J Korean Med Sci.
2021 Oct;36(41):e251. 10.3346/jkms.2021.36.e251.
The Distribution of Multidrugresistant Microorganisms and Treatment Status of Hospital-acquired Pneumonia/Ventilator-associated Pneumonia in Adult Intensive Care Units: a Prospective Cohort Observational Study
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, College of Medicine Inje University Sanggye Paik Hospital, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 5Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Infectious Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 7Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2521469
- DOI: http://doi.org/10.3346/jkms.2021.36.e251
Abstract
- Background
It is essential to determine the distribution of the causative microorganisms in the region and the status of local antibiotic resistance for the proper treatment of hospitalacquired pneumonia/ventilator-associated pneumonia (HAP/VAP). This study aimed to investigate the occurrence and causative strains of HAP/VAP, distribution of resistant bacteria, use of antibiotics, and the ensuing outcomes of patients in Korea.
Methods
A multicenter prospective observational cohort study was conducted among patients with HAP/VAP admitted to the medical intensive care unit of 5 tertiary referral centers between August 2012 and June 2015. Patients' demographic and clinical data were collected.
Results
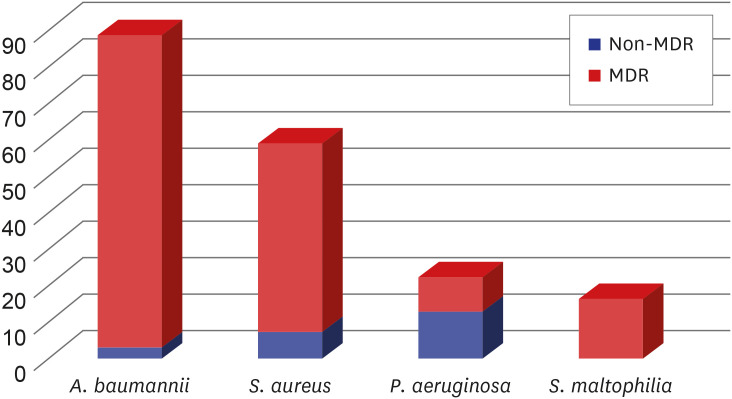
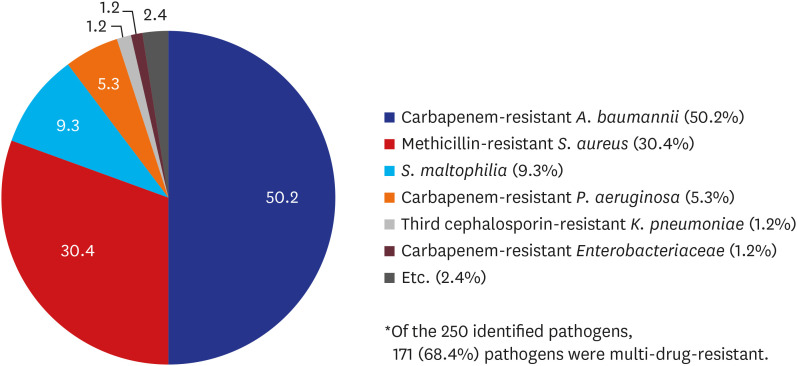
A total of 381 patients were diagnosed with HAP/VAP. Their median age was 69 (59–76) years and 71% were males. A majority of the patients (88%) had late-onset (> 5 days) HAP/VAP. One-quarter of the patients (n = 99) had at least one risk factor for multidrug-resistant (MDR) pathogens, such as prior intravenous antibiotic use within the last 90 days. Microbiological specimens were mostly obtained noninvasively (87%) using sputum or endotracheal aspirates. Pathogens were identified in 235 (62%) of the 381 patients. The most common bacterial pathogen was Acinetobacter baumannii (n = 89), followed by Staphylococcus aureus (n = 52), Klebsiella pneumoniae (n = 25) and Pseudomonas aeruginosa (n = 22). Most of isolated A. baumannii (97%) and S. aureus (88%) were multidrug resistant. The most commonly used empirical antibiotic regimens were carbapenem-based antibiotics (38%), followed by extended-spectrum penicillin/ β-lactamase inhibitor (34%). Glycopeptide or linezolid were also used in combination in 54% of patients. The 28-day mortality rate of the patients with HAP/VAP was 30% and the 60-day mortality was 46%. Patients who used empirical antibiotics appropriately had significantly lower mortality rates than those who did not (28-day mortality: 25% vs. 40%, P = 0.032; 60-day mortality: 41% vs. 55%, P = 0.032, respectively). Administration of appropriate empirical antibiotics (odds ratio [OR], 0.282; confidence interval [CI], 0.092–0.859; P = 0.026), Day 7 treatment failure (OR, 4.515; CI, 1.545–13.192; P= 0.006), and APACHE II score on day 1 (OR, 1.326; CI, 0.988–1.779; P = 0.012) were the factors that determined the 28-day mortality in patients with HAP who had identified bacteria as pathogens.
Conclusion
In HAP/VAP patients, there was a large burden of MDR pathogens, and their associated mortality rate was high. Proper selection of empirical antibiotics was significantly associated with the patient's prognosis; however, there was a discrepancy between major pathogens and empirical antibiotic therapy.
Keyword
Figure
Reference
-
1. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005; 171(4):388–416. PMID: 15699079.2. Falagas ME, Bliziotis IA, Siempos II. Attributable mortality of Acinetobacter baumannii infections in critically ill patients: a systematic review of matched cohort and case-control studies. Crit Care. 2006; 10(2):R48. PMID: 16563184.3. Agrafiotis M, Siempos II, Ntaidou TK, Falagas ME. Attributable mortality of ventilator-associated pneumonia: a meta-analysis. Int J Tuberc Lung Dis. 2011; 15(9):1154–1163. PMID: 21669028.
Article4. Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014; 370(13):1198–1208. PMID: 24670166.
Article5. Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. A novel algorithm to analyze epidemiology and outcomes of carbapenem resistance among patients with hospital-acquired and ventilator-associated pneumonia: a retrospective cohort study. Chest. 2019; 155(6):1119–1130. PMID: 30685333.6. Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005; 33(10):2184–2193. PMID: 16215368.
Article7. Beardsley JR, Williamson JC, Johnson JW, Ohl CA, Karchmer TB, Bowton DL. Using local microbiologic data to develop institution-specific guidelines for the treatment of hospital-acquired pneumonia. Chest. 2006; 130(3):787–793. PMID: 16963676.
Article8. Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016; 63(5):e61–111. PMID: 27418577.9. Lee JK, Lee J, Park YS, Lee CH, Yim JJ, Yoo CG, et al. Clinical manifestations of pneumonia according to the causative organism in patients in the intensive care unit. Korean J Intern Med. 2015; 30(6):829–836. PMID: 26552458.
Article10. Kwak YG, Choi JY, Yoo H, Lee SO, Kim HB, Han SH, et al. Korean National Healthcare-associated Infections Surveillance System, intensive care unit module report: summary of data from July 2014 through June 2015. Korean J Healthc Assoc Infect Control Prev. 2016; 21(2):37–49.
Article11. Kim JM, Park ES, Jeong JS, Kim KM, Kim JM, Oh HS, et al. Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Am J Infect Control. 2000; 28(6):454–458. PMID: 11114615.
Article12. Chung DR, Song JH, Kim SH, Thamlikitkul V, Huang SG, Wang H, et al. High prevalence of multidrug-resistant nonfermenters in hospital-acquired pneumonia in Asia. Am J Respir Crit Care Med. 2011; 184(12):1409–1417. PMID: 21920919.
Article13. Koulenti D, Lisboa T, Brun-Buisson C, Krueger W, Macor A, Sole-Violan J, et al. Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit Care Med. 2009; 37(8):2360–2368. PMID: 19531951.
Article14. Lambert ML, Suetens C, Savey A, Palomar M, Hiesmayr M, Morales I, et al. Clinical outcomes of health-care-associated infections and antimicrobial resistance in patients admitted to European intensive-care units: a cohort study. Lancet Infect Dis. 2011; 11(1):30–38. PMID: 21126917.
Article15. Higgins PG, Dammhayn C, Hackel M, Seifert H. Global spread of carbapenem-resistant Acinetobacter baumannii . J Antimicrob Chemother. 2010; 65(2):233–238. PMID: 19996144.16. Villar M, Cano ME, Gato E, Garnacho-Montero J, Miguel Cisneros J, Ruíz de Alegría C, et al. Epidemiologic and clinical impact of Acinetobacter baumannii colonization and infection: a reappraisal. Medicine (Baltimore). 2014; 93(5):202–210. PMID: 25181313.17. Kollef KE, Schramm GE, Wills AR, Reichley RM, Micek ST, Kollef MH. Predictors of 30-day mortality and hospital costs in patients with ventilator-associated pneumonia attributed to potentially antibiotic-resistant gram-negative bacteria. Chest. 2008; 134(2):281–287. PMID: 18682456.
Article18. Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. Multidrug resistance, inappropriate empiric therapy, and hospital mortality in Acinetobacter baumannii pneumonia and sepsis. Crit Care. 2016; 20(1):221. PMID: 27417949.
Article19. Zilberberg MD, Shorr AF, Micek ST, Vazquez-Guillamet C, Kollef MH. Multi-drug resistance, inappropriate initial antibiotic therapy and mortality in Gram-negative severe sepsis and septic shock: a retrospective cohort study. Crit Care. 2014; 18(6):596. PMID: 25412897.
Article20. Rello J, Ulldemolins M, Lisboa T, Koulenti D, Mañez R, Martin-Loeches I, et al. Determinants of prescription and choice of empirical therapy for hospital-acquired and ventilator-associated pneumonia. Eur Respir J. 2011; 37(6):1332–1339. PMID: 20847075.
Article21. Kalanuria AA, Ziai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014; 18(2):208. PMID: 25029020.
Article22. Torres A, Sibila O, Ferrer M, Polverino E, Menendez R, Mensa J, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015; 313(7):677–686. PMID: 25688779.
Article23. Wang L, Li X, Yang Z, Tang X, Yuan Q, Deng L, et al. Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation. Cochrane Database Syst Rev. 2016; 2016(1):CD009946.
Article24. Coppadoro A, Bellani G, Foti G. Non-pharmacological interventions to prevent ventilator-associated pneumonia: a literature review. Respir Care. 2019; 64(12):1586–1595. PMID: 31551284.
Article25. Park SY, Lee HB. Prevention and management of ventilator-associated pneumonia. Korean J Med. 2014; 86(5):537–545.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention and Management of Ventilator-Associated Pneumonia
- Impact of the Ventilator-associated Pneumonia Bundle in a Medical Intensive Care Unit
- Respiratory Review of 2012: Pneumonia
- Role of Microbiologic Culture Results of Specimens Prior to Onset of Ventilator-Associated Pneumonia in the Patients Admitted to Intensive Care Unit
- The Incidence Rate of Ventilator Associated Pneumonia in Relation to the Exchange of Circuit Cycle