 466:1966–70.
Article61. Kathol MH, el-Khoury GY, Moore TE, Marsh JL. Calcaneal insufficiency avulsion fractures in patients with diabetes mellitus. Radiology. 1991; 180:725–9.
Article62. Lee SM, Huh SW, Chung JW, Kim DW, Kim YJ, Rhee SK. Avulsion fracture of the calcaneal tuberosity: classification and its characteristics. Clin Orthop Surg. 2012; 4:134–8.
Article63. Yu SM, Yu JS. Calcaneal avulsion fractures: an often forgotten diagnosis. Am J Roentgenol. 2015; 205:1061–7.
Article64. Frame TS. Rockwood & Green’s fractures in adults. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 2023.65. Davis WH, Sobel M, Deland J, Bohne WH, Patel MB. The superior peroneal retinaculum: an anatomic study. Foot Ankle Int. 1994; 15:271–5.
Article66. Rosenberg ZS, Bencardino J, Astion D, Schweitzer ME, Rokito A, Sheskier S. MRI features of chronic injuries of the superior peroneal retinaculum. Am J Roentgenol. 2003; 181:1551–7.
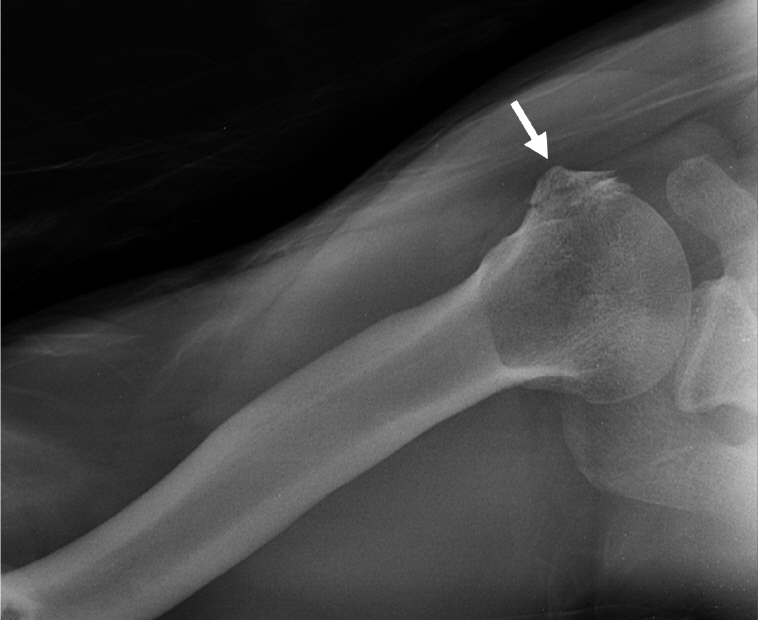
Article67. Bahrs C, Lingenfelter E, Fischer F, Walters EM, Schnabel M. Mechanism of injury and morphology of the greater tuberosity fracture. J Shoulder Elbow Surg. 2006; 15:140–7.
Article68. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003; 12:641–9.
Article69. Pace A, Ribbans W, Kim JH. Isolated lesser tuberosity fracture of the humerus. Orthopedics. 2008; 31:94.
Article70. Earwaker J. Isolated avulsion fracture of the lesser tuberosity of the humerus. Skeletal Radiol. 1990; 19:121–5.
Article71. van Laarhoven HA, te Slaa RL, van Laarhoven EW. Isolated avulsion fracture of the lesser tuberosity of the humerus. J Trauma. 1995; 39:997–9.
Article72. Levine B, Pereira D, Rosen J. Avulsion fractures of the lesser tuberosity of the humerus in adolescents: review of the literature and case report. J Orthop Trauma. 2005; 19:349–52.73. Wenzke DR. MR imaging of the elbow in the injured athlete. Radiol Clin North Am. 2013; 51:195–213.
Article74. Iyer RS, Thapa MM, Khanna PC, Chew FS. Pediatric bone imaging: imaging elbow trauma in children: a review of acute and chronic injuries. Am J Roentgenol. 2012; 198:1053–68.75. Crowther M. Elbow pain in pediatrics. Curr Rev Musculoskelet Med. 2009; 2:83–7.
Article76. Rajasekhar C, Kakarlapudi TK, Bhamra MS. Avulsion of the triceps tendon. Emerg Med J. 2002; 19:271–2.
Article77. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009; 40:575–81.
Article78. Delgado J, Jaramillo D, Chauvin NA. Imaging the injured pediatric athlete: upper extremity. Radiographics. 2016; 36:1672–87.
Article79. Woods GW, Tullos HS. Elbow instability and medial epicondyle fractures. Am J Sports Med. 1977; 5:23–30.
Article80. Kobayashi Y, Oka Y, Ikeda M, Munesada S. Avulsion fracture of the medial and lateral epicondyles of the humerus. J Shoulder Elbow Surg. 2000; 9:59–64.
Article81. Dodds SD, Flanagin BA, Bohl DD, DeLuca PA, Smith BG. Incarcerated medial epicondyle fracture following pediatric elbow dislocation: 11 cases. J Hand Surg Am. 2014; 39:1739–45.
Article82. Kang R, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Am Soc Surg Hand. 2002; 2:47–59.
Article83. Freiberg A, Pollard BA, Macdonald MR, Duncan MJ. Management of proximal interphalangeal joint injuries. J Trauma. 1999; 46:523–8.
Article84. Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clin J Sport Med. 2010; 20:106–12.
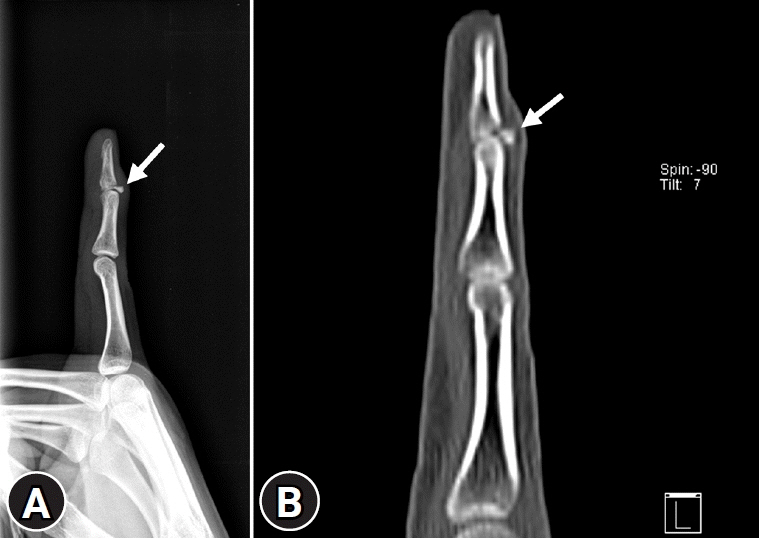
Article85. Simpson D, McQueen MM, Kumar P. Mallet deformity in sport. J Hand Surg Br. 2001; 26:32–3.
Article86. Aronowitz ER, Leddy JP. Closed tendon injuries of the hand and wrist in athletes. Clin Sports Med. 1998; 17:449–67.
Article87. Blair WF, Steyers CM. Extensor tendon injuries. Orthop Clin North Am. 1992; 23:141–8.
Article88. Cheung JP, Fung B, Ip WY. Review on mallet finger treatment. Hand Surg. 2012; 17:439–47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Friction Avulsion Injuries of the Foot: Report of 6 Cases
- Avulsion Fracture of the Calcaneal Tuberosity: 2 Cases Report
- MR Imaging Findings of Avulsion Fracture of the Tibial Spine of the Knee, Focusing on Cruciate Ligament Tear
- Isolated Avulsion Fracture of the Superior Border of the Scapula: A Case Report
- Tratment of the Nail Bed Avulsion Injury with Split-thickness Nail Bed Graft