J Korean Med Sci.
2021 Oct;36(41):e291. 10.3346/jkms.2021.36.e291.
Non-alcoholic Fatty Liver Disease and COVID-19 Susceptibility and Outcomes: a Korean Nationwide Cohort
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 2Department of Data Science, Sejong University College of Software Convergence, Seoul, Korea
- 3Department of Pediatrics, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Internal Medicine I, Gastroenterology, Hepatology, Endocrinology and Metabolism, Medical University of Innsbruck, Innsbruck, Austria
- 5Department of Pediatrics, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
- 6Department of Otorhinolaryngology-Head & Neck Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 7Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 8Genomics and Digital Health, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 9Korea University College of Medicine, Seoul, Korea
- 10Catalan Institution for Research and Advanced Studies (ICREA), Pg. Lluis Companys, Barcelona, Spain
- 11Research and Development Unit, Parc Sanitari Sant Joan de Déu, CIBERSAM, Barcelona, Spain
- 12Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid, Spain
- 13Faculty of Medicine, University of Versailles Saint-Quentin-en-Yvelines, Montigny-le-Bretonneux, France
- 14The Cambridge Centre for Sport and Exercise Sciences, Anglia Ruskin University, Cambridge, UK
- 15Department of Gastroenterology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 16Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2521474
- DOI: http://doi.org/10.3346/jkms.2021.36.e291
Abstract
- Background
Evidence for the association between underlying non-alcoholic fatty liver disease (NAFLD), the risk of testing severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) positive, and the clinical consequences of coronavirus disease 2019 (COVID-19) is controversial and scarce. We aimed to investigate the association between the presence of NAFLD and the risk of SARS-CoV-2 infectivity and COVID-19-related outcomes.
Methods
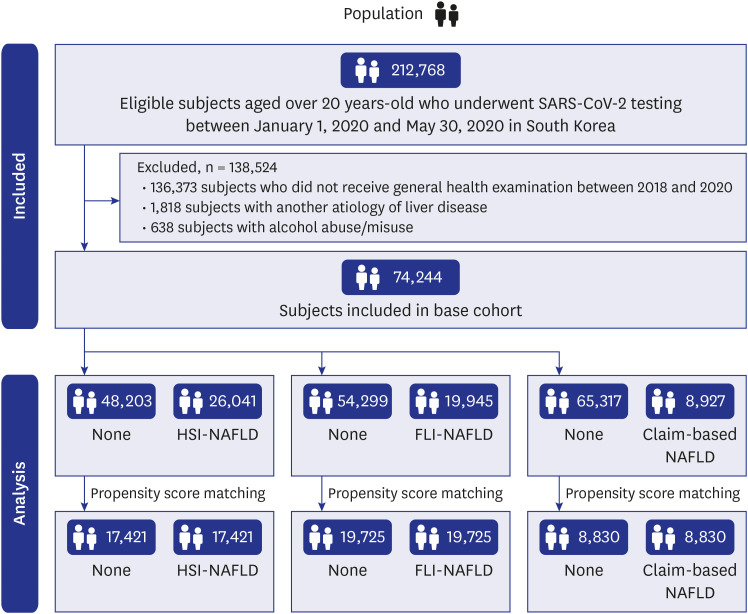
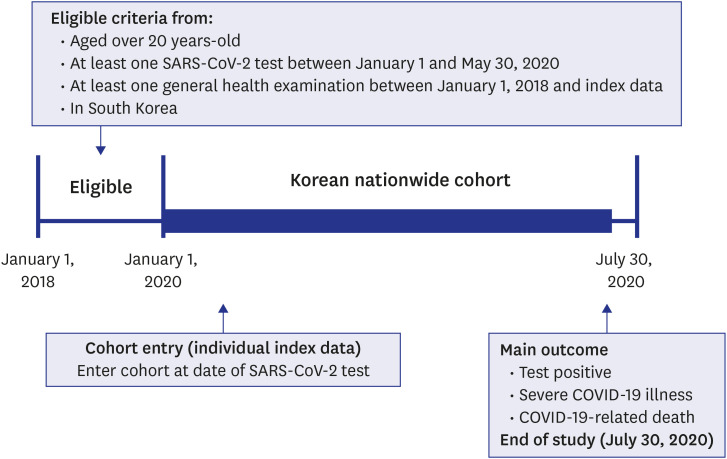
We used the population-based, nationwide cohort in South Korea linked with the general health examination records between January 1, 2018 and July 30, 2020. Data for 212,768 adults older than 20 years who underwent SARS-CoV-2 testing from January 1 to May 30, 2020, were obtained. The presence of NAFLDs was defined using three definitions, namely hepatic steatosis index (HSI), fatty liver index (FLI), and claims-based definition. The outcomes were SARS-CoV-2 test positive, COVID-19 severe illness, and related death.
Results
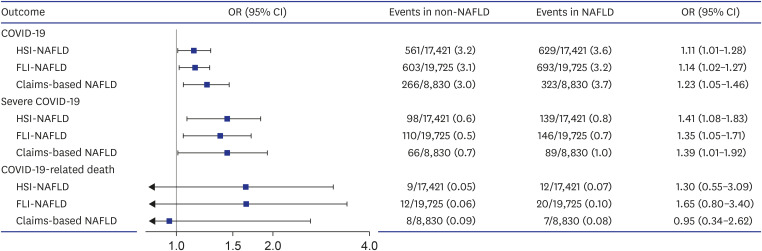
Among 74,244 adults who completed the general health examination, there were 2,251 (3.0%) who were SARS-CoV-2 positive, 438 (0.6%) with severe COVID-19 illness, and 45 (0.06%) COVID-19-related deaths. After exposure-driven propensity score matching, patients with pre-existing HSI-NAFLD, FLI-NAFLD, or claims-based NAFLD had an 11–23% increased risk of SARS-CoV-2 infection (HSI-NAFLD 95% confidence interval [CI], 1–28%; FLI-NAFLD 95% CI, 2–27%; and claims-based NAFLD 95% CI, 2–31%) and a 35–41% increased risk of severe COVID-19 illness (HSI-NAFLD 95% CI, 8–83%; FLI-NAFLD 95% CI, 5–71%; and claims-based NAFLD 95% CI, 1–92%). These associations are more evident as liver fibrosis advanced (based on the BARD scoring system). Similar patterns were observed in several sensitivity analyses including the full-unmatched cohort.
Conclusion
Patients with pre-existing NAFLDs have a higher likelihood of testing SARSCoV-2 positive and severe COVID-19 illness; this association was more evident in patients with NAFLD with advanced fibrosis. Our results suggest that extra attention should be given to the management of patients with NAFLD during the COVID-19 pandemic.
Keyword
Figure
Reference
-
1. Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020; 7(12):1025–1031. PMID: 32950066.
Article2. Kim MS, Jung SY, Lee SW, Li H, Koyanagi A, Kronbichler A, et al. Hepatobiliary adverse drug reactions associated with remdesivir: the WHO international pharmacovigilance study. Clin Gastroenterol Hepatol. 2021; 19(9):1970–1972.e3. PMID: 33940227.
Article3. Saviano A, Wrensch F, Ghany MG, Baumert TF. Liver disease and coronavirus disease 2019: from pathogenesis to clinical care. Hepatology. 2021; 74(2):1088–1100. PMID: 33332624.
Article4. Iavarone M, D'Ambrosio R, Soria A, Triolo M, Pugliese N, Del Poggio P, et al. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J Hepatol. 2020; 73(5):1063–1071. PMID: 32526252.
Article5. Meijnikman AS, Bruin S, Groen AK, Nieuwdorp M, Herrema H. Increased expression of key SARS-CoV-2 entry points in multiple tissues in individuals with NAFLD. J Hepatol. 2021; 74(3):748–749. PMID: 33338513.
Article6. Singh S, Khan A. Clinical characteristics and outcomes of coronavirus disease 2019 among patients with preexisting liver disease in the United States: a multicenter research network study. Gastroenterology. 2020; 159(2):768–771.e3. PMID: 32376408.
Article7. Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. 2019; 71(4):793–801. PMID: 31279902.
Article8. Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol. 2021; 3(10):e698–e706. PMID: 34179832.
Article9. Lagana SM, Kudose S, Iuga AC, Lee MJ, Fazlollahi L, Remotti HE, et al. Hepatic pathology in patients dying of COVID-19: a series of 40 cases including clinical, histologic, and virologic data. Mod Pathol. 2020; 33(11):2147–2155. PMID: 32792598.
Article10. Lazarus JV, Colombo M, Cortez-Pinto H, Huang TT, Miller V, Ninburg M, et al. NAFLD - sounding the alarm on a silent epidemic. Nat Rev Gastroenterol Hepatol. 2020; 17(7):377–379. PMID: 32514153.
Article11. Woo A, Lee SW, Koh HY, Kim MA, Han MY, Yon DK. Incidence of cancer after asthma development: 2 independent population-based cohort studies. J Allergy Clin Immunol. 2021; 147(1):135–143. PMID: 32417133.
Article12. Lee SW, Lee J, Moon SY, Jin HY, Yang JM, Ogino S, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. Forthcoming. 2021; DOI: 10.1136/bjsports-2021-104203.
Article13. Lee SW, Yang JM, Moon SY, Kim N, Ahn YM, Kim JM, et al. Association between mental illness and COVID-19 in South Korea: a post-hoc analysis. Lancet Psychiatry. 2021; 8(4):271–272. PMID: 33617761.
Article14. Yang JM, Koh HY, Moon SY, Yoo IK, Ha EK, You S, et al. Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol. 2020; 146(4):790–798. PMID: 32810517.15. Yoo HW, Shin JI, Yon DK, Lee SW. COVID-19 morbidity and severity in patients with nonalcoholic fatty liver disease in South Korea: a nationwide cohort study. Clin Gastroenterol Hepatol. Forthcoming. 2021; DOI: 10.1016/j.cgh.2021.07.031.
Article16. Lee SW, Ha EK, Yeniova AÖ, Moon SY, Kim SY, Koh HY, et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. Gut. 2021; 70(1):76–84. PMID: 32732368.
Article17. Ha J, Lee SW, Yon DK. Ten-year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017. Clin Exp Pediatr. 2020; 63(7):278–283. PMID: 32023407.
Article18. Lee SW, Kim SY, Moon SY, Yang JM, Ha EK, Jee HM, et al. Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study. J Allergy Clin Immunol Pract. 2021; 9(6):2262–2271.e2. PMID: 33931377.
Article19. Boursier J, Shreay S, Fabron C, Torreton E, Fraysse J. Hospitalization costs and risk of mortality in adults with nonalcoholic steatohepatitis: analysis of a French national hospital database. EClinicalMedicine. 2020; 25:100445. PMID: 32775971.
Article20. Chen LD, Huang JF, Chen QS, Lin GF, Zeng HX, Lin XF, et al. Validation of fatty liver index and hepatic steatosis index for screening of non-alcoholic fatty liver disease in adults with obstructive sleep apnea hypopnea syndrome. Chin Med J (Engl). 2019; 132(22):2670–2676. PMID: 31765354.
Article21. Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008; 57(10):1441–1447. PMID: 18390575.
Article22. Lee SW, Yang JM, Yoo IK, Moon SY, Ha EK, Yeniova AÖ, et al. Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort. Gut. 2021; 70(10):2013–2015. PMID: 33303566.
Article23. Mushtaq K, Khan MU, Iqbal F, Alsoub DH, Chaudhry HS, Ata F, et al. NAFLD is a predictor of liver injury in COVID-19 hospitalized patients but not of mortality, disease severity on the presentation or progression - The debate continues. J Hepatol. 2021; 74(2):482–484. PMID: 33223215.
Article24. Sachdeva S, Khandait H, Kopel J, Aloysius MM, Desai R, Goyal H. NAFLD and COVID-19: a pooled analysis. SN Compr Clin Med. 2020; 1–4.
Article25. Forlano R, Mullish BH, Mukherjee SK, Nathwani R, Harlow C, Crook P, et al. In-hospital mortality is associated with inflammatory response in NAFLD patients admitted for COVID-19. PLoS One. 2020; 15(10):e0240400. PMID: 33031439.
Article26. Huang R, Zhu L, Wang J, Xue L, Liu L, Yan X, et al. Clinical features of COVID-19 patients with non-alcoholic fatty liver disease. Hepatol Commun. 2020; 4(12):1758–1768.27. Campos-Murguía A, Román-Calleja BM, Toledo-Coronado IV, González-Regueiro JA, Solís-Ortega AA, Kúsulas-Delint D, et al. Liver fibrosis in patients with metabolic associated fatty liver disease is a risk factor for adverse outcomes in COVID-19. Dig Liver Dis. 2021; 53(5):525–533. PMID: 33551355.
Article28. Targher G, Mantovani A, Byrne CD, Wang XB, Yan HD, Sun QF, et al. Detrimental effects of metabolic dysfunction-associated fatty liver disease and increased neutrophil-to-lymphocyte ratio on severity of COVID-19. Diabetes Metab. 2020; 46(6):505–507. PMID: 32505652.
Article29. Sohrabi Y, Reinecke H, Godfrey R. Altered cholesterol and lipid synthesis mediates hyperinflammation in COVID-19. Trends Endocrinol Metab. 2021; 32(3):132–134. PMID: 33455862.
Article30. Nardo AD, Schneeweiss-Gleixner M, Bakail M, Dixon ED, Lax SF, Trauner M. Pathophysiological mechanisms of liver injury in COVID-19. Liver Int. 2021; 41(1):20–32. PMID: 33190346.
Article31. Kukla M, Skonieczna-Żydecka K, Kotfis K, Maciejewska D, Łoniewski I, Lara LF, et al. COVID-19, MERS and SARS with concomitant liver injury-systematic review of the existing literature. J Clin Med. 2020; 9(5):1420.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Should you advocate for hepatocellular carcinomasurveillance in patients with alcohol-related liverdisease or non-alcoholic fatty liver disease?
- Correspondence on Letter regarding “COVID-19 vaccine immunogenicity among chronic liver disease patients and liver transplant recipients: A meta-analysis”
- How to optimize the outcome of liver transplantation for non-alcoholic fatty liver disease
- A Case of Hepatocellular Carcinoma in Non-alcoholic Fatty Liver Disease
- Are patients with alcohol-related fatty liver at increased risk of coronary heart disease?