Obstet Gynecol Sci.
2021 Sep;64(5):393-406. 10.5468/ogs.21040.
Sonographic evaluation of fetal scrotum, testes and epididymis
- Affiliations
-
- 1Prenatal Diagnosis Unit, Department of Obstetrics, Hospital General Universitario Santa Lucía, Cartagena, Spain
- KMID: 2520260
- DOI: http://doi.org/10.5468/ogs.21040
Abstract
- External male genitalia have rarely been evaluated on fetal ultrasound. Apart from visualization of the penis for fetal sex determination, there are no specific instructions or recommendations from scientific societies. This study aimed to review the current knowledge about prenatal diagnosis of the scrotum and internal structures, with discussion regarding technical aspects and clinical management. We conducted an article search in Medline, EMBASE, Scopus, Google Scholar, and Web of Science databases for studies in English or Spanish language that discussed prenatal scrotal pathologies. We identified 72 studies that met the inclusion criteria. Relevant data were grouped into sections of embryology, ultrasound, pathology, and prenatal diagnosis. The scrotum and internal structures show a wide range of pathologies, with varying degrees of prevalence and morbidity. Most of the reported cases have described incidental findings diagnosed via striking ultrasound signs. Studies discussing normative data or management are scarce.
Figure
Reference
-
References
1. Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Hernandez-Andrade E, Johnsen SL, et al. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol. 2011; 37:116–26.
Article2. Reddy UM, Abuhamad AZ, Levine D, Saade GR. Fetal Imaging Workshop Invited Participants. Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound Fetal Imaging workshop. Obstet Gynecol. 2014; 123:1070–82.3. Soto ÁL. Genital abnormalities: contextualization of a neglected area in prenatal diagnosis. Rev Colomb Obstet Ginecol. 2020; 71:275–85.4. Achiron R, Pinhas-Hamiel O, Zalel Y, Rotstein Z, Lipitz S. Development of fetal male gender: prenatal sonographic measurement of the scrotum and evaluation of testicular descent. Ultrasound Obstet Gynecol. 1998; 11:242–5.
Article5. Birnholz JC. Determination of fetal sex. N Engl J Med. 1983; 309:942–4.
Article6. Melcer Y, Mendlovic S, Klin B, Keidar R, Lysyy O, Herman A, et al. Fetal diagnosis of testicular torsion: what shall we tell the parents? Prenat Diagn. 2015; 35:167–73.
Article7. Zampieri N, Zamboni C, Ghidini A, Borruto F, Camoglio FS. Prenatal sonographic evaluation of male genitalia development. Minerva Ginecol. 2008; 60:317–21.8. Braga LH, Lorenzo AJ, Romao RLP. Canadian Urological Association-Pediatric Urologists of Canada (CUA-PUC) guideline for the diagnosis, management, and follow-up of cryptorchidism. Can Urol Assoc J. 2017; 11:E251–60.
Article9. Ronzoni S, Melamed N, Kingdom JC, Ryan G, Jaeggi E, Windrim RC. Prenatal diagnosis of inguinoscrotal hernia associated with bowel dilatation: a pathogenetic hypothesis. Prenat Diagn. 2015; 35:1151–3.
Article10. Durmuş G, Boybeyi-Türer Ö, Gharibzadeh-Hizal M, Ekinci S, Kiper N. Meconium periorchitis: an incidentally diagnosed rare entity during inguinal herniorraphy. Turk J Pediatr. 2018; 60:612–4.
Article11. Makiyan Z. Systematization of ambiguous genitalia. Organogenesis. 2016; 12:169–82.
Article12. Marshall FF. Embryology of the lower genitourinary tract. Urol Clin North Am. 1978; 5:3–15.
Article13. Sharpe RM. Environmental/lifestyle effects on spermatogenesis. Philos Trans R Soc Lond B Biol Sci. 2010; 365:1697–712.
Article14. Sampaio FJ, Favorito LA. Analysis of testicular migration during the fetal period in humans. J Urol. 1998; 159:540–2.
Article15. Zimmermann S, Steding G, Emmen JM, Brinkmann AO, Nayernia K, Holstein AF, et al. Targeted disruption of the Insl3 gene causes bilateral cryptorchidism. Mol Endocrinol. 1999; 13:681–91.
Article16. Hutson JM, Southwell BR, Li R, Lie G, Ismail K, Harisis G, et al. The regulation of testicular descent and the effects of cryptorchidism. Endocr Rev. 2013; 34:725–52.
Article17. Fait G, Yaron Y, Shenhar D, Gull I, Har-Toov J, Jaffa AJ, et al. Sonographic detection of undescended testes in the third trimester. J Ultrasound Med. 2002; 21:15–8. quiz 20.
Article18. Delaney LR, Karmazyn B. Ultrasound of the pediatric scrotum. Semin Ultrasound CT MR. 2013; 34:248–56.
Article19. Tyloch JF, Wieczorek AP. Standards for scrotal ultrasonography. J Ultrason. 2016; 16:391–403.20. Alkhori NA, Barth RA. Pediatric scrotal ultrasound: review and update. Pediatr Radiol. 2017; 47:1125–33.
Article21. Pinette MG, Wax JR, Blackstone J, Cartin A. Normal growth and development of fetal external genitalia demonstrated by sonography. J Clin Ultrasound. 2003; 31:465–72.
Article22. Rotondi M, Valenzano F, Bilancioni E, Spanò G, Rotondi M, Giorlandino C. Prenatal measurement of testicular diameter by ultrasonography: development of fetal male gender and evaluation of testicular descent. Prenat Diagn. 2001; 21:112–5.
Article23. Baskin L, Shen J, Sinclair A, Cao M, Liu X, Liu G, et al. Development of the human penis and clitoris. Differentiation. 2018; 103:74–85.
Article24. Malas MA, Sulak O, Oztürk A. The growth of the testes during the fetal period. BJU Int. 1999; 84:689–92.
Article25. Kaplan SL, Edgar JC, Ford EG, Adgent MA, Schall JI, Kelly A, et al. Size of testes, ovaries, uterus and breast buds by ultrasound in healthy full-term neonates ages 0–3 days. Pediatr Radiol. 2016; 46:1837–47.
Article26. Kaleva M, Toppari J. Genetics and hormones in testicular descent. Hormones (Athens). 2003; 2:211–6.
Article27. Nemec SF, Nemec U, Weber M, Kasprian G, Brugger PC, Krestan CR, et al. Male sexual development in utero: testicular descent on prenatal magnetic resonance imaging. Ultrasound Obstet Gynecol. 2011; 38:688–94.
Article28. Favorito LA, Klojda CA, Sampaio FJ. Congenital absence of the testis in human fetuses and in cryptorchid patients. Int J Urol. 2004; 11:1110–3.
Article29. DeRoo SE, Lumpkins KM, El-Metwally DE. Scrotoschisis in a neonate with meconium peritonitis and periorchitis. J Neonatal Perinatal Med. 2016; 9:107–12.
Article30. Inde Y, Terada Y, Ikegami E, Sekiguchi A, Nakai A, Takeshita T. Bifid scrotum and anocutaneous fistula associated with a perineal lipomatous tumor complicated by temporary bilateral cryptorchidism in utero mimicking ambiguous genitalia: 2-D/3-D fetal ultrasonography. J Obstet Gynaecol Res. 2014; 40:843–8.
Article31. Fahmy MA, El Shennawy AA, Edress AM. Spectrum of penoscrotal positional anomalies in children. Int J Surg. 2014; 12:983–8.
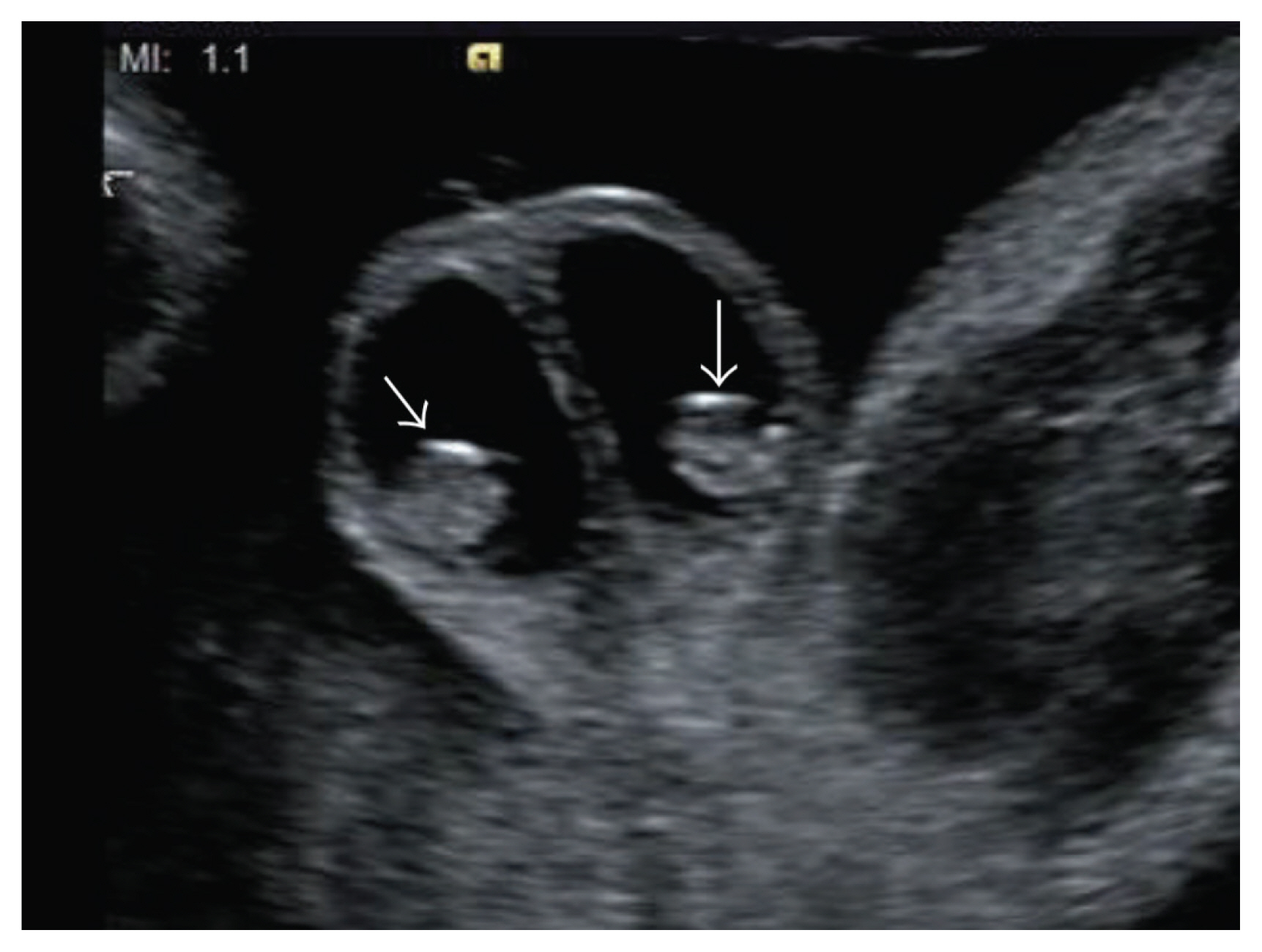
Article32. Paladini D, Palmieri S, Morelli PM, Forleo F, Morra T, Salviati M, et al. Fetal inguinoscrotal hernia: prenatal ultrasound diagnosis and pathogenetic evaluation. Ultrasound Obstet Gynecol. 1996; 7:145–6.33. Stupak A, Krzyzanowski A, Semczuk-Sikora A, Dymanowska-Dyjak I, Geca T, Kondracka A, et al. Conservative management after prenatal ultrasound diagnosis of meconium periorchitis. J Med Ultrason. 2014; 41:499–505.
Article34. Suriawinata A, Talerman A, Vapnek JM, Unger P. Hemangioma of the testis: report of unusual occurrences of cavernous hemangioma in a fetus and capillary hemangioma in an older man. Ann Diagn Pathol. 2001; 5:80–3.
Article35. Lamm DL, Kaplan GW. Accessory and ectopic scrota. Urology. 1977; 9:149–53.
Article36. Sexton P, Thomas JT, Petersen S, Brown N, Arms JE, Bryan J, et al. Complete penoscrotal transposition: case report and review of the literature. Fetal Diagn Ther. 2015; 37:70–4.
Article37. Nakamura Y, Jennings RW, Connolly S, Diamond DA. Fetal diagnosis of penoscrotal transposition associated with perineal lipoma in one twin. Fetal Diagn Ther. 2010; 27:164–7.
Article38. Murase N, Uchida H, Hiramatsu K. Accessory scrotum with perineal lipoma diagnosed prenatally: case report and review of the literature. Nagoya J Med Sci. 2015; 77:501–6.39. Ono M, Harley VR. Disorders of sex development: new genes, new concepts. Nat Rev Endocrinol. 2013; 9:79– 91.
Article40. Moorthy HK, Pillai BS, Rathore RS, Mehta N. Ectopic scrotum: a unique case report. Can Urol Assoc J. 2015; 9:E665–6.
Article41. Redman JF, Bissada NK. Complete penoscrotal transposition. Urology. 2007; 69:181–2.
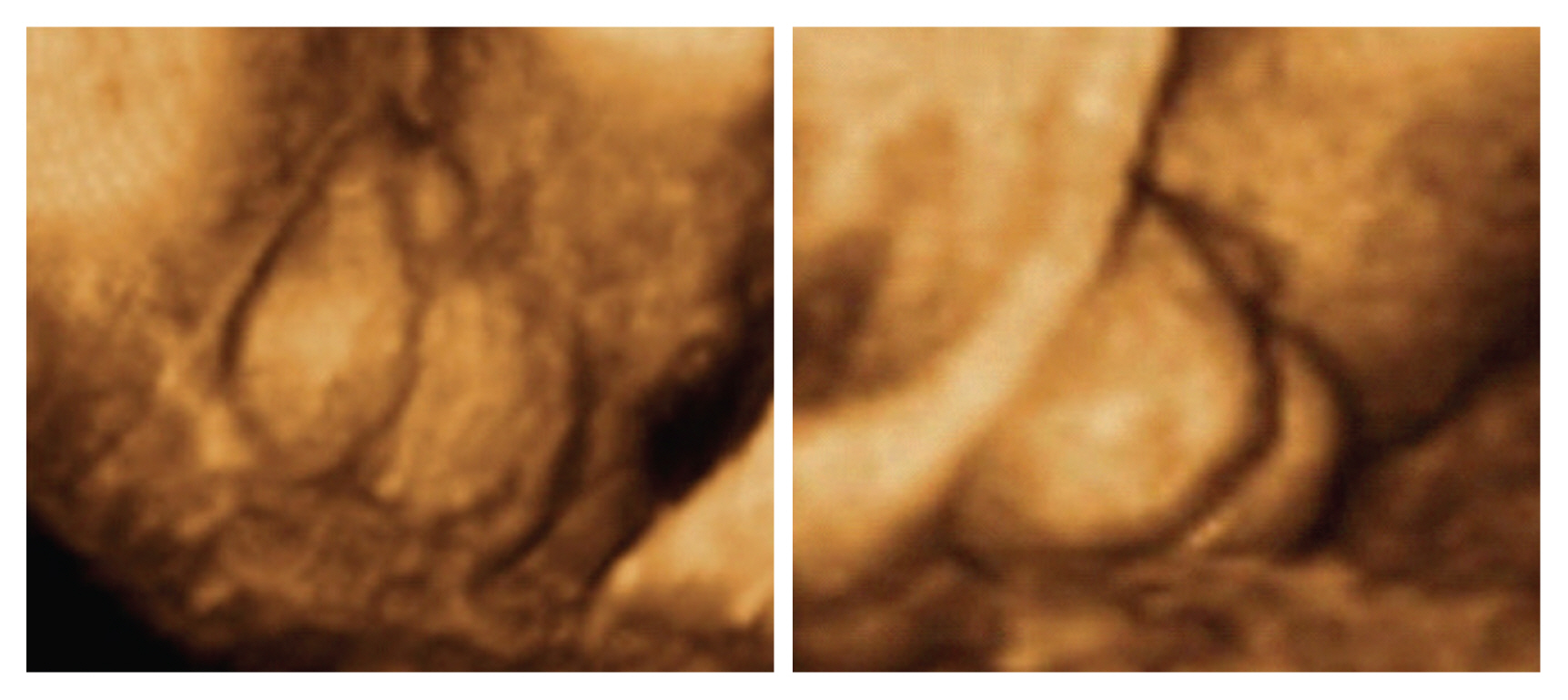
Article42. Wang Y, Cai A, Sun J, Li T, Wang B, Li J. Prenatal diagnosis of penoscrotal transposition with 2- and 3-dimensional ultrasonography. J Ultrasound Med. 2011; 30:1397–401.
Article43. Swartz JM, Ciarlo R, Denhoff E, Abrha A, Diamond DA, Hirschhorn JN, et al. Variation in the clinical and genetic evaluation of undervirilized boys with bifid scrotum and hypospadias. J Pediatr Urol. 2017; 13:293.e1–6.
Article44. Perović S, Vukadinović V. Penoscrotal transposition with hypospadias: 1-stage repair. J Urol. 1992; 148:1510–3.
Article45. Mohan PP, Woodward MN, Chandran H, Parashar K. Topical testosterone in scrotal agenesis. Pediatr Surg Int. 2006; 22:565–6.
Article46. Coplen DE, Mikkelsen D, Manley CB. Accessory scrotum located on the distal penile shaft. J Urol. 1995; 154:1908.
Article47. Nishio H, Mizuno K, Moritoki Y, Kamisawa H, Naiki T, Kurokawa S, et al. Hemiscrotal agenesis: pathogenesis and management strategies. Int J Urol. 2016; 23:523–6.
Article48. Pinke LA, Rathbun SR, Husmann DA, Kramer SA. Penoscrotal transposition: review of 53 patients. J Urol. 2001; 166:1865–8.
Article49. Karmazyn B. Scrotal ultrasound. J Clin Ultrasound. 2010; 5:61–74.
Article50. Bushby LH, Miller FN, Rosairo S, Clarke JL, Sidhu PS. Scrotal calcification: ultrasound appearances, distribution and aetiology. Br J Radiol. 2002; 75:283–8.
Article51. Calle-Toro JS, Kelly A, Ford EJ, Zemel BS, Schall JI, Adgent MA, et al. Incidental findings during ultrasound of thyroid, breast, testis, uterus and ovary in healthy term neonates. J Ultrasound. 2019; 22:395–400.
Article52. Eyssartier E, Villemagne T, Maurin L, Machet MC, Lardy H. Intrascrotal lipoblastoma: a report of two cases and a review of the literature. J Pediatr Urol. 2013; 9(6 Pt B):e151–4.53. Ito M, Hashizume K, Kanamori Y. New phenotype of accessory scrotum with perineal lipoblastoma: coexistence of midperineal and lateral accessory scrotums. Int J Urol. 2004; 11:125–7.
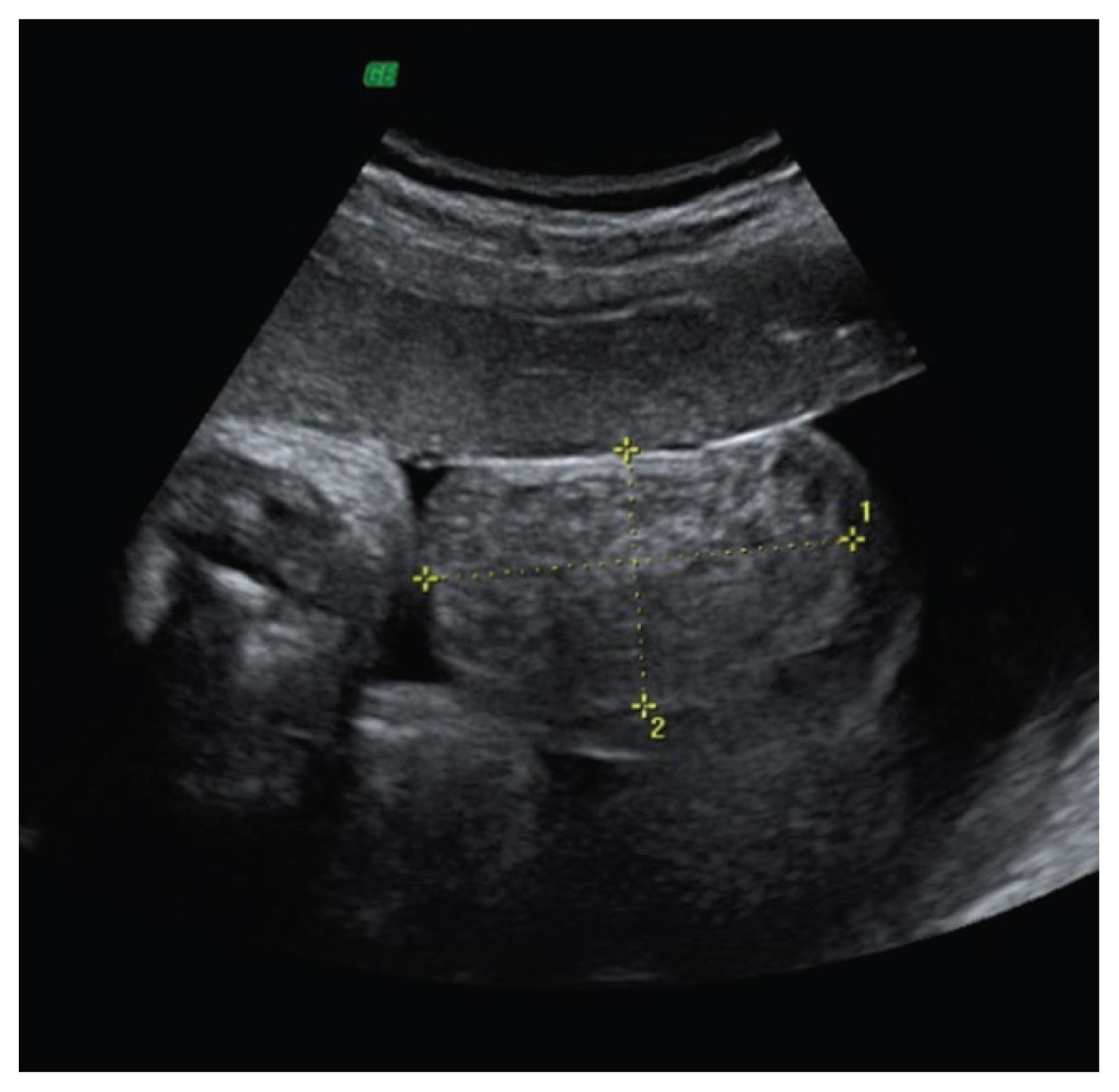
Article54. Massaro G, Sglavo G, Cavallaro A, Pastore G, Nappi C, Di Carlo C. Ultrasound prenatal diagnosis of inguinal scrotal hernia and contralateral hydrocele. Case Rep Obstet Gynecol. 2013; 2013:764579.
Article55. Pretorius DH, Halsted MJ, Abels W, Catanzarite VA, Kaplan G. Hydroceles identified prenatally: common physiologic phenomenon? J Ultrasound Med. 1998; 17:49–52.
Article56. Kim SO, Na SW, Yu HS, Kwon D. Epididymal anomalies in boys with undescended testis or hydrocele: significance of testicular location. BMC Urol. 2015; 15:108.
Article57. Berdon WE, Baker DH, Becker J, De Sanctis P. Scrotal masses in healed meconium peritonitis. N Engl J Med. 1967; 277:585–7.
Article58. Pan EY, Chen LY, Yang JZ, Lee Z, Wang ZZ. Radiographic diagnosis of meconium peritonitis. A report of 200 cases including six fetal cases. Pediatr Radiol. 1983; 13:199–205.
Article59. Rios LT, Araujo Júnior E, Nardozza LM, Caetano AC, Moron AF, Martins Mda G. Prenatal diagnosis and postnatal ultrasound findings of cloacal anomaly: a case report. Case Rep Pediatr. 2012; 2012:969860.
Article60. Wax JR, Pinette MG, Cartin A, Blackstone J. Prenatal sonographic diagnosis of meconium periorchitis. J Ultrasound Med. 2007; 26:415–7.
Article61. Ochiai D, Omori S, Ikeda T, Yakubo K, Fukuiya T. A rare case of meconium periorchitis diagnosed in utero. Case Rep Obstet Gynecol. 2015; 2015:606134.
Article62. Jeanty C, Bircher A, Turner C. Prenatal diagnosis of meconium periorchitis and review of the literature. J Ultrasound Med. 2009; 28:1729–34.
Article63. Acosta P, Gambina F, Perelli L, Díaz Pumará E, Martínez JL, Etchepareborda MN, et al. Meconium periorchitis: a case report. Arch Argent Pediatr. 2015; 113:e330–2.64. Brown-Harrison MC, Harrison AM, Reid BS, Cartwright PC. Meconium periorchitis--a cause of scrotal mass in the newborn. Clin Pediatr (Phila). 2000; 39:179–82.65. Zerhouni S, Mayer C, Skarsgard ED. Can we select fetuses with intra-abdominal calcification for delivery in neonatal surgical centres? J Pediatr Surg. 2013; 48:946–50.
Article66. Grosfeld JL. Current concepts in inguinal hernia in infants and children. World J Surg. 1989; 13:506–15.
Article67. Frati A, Ducarme G, Vuillard E, Pecastaing A, Yver C, Pejoan H, et al. Prenatal evaluation of a scrotal mass using a high-frequency probe in the diagnosis of inguinoscrotal hernia. Ultrasound Obstet Gynecol. 2008; 32:949–50.
Article68. Kesby G, Beilby R, Petroni M. Fetal inguinoscrotal hernia: sonographic diagnosis and obstetric management. Ultrasound Obstet Gynecol. 1997; 10:359–61.
Article69. Allen LM, Nosovitch JT Jr, Silverman RK, Folk JJ. Prenatal diagnosis of an inguinoscrotal hernia in a fetus with cystic fibrosis. J Ultrasound Med. 2004; 23:1391–4.
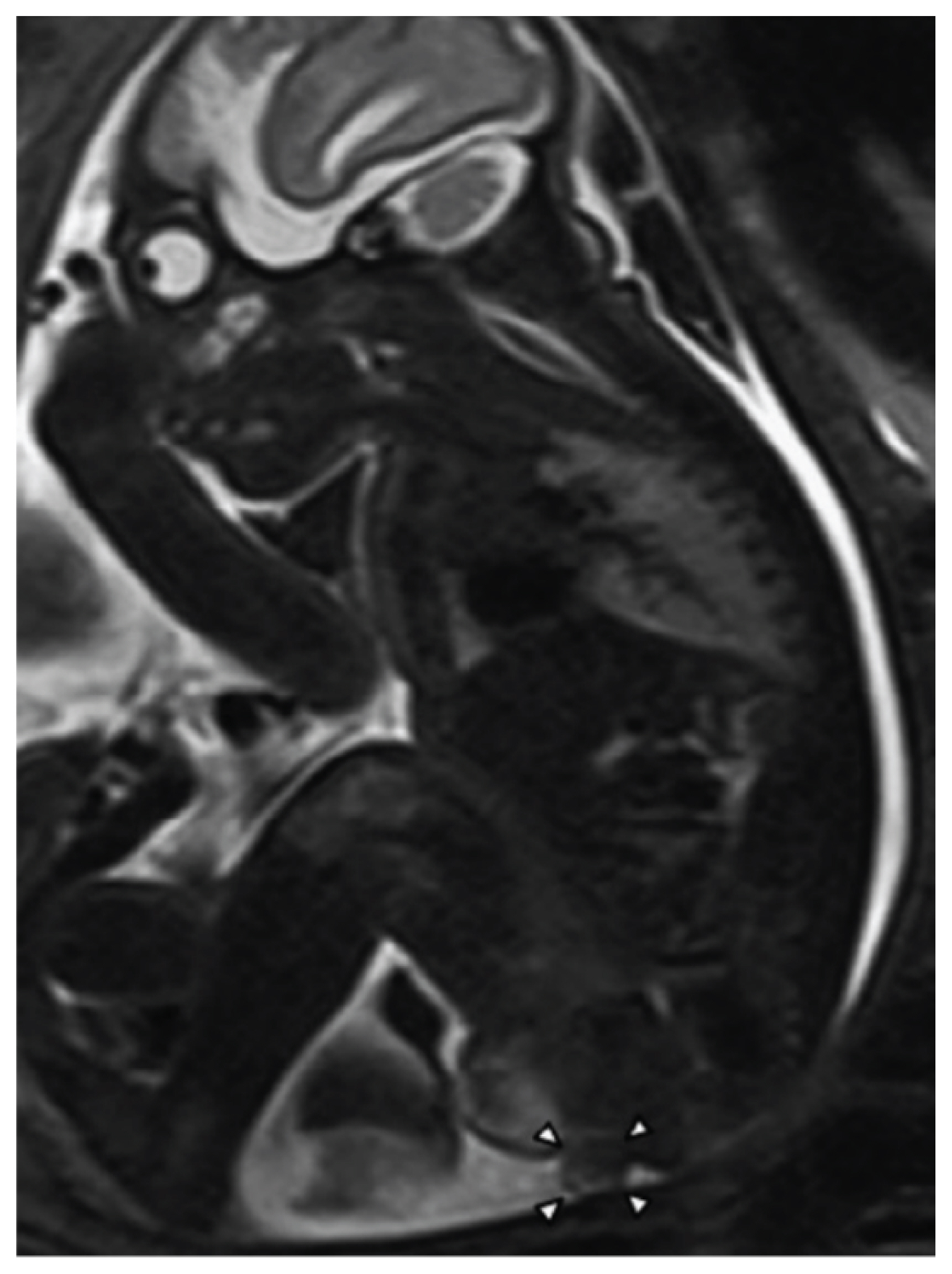
Article70. Ji EK, Yoon CS, Pretorius DH. Prenatal diagnosis of an inguinoscrotal hernia: sonographic and magnetic resonance imaging findings. J Ultrasound Med. 2005; 24:239–42.71. Khatib N, Goldstein I, Vitner D, Ganem N, Livoff A, Wiener Z. Prenatal diagnosis of scrotal-inguinal hernia: two case reports and review of the English literature. Eur J Obstet Gynecol Reprod Biol. 2013; 171:9–11.
Article72. Bhatt S, Ahmad M, Batra P, Tandon A, Roy S, Mandal S. Neonatal adrenal hemorrhage presenting as “Acute Scrotum”-looking beyond the obvious: a sonographic insight. J Ultrasound. 2017; 20:253–9.
Article73. Sountoulides P, Neri F, Bellocci R, Schips L, Cindolo L. Splenogonadal fusion mimicking a testis tumor. J Postgrad Med. 2014; 60:202–4.
Article74. Floyd MS Jr, Dowling CM, Power RE, O’Bien A, Gibney RG, Quinlan DM. Ectopic splenic tissue presenting as a scrotal mass. Ir J Med Sci. 2007; 176:141–2.
Article75. Khairat AB, Ismail AM. Splenogonadal fusion: case presentation and literature review. J Pediatr Surg. 2005; 40:1357–60.
Article76. Senescende L, Bitolog PL, Auberger E, Zarzavadjian Le Bian A, Cesaretti M. Adrenal ectopy of adult groin region: a systematic review of an unexpected anatomopathologic diagnosis. Hernia. 2016; 20:879–85.
Article77. Ji Y, Song B, Chen S, Jiang X, Yang G, Gao X, et al. Fetus in fetu in the scrotal sac: case report and literature review. Medicine (Baltimore). 2015; 94:e1322.78. Rescorla FJ. Pediatric germ cell tumors. Semin Pediatr Surg. 2012; 21:51–60.
Article79. Fumino S, Tajiri T, Usui N, Tamura M, Sago H, Ono S, et al. Japanese clinical practice guidelines for sacrococcygeal teratoma, 2017. Pediatr Int. 2019; 61:672–8.
Article80. Yu C, Wei Y, Tang X, Liu B, Shen L, Long C, et al. Maternal smoking during pregnancy and risk of cryptorchidism: a systematic review and meta-analysis. Eur J Pediatr. 2019; 178:287–97.
Article81. Boisen KA, Kaleva M, Main KM, Virtanen HE, Haavisto AM, Schmidt IM, et al. Difference in prevalence of congenital cryptorchidism in infants between two Nordic countries. Lancet. 2004; 363:1264–9.
Article82. Cendron M, Huff DS, Keating MA, Snyder HM 3rd, Duckett JW. Anatomical, morphological and volumetric analysis: a review of 759 cases of testicular maldescent. J Urol. 1993; 149:570–3.
Article83. Jensen MS, Wilcox AJ, Olsen J, Bonde JP, Thulstrup AM, Ramlau-Hansen CH, et al. Cryptorchidism and hypospadias in a cohort of 934,538 Danish boys: the role of birth weight, gestational age, body dimensions, and fetal growth. Am J Epidemiol. 2012; 175:917–25.
Article84. Juul A, Almstrup K, Andersson AM, Jensen TK, Jørgensen N, Main KM, et al. Possible fetal determinants of male infertility. Nat Rev Endocrinol. 2014; 10:553–62.
Article85. Barrett ES, Swan SH. Stress and androgen activity during fetal development. Endocrinology. 2015; 156:3435–41.
Article86. Wohlfahrt-Veje C, Boisen KA, Boas M, Damgaard IN, Kai CM, Schmidt IM, et al. Acquired cryptorchidism is frequent in infancy and childhood. Int J Androl. 2009; 32:423–8.
Article87. Tasian GE, Hittelman AB, Kim GE, DiSandro MJ, Baskin LS. Age at orchiopexy and testis palpability predict germ and Leydig cell loss: clinical predictors of adverse histological features of cryptorchidism. J Urol. 2009; 182:704–9.
Article88. Lee PA, Rogol A, Houk CP. Optimizing potential for fertility: fertility preservation considerations for the pediatric endocrinologist. Endocrinol Metab Clin North Am. 2009; 38:761–75.
Article89. Wood HM, Elder JS. Cryptorchidism and testicular cancer: separating fact from fiction. J Urol. 2009; 181:452–61.
Article90. Benacerraf BR, Bromley B. Sonographic finding of undescended testes in fetuses at 35–40 weeks: significance and outcome. J Clin Ultrasound. 1998; 26:69–71.
Article91. Kolon TF, Herndon CD, Baker LA, Baskin LS, Baxter CG, Cheng EY, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol. 2014; 192:337–45.
Article92. Rogers E, Teahan S, Gallagher H, Butler MR, Grainger R, McDermott TE, et al. The role of orchiectomy in the management of postpubertal cryptorchidism. J Urol. 1998; 159:851–4.93. Pirgon Ö, Dündar BN. Vanishing testes: a literature review. J Clin Res Pediatr Endocrinol Endocrinol. 2012; 4:116–20.
Article94. Mangaraj S, Choudhury A, Mohanty B, Baliarsinha A. Congenital anorchia: a report of two cases and a brief review of the literature. J Integr Nephrol Androl. 2017; 4:141–3.
Article95. Tosi SE, Morin LJ. The vanishing testis syndrome: indications for conservative therapy. J Urol. 1976; 115:758–9.
Article96. Turek PJ, Ewalt DH, Snyder HM 3rd, Stampfers D, Blyth B, Huff DS, et al. The absent cryptorchid testis: surgical findings and their implications for diagnosis and etiology. J Urol. 1994; 151:718–20. discussion 720–1.
Article97. Pohl HG, Shukla AR, Metcalf PD, Cilento BG, Retik AB, Bagli DJ, et al. Prepubertal testis tumors: actual prevalence rate of histological types. J Urol. 2004; 172(6 Pt 1):2370–2.
Article98. Pearl MS, Hill MC. Ultrasound of the scrotum. Semin Ultrasound CT MR. 2007; 28:225–48.
Article99. Youssef A, Salsi G, Curti A, Bellussi F, Elbarbary NA, Locatelli F, et al. Prenatal ultrasonographic features of mature cystic teratoma in undescended testicle. Ultrasound Obstet Gynecol. 2016; 47:527–9.
Article100. Peterson C, Skoog S. Prenatal diagnosis of juvenile granulosa cell tumor of the testis. J Pediatr Urol. 2008; 4:472–4.
Article101. Bulotta AL, Molinaro F, Angotti R, Ferrara F, Di Maggio G, Bindi E, et al. Juvenile granulosa cell tumor of the testis: prenatal diagnosis and prescrotal approach. Ital J Pediatr. 2012; 38:67.
Article102. Illescas T, Ibba RM, Zoppi MA, Iuculano A, Contu R, Monni G. Prenatal ultrasound diagnosis of a fetal testis granulosa cell tumour. J Obstet Gynaecol. 2014; 34:96–7.
Article103. Janda GM, Najdzionek JS, Kozielski R, Greenfield SP, Williot PE. Early prenatal detection of an intra-abdominal cryptorchid testicular teratoma. Urology. 2014; 83:214–6.
Article104. Sung EK, Setty BN, Castro-Aragon I. Sonography of the pediatric scrotum: emphasis on the Ts-torsion, trauma, and tumors. AJR Am J Roentgenol. 2012; 198:996–1003.
Article105. Herman A, Schvimer M, Tovbin J, Sandbank J, Bukovski I, Strauss S. Antenatal sonographic diagnosis of testicular torsion. Ultrasound Obstet Gynecol. 2002; 20:522–4.
Article106. Das S, Singer A. Controversies of perinatal torsion of the spermatic cord: a review, survey and recommendations. J Urol. 1990; 143:231–3.
Article107. Arena F, Nicòtina PA, Romeo C, Zimbaro G, Arena S, Zuccarello B, et al. Prenatal testicular torsion: ultrasonographic features, management and histopathological findings. Int J Urol. 2006; 13:135–41.
Article108. Al-Salem AH. Intra-uterine testicular torsion: early diagnosis and treatment. BJU Int. 1999; 83:1023–5.
Article109. van der Sluijs JW, den Hollander JC, Lequin MH, Nijman RM, Robben SG. Prenatal testicular torsion: diagnosis and natural course. An ultrasonographic study. Eur Radiol. 2004; 14:250–5.
Article110. Kaye JD, Levitt SB, Friedman SC, Franco I, Gitlin J, Palmer LS. Neonatal torsion: a 14-year experience and proposed algorithm for management. J Urol. 2008; 179:2377–83.
Article111. Olguner M, Akgür FM, Aktuğ T, Derebek E. Bilateral asynchronous perinatal testicular torsion: a case report. J Pediatr Surg. 2000; 35:1348–9.
Article112. Togami J, Radhakrishnan J. Testicular extrusion due to scrotoschisis. Urology. 2002; 60:1112.
Article113. Kella N, Asif M, Kumar M, Laghari F, Qureshi MA. Congenital extrusion of testis (scrotoschisis). J Coll Physicians Surg Pak. 2014; 24(Suppl 3):S243–4.114. Arslanoglu A, Tuncel SA, Hamarat M. Polyorchidism: color Doppler ultrasonography and magnetic resonance imaging findings. Clin Imaging. 2013; 37:189–91.
Article115. Alamsahebpour A, Hidas G, Kaplan A, McAleer IM. Bilateral polyorchidism with diffuse microlithiasis: a case report of an adolescent with 4 testes. Urology. 2013; 82:1421–3.
Article116. Trout AT, Chow J, McNamara ER, Darge K, Ramirez Grueso R, Munden M, et al. Association between testicular microlithiasis and testicular neoplasia: large multicenter study in a pediatric population. Radiology. 2017; 285:576–83.117. Posey ZQ, Ahn HJ, Junewick J, Chen JJ, Steinhardt GF. Rate and associations of epididymal cysts on pediatric scrotal ultrasound. J Urol. 2010; 184(4 Suppl):1739–42.
Article118. Favorito LA, Riberio Julio-Junior H, Sampaio FJ. Relationship between undescended testis position and prevalence of testicular appendices, epididymal anomalies, and patency of processus vaginalis. Biomed Res Int. 2017; 2017:5926370.
Article119. Pujar VC, Joshi SS, Singh DR. Scrotoschisis: a rare cause of acute scrotum in neonates. Indian J Urol. 2015; 31:262–3.
Article120. Han CH, Kang SH. Epididymal anomalies associated with patent processus vaginalis in hydrocele and cryptorchidism. J Korean Med Sci. 2002; 17:660–2.
Article121. Sahni D, Jit I, Joshi K, Sanjeev . Incidence and structure of the appendices of the testis and epididymis. J Anat. 1996; 189(Pt 2):341–8.122. Józsa T, Dienes B, Telek A, Hargitai Z, Pór A, Kiss C. Differential expression of androgen and estrogen receptor of appendix testis in patients with descended and undescended testes. Int J Urol. 2008; 15:171–4.
Article123. Lev M, Ramon J, Mor Y, Jacobson JM, Soudack M. Sonographic appearances of torsion of the appendix testis and appendix epididymis in children. J Clin Ultrasound. 2015; 43:485–9.
Article124. Manuel N, Ricardo P, Pilar GP, Miguel RM. Perspectives in pediatric pathology, Chapter 12. Congenital epididymal anomalies. Pediatr Dev Pathol. 2016; 19:12–23.
Article125. Monteilh C, Calixte R, Burjonrappa S. Controversies in the management of neonatal testicular torsion: a meta-analysis. J Pediatr Surg. 2019; 54:815–9.
Article126. Nowaczyk MJ, Irons MB. Smith-Lemli-Opitz syndrome: phenotype, natural history, and epidemiology. Am J Med Genet C Semin Med Genet. 2012; 160C(4):250–62.
Article127. Arlen AM, Nawaf C, Kirsch AJ. Prune belly syndrome: current perspectives. Pediatric Health Med Ther. 2019; 10:75–81.128. Freedman AL. Prenatal scrotal ultrasound: providing new clues in cryptorchidism. Ultrasound Obstet Gynecol. 1998; 11:240.
Article129. Bricker L, Medley N, Pratt JJ. Routine ultrasound in late pregnancy (after 24 weeks’ gestation). Cochrane Database Syst Rev. 2015; 2015:CD001451.
Article130. Henrichs J, Verfaille V, Jellema P, Viester L, Pajkrt E, Wilschut J, et al. Effectiveness of routine third trimester ultrasonography to reduce adverse perinatal outcomes in low risk pregnancy (the IRIS study): nationwide, pragmatic, multicentre, stepped wedge cluster randomised trial. BMJ. 2019; 367:I5517.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Value of Scrotal Ultrasonography in Diagnosis of Acute Scrotum
- Sonographic Features of Vasectomy-Related Changes and Abnormalities in the Scrotum
- Spontaneous Reduction of Torsion of the Appendix Epididymis Torsion During Scrotal Ultrasonography: A Case Report
- The sonographic findings of the scrotal pathology
- A Case of Leiomyosarcoma of the Scrotum