J Liver Cancer.
2021 Sep;21(2):181-186. 10.17998/jlc.2021.09.08.
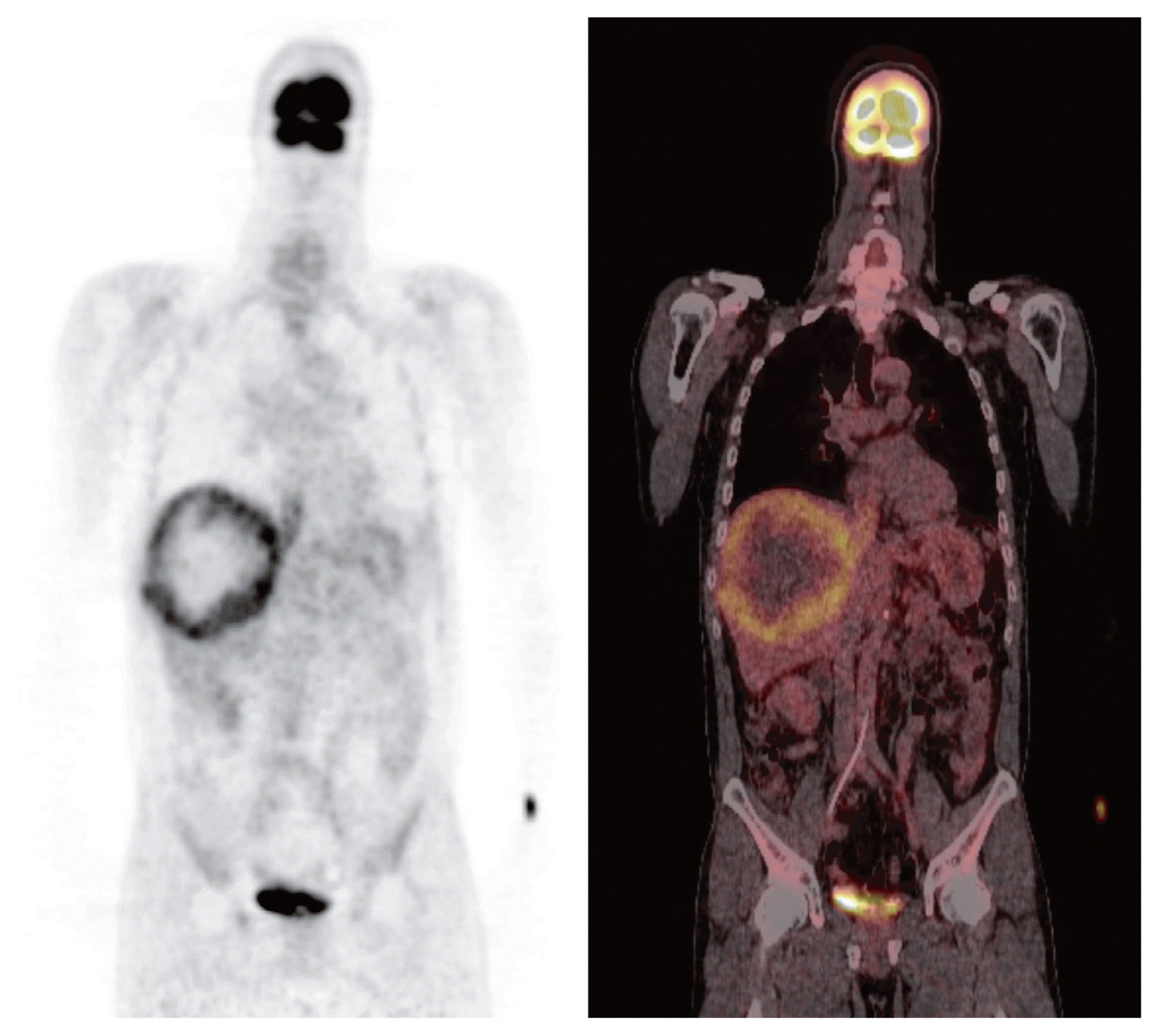
Curative liver transplantation after lung resection for advanced hepatocellular carcinoma with lung metastasis and inferior vena cava tumor thrombosis: a case report
- Affiliations
-
- 1Department of Surgery, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- 2The Research Institute for Transplantation, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2520906
- DOI: http://doi.org/10.17998/jlc.2021.09.08
Abstract
- Hepatocellular carcinoma (HCC) with distant metastasis is an absolute contraindication for liver transplantation (LT). However, it is still unclear whether LT is feasible or acceptable in such patients, albeit after being treated with a multidisciplinary approach and after any metastatic lesion is ruled out. We report one such successful treatment with living donor LT (LDLT) after completely controlling far-advanced HCC with inferior vena cava tumor thrombosis and multiple lung metastases. The patient has been doing well without HCC recurrence for eight years since LDLT. The current patient could be an anecdotal case, but provides a case for expanding LDLT indications in the context of advanced HCC and suchlike.
Keyword
Figure
Reference
-
References
1. Kaido T, Mori A, Ogura Y, Hata K, Yoshizawa A, Iida T, et al. Recurrence of hepatocellular carcinoma after living donor liver transplantation: what is the current optimal approach to prevent recurrence? World J Surg. 2011; 35:1355–1359.2. Mazzaferro V, Bhoori S, Sposito C, Bongini M, Langer M, Miceli R, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 2011; 17(Suppl 2):S44–57.3. Lingiah VA, Niazi M, Olivo R, Paterno F, Guarrera JV, Pyrsopoulos NT. Liver transplantation beyond Milan criteria. J Clin Transl Hepatol. 2020; 8:69–75.4. Han KH, Seong J, Kim JK, Ahn SH, Lee DY, Chon CY. Pilot clinical trial of localized concurrent chemoradiation therapy for locally advanced hepatocellular carcinoma with portal vein thrombosis. Cancer. 2008; 113:995–1003.5. Elshamy M, Aucejo F, Menon KV, Eghtesad B. Hepatocellular carcinoma beyond Milan criteria: Management and transplant selection criteria. World J Hepatol. 2016; 8:874–880.6. Yoshizumi T, Shirabe K, Mori M. It is time to abandon the Milan criteria. Hepatobiliary Surg Nutr. 2019; 8:56–58.7. Ho CM, Hu RH. Comment on “Is it time to abandon the Milan criteria?”. Ann Surg. 2019; 270:e85.8. Xu X, Lu D, Ling Q, Wei X, Wu J, Zhou L, et al. Liver transplantation for hepatocellular carcinoma beyond the Milan criteria. Gut. 2016; 65:1035–1041.9. Han DH, Joo DJ, Kim MS, Choi GH, Choi JS, Park YN, et al. Living donor liver transplantation for advanced hepatocellular carcinoma with portal vein tumor thrombosis after concurrent chemoradiation therapy. Yonsei Med J. 2016; 57:1276–1281.10. De Carlis L, Di Sandro S, Giacomoni A, Slim A, Lauterio A, Mangoni I, et al. Beyond the Milan criteria: what risks for patients with hepatocellular carcinoma progression before liver transplantation? J Clin Gastroenterol. 2012; 46:78–86.11. Lee WH, Byun HK, Choi JS, Choi GH, Han DH, Joo DJ, et al. Liver-directed combined radiotherapy as a bridge to curative surgery in locally advanced hepatocellular carcinoma beyond the Milan criteria. Radiother Oncol. 2020; 152:1–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatocellular Carcinoma Metastatic to Brain
- Anesthetic Management for Liver Segmentectomy and Thrombectomy of Inferior Vena Cava and Right Atrium without Cardiopulmonary Bypass : A case report
- Hepatocellular Carcinoma Extending to the Inferior Vena Cava and Right Atrium-A Case Report of 4 Years Survival after Repeated Transcatheter Arterial Chemoembolization Therapy -
- Renal Cell Carcinoma with Deep Vein Thrombosis
- Small Renal Cell Carcinoma Associated with Inferior Vena Cava Thrombus