J Korean Assoc Oral Maxillofac Surg.
2021 Aug;47(4):291-314. 10.5125/jkaoms.2021.47.4.291.
A systematic review of therapeutic outcomes following treatment of squamous cell carcinoma of the retromolar trigone
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University, Cheonan, Korea
- KMID: 2519827
- DOI: http://doi.org/10.5125/jkaoms.2021.47.4.291
Abstract
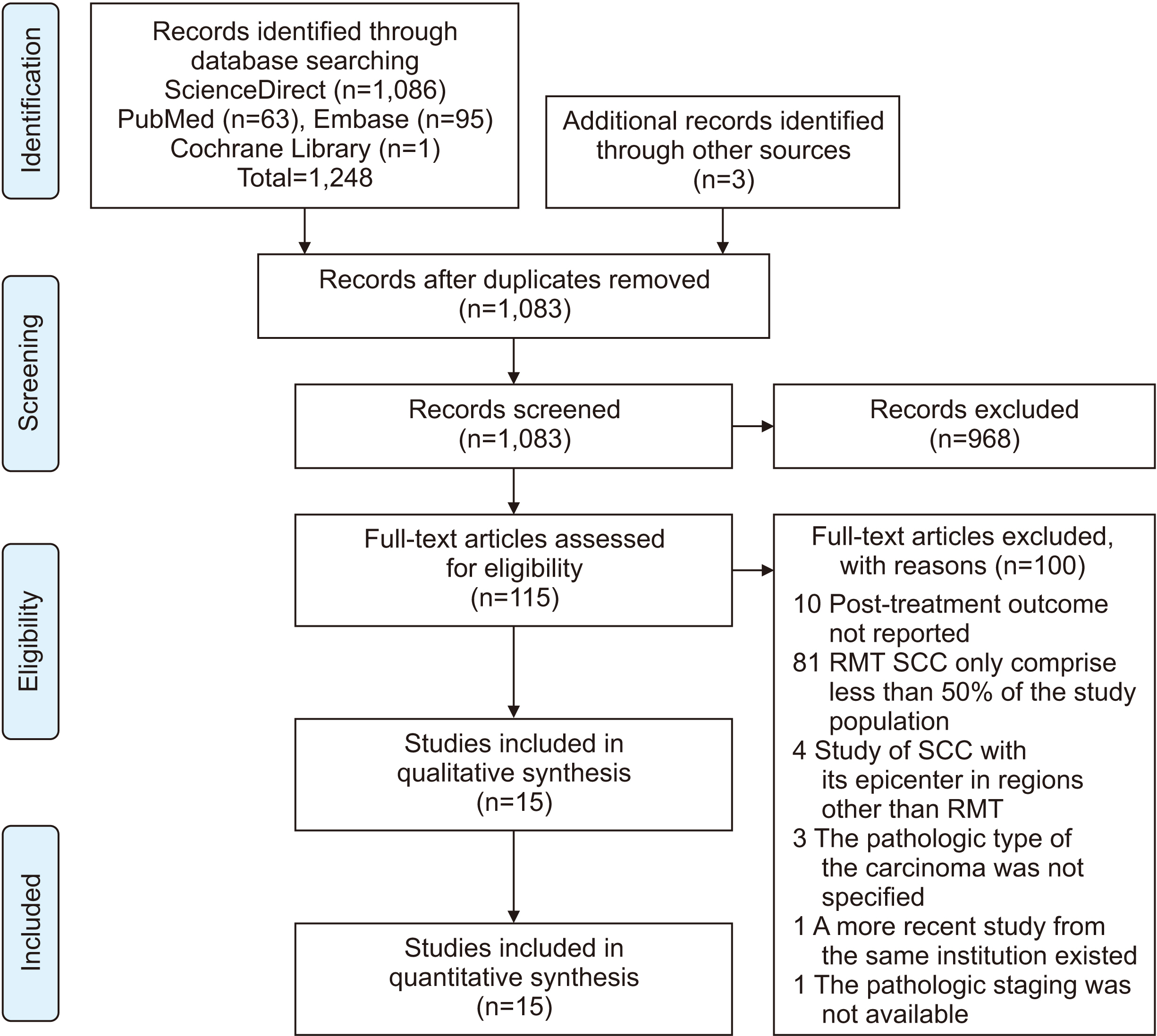
- Squamous cell carcinoma (SCC) of the retromolar trigone (RMT) is a rare but potentially fatal disease that carries a poor prognosis due to its unique anatomic position. RMT SCCs tend to spread to vital nearby structures, including the tonsillar pillar, masticatory muscles, and underlying mandibular bone, even in their early stages, and aggressive treatment is often warranted. This systematic review appraises and qualitatively analyzes all available literature regarding the survival outcomes and prognosis of RMT SCC. Four databases were searched to identify all eligible articles published since January 1980. Of the 1,248 studies, a total of 15 studies representing 4,838 cases met the inclusion criteria. The evaluated patients had a high rate of advanced tumor stage (T3 or T4: 61.4%), lymph node metastasis (38.8%), and mandibular bone invasion (24%) at the time of diagnosis. Aggressive surgical treatments such as lip-splitting (92%), segmental mandibulectomy (61.1%), radical neck dissection (44.1%), and reconstruction using free flaps (49.5%) was undertaken for 92% of the pooled patient population. The mean rates for local, regional, and systemic recurrence were 23.40%, 8.40%, and 8.50%, respectively. The mean 5-year overall survival rate was 38.90%. Osteonecrosis was noted in 11.6% of the 328 patients who received radiotherapy. In conclusion, RMT SCC is generally associated with high recurrence, low survival, and high postoperative complication rates. Early diagnosis and aggressive treatment are thus warranted. However, significant methodological problems hamper current knowledge. Future studies of this topic that use randomized or cohort designs are thus needed.
Keyword
Figure
Reference
-
References
1. Faisal M, Abbas T, Khaleeq U, Adeel M, Anwer AW, Hussain R, et al. 2017; Treatment outcomes of rare retromolar trigone squamous cell carcinoma using combined modalities. Cureus. 9:e1203. https://doi.org/10.7759/cureus.1203 . DOI: 10.7759/cureus.1203. PMID: 28580200. PMCID: PMC5451270.
Article2. Farhood Z, Simpson M, Ward GM, Walker RJ, Osazuwa-Peters N. 2019; Does anatomic subsite influence oral cavity cancer mortality? A SEER database analysis. Laryngoscope. 129:1400–6. https://doi.org/10.1002/lary.27490 . DOI: 10.1002/lary.27490. PMID: 30408182.
Article3. Luryi AL, Chen MM, Mehra S, Roman SA, Sosa JA, Judson BL. 2014; Positive surgical margins in early stage oral cavity cancer: an analysis of 20,602 cases. Otolaryngol Head Neck Surg. 151:984–90. https://doi.org/10.1177/0194599814551718 . DOI: 10.1177/0194599814551718. PMID: 25257901.
Article4. Sowder JC, Cannon RB, Buchmann LO, Hunt JP, Hitchcock Y, Lloyd S, et al. 2017; Treatment-related determinants of survival in early-stage (T1-2N0M0) oral cavity cancer: a population-based study. Head Neck. 39:876–80. https://doi.org/10.1002/hed.24679 . DOI: 10.1002/hed.24679. PMID: 28236368.
Article5. Mukherji SK, Pillsbury HR, Castillo M. 1997; Imaging squamous cell carcinomas of the upper aerodigestive tract: what clinicians need to know. Radiology. 205:629–46. https://doi.org/10.1148/radiology.205.3.9393513 . DOI: 10.1148/radiology.205.3.9393513. PMID: 9393513.
Article6. Richardson WS, Wilson MC, Nishikawa J, Hayward RS. 1995; The well-built clinical question: a key to evidence-based decisions. ACP J Club. 123:A12–3. PMID: 7582737.7. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. 2009; The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 62:e1–34. https://doi.org/10.1016/j.jclinepi.2009.06.006 . DOI: 10.1016/j.jclinepi.2009.06.006. PMID: 19631507.
Article8. Saltaji H, Major MP, Altalibi M, Youssef M, Flores-Mir C. 2012; Long-term skeletal stability after maxillary advancement with distraction osteogenesis in cleft lip and palate patients. Angle Orthod. 82:1115–22. https://doi.org/10.2319/011212-27.1 . DOI: 10.2319/011212-27.1. PMID: 22506512.
Article9. Deo SV, Shukla NK, Kallianpur AA, Mohanti BK, Thulkar SP. 2013; Aggressive multimodality management of locally advanced retromolar trigone tumors. Head Neck. 35:1269–73. https://doi.org/10.1002/hed.23113 . DOI: 10.1002/hed.23113. PMID: 22907659.
Article10. Huang CJ, Chao KS, Tsai J, Simpson JR, Haughey B, Spector GJ, et al. 2001; Cancer of retromolar trigone: long-term radiation therapy outcome. Head Neck. 23:758–63. https://doi.org/10.1002/hed.1108 . DOI: 10.1002/hed.1108. PMID: 11505486.
Article11. Kowalski LP, Hashimoto I, Magrin J. 1993; End results of 114 extended "commando" operations for retromolar trigone carcinoma. Am J Surg. 166:374–9. https://doi.org/10.1016/s0002-9610(05)80336-8 .
Article12. Binahmed A, Nason RW, Abdoh AA, Sándor GK. 2007; Population-based study of treatment outcomes in squamous cell carcinoma of the retromolar trigone. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 104:662–5. https://doi.org/10.1016/j.tripleo.2007.04.004 . DOI: 10.1016/j.tripleo.2007.04.004. PMID: 17764982.
Article13. Petruzzelli GJ, Knight FK, Vandevender D, Clark JI, Emami B. 2003; Posterior marginal mandibulectomy in the management of cancer of the oral cavity and oropharynx. Otolaryngol Head Neck Surg. 129:713–9. https://doi.org/10.1016/s0194-5998(03)01387-1 . DOI: 10.1016/s0194-5998(03)01387-1. PMID: 14663440.
Article14. Bayman NA, Sykes AJ, Bonington S, Blackburn T, Patel M, Swindell R, et al. 2010; Primary radiotherapy for carcinoma of the retromolar trigone: a useful alternative to surgery. Clin Oncol (R Coll Radiol). 22:119–24. https://doi.org/10.1016/j.clon.2009.10.017 . DOI: 10.1016/j.clon.2009.10.017. PMID: 19962868.
Article15. Factor O, Su W, Lazarev S, Miles B, Genden E, Sharma S, et al. 2020; Rapid in-field failures following adjuvant radiation for buccal squamous cell carcinoma. Laryngoscope. 130:413–7. https://doi.org/10.1002/lary.27996 . DOI: 10.1002/lary.27996. PMID: 31021426.
Article16. Ayad T, Gélinas M, Guertin L, Larochelle D, Del Vecchio P, Tabet JC, et al. 2005; Retromolar trigone carcinoma treated by primary radiation therapy: an alternative to the primary surgical approach. Arch Otolaryngol Head Neck Surg. 131:576–82. https://doi.org/10.1001/archotol.131.7.576 . DOI: 10.1001/archotol.131.7.576. PMID: 16027279.
Article17. Hitchcock KE, Amdur RJ, Morris CG, Werning JW, Dziegielewski PT, Mendenhall WM. 2015; Retromolar trigone squamous cell carcinoma treated with radiotherapy alone or combined with surgery: a 10-year update. Am J Otolaryngol. 36:140–5. https://doi.org/10.1016/j.amjoto.2014.10.005 . DOI: 10.1016/j.amjoto.2014.10.005. PMID: 25456514.
Article18. Nishi H, Shinozaki T, Tomioka T, Maruo T, Hayashi R. 2018; Squamous cell carcinoma of the retromolar trigone: treatment outcomes. Auris Nasus Larynx. 45:337–42. https://doi.org/10.1016/j.anl.2017.05.011 . DOI: 10.1016/j.anl.2017.05.011. PMID: 28624429.
Article19. Byers RM, Anderson B, Schwarz EA, Fields RS, Meoz R. 1984; Treatment of squamous carcinoma of the retromolar trigone. Am J Clin Oncol. 7:647–52. https://doi.org/10.1097/00000421-198412000-00011 . DOI: 10.1097/00000421-198412000-00011. PMID: 6442099.
Article20. Hao SP, Tsang NM, Chang KP, Chen CK, Huang SS. 2006; Treatment of squamous cell carcinoma of the retromolar trigone. Laryngoscope. 116:916–20. https://doi.org/10.1097/01.mlg.0000214900.07495.39 . DOI: 10.1097/01.mlg.0000214900.07495.39. PMID: 16735888.
Article21. Demir UL, Öztürk Yanaşma H. 2020; Treatment outcomes for primary retromolar trigone carcinoma: a single institution experience. Turk Arch Otorhinolaryngol. 58:87–92. https://doi.org/10.5152/tao.2020.5153 . DOI: 10.5152/tao.2020.5153. PMID: 32783034. PMCID: PMC7397542.
Article22. Rizvi ZH, Alonso JE, Kuan EC, St John MA. 2018; Treatment outcomes of patients with primary squamous cell carcinoma of the retromolar trigone. Laryngoscope. 128:2740–4. https://doi.org/10.1002/lary.27234 . DOI: 10.1002/lary.27234. PMID: 29756295.
Article23. Mazziotti S, Pandolfo I, D'Angelo T, Mileto A, Visalli C, Racchiusa S, et al. 2014; Diagnostic approach to retromolar trigone cancer by multiplanar computed tomography reconstructions. Can Assoc Radiol J. 65:335–44. https://doi.org/10.1016/j.carj.2014.04.001 . DOI: 10.1016/j.carj.2014.04.001. PMID: 25267376.
Article24. Zygogianni AG, Kyrgias G, Karakitsos P, Psyrri A, Kouvaris J, Kelekis N, et al. 2011; Oral squamous cell cancer: early detection and the role of alcohol and smoking. Head Neck Oncol. 3:2. https://doi.org/10.1186/1758-3284-3-2 . DOI: 10.1186/1758-3284-3-2. PMID: 21211041. PMCID: PMC3022893.
Article25. Llewelyn J, Mitchell R. 1994; Smoking, alcohol and oral cancer in South East Scotland: a 10-year experience. Br J Oral Maxillofac Surg. 32:146–52. https://doi.org/10.1016/0266-4356(94)90098-1 . DOI: 10.1016/0266-4356(94)90098-1. PMID: 8068584.
Article26. Schmidt BL, Dierks EJ, Homer L, Potter B. 2004; Tobacco smoking history and presentation of oral squamous cell carcinoma. J Oral Maxillofac Surg. 62:1055–8. https://doi.org/10.1016/j.joms.2004.03.010 . DOI: 10.1016/j.joms.2004.03.010. PMID: 15346353.
Article27. Morelatto RA, Herrera MC, Fernández EN, Corball AG, López de Blanc SA. 2007; Diagnostic delay of oral squamous cell carcinoma in two diagnosis centers in Córdoba Argentina. J Oral Pathol Med. 36:405–8. https://doi.org/10.1111/j.1600-0714.2007.00547.x . DOI: 10.1111/j.1600-0714.2007.00547.x. PMID: 17617833.
Article28. Seoane-Romero JM, Vázquez-Mahía I, Seoane J, Varela-Centelles P, Tomás I, López-Cedrún JL. 2012; Factors related to late stage diagnosis of oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal. 17:e35–40. https://doi.org/10.4317/medoral.17399 . DOI: 10.4317/medoral.17399. PMID: 21743390. PMCID: PMC3448190.
Article29. Burusapat C, Jarungroongruangchai W, Charoenpitakchai M. 2015; Prognostic factors of cervical node status in head and neck squamous cell carcinoma. World J Surg Oncol. 13:51. https://doi.org/10.1186/s12957-015-0460-6 . DOI: 10.1186/s12957-015-0460-6. PMID: 25889704. PMCID: PMC4336753.
Article30. Lane AP, Buckmire RA, Mukherji SK, Pillsbury HC 3rd, Meredith SD. 2000; Use of computed tomography in the assessment of mandibular invasion in carcinoma of the retromolar trigone. Otolaryngol Head Neck Surg. 122:673–7. https://doi.org/10.1067/mhn.2000.104806 . DOI: 10.1016/S0194-5998(00)70194-X. PMID: 10793344.
Article31. Cheng A, Cox D, Schmidt BL. 2008; Oral squamous cell carcinoma margin discrepancy after resection and pathologic processing. J Oral Maxillofac Surg. 66:523–9. https://doi.org/10.1016/j.joms.2007.08.040 . DOI: 10.1016/j.joms.2007.08.040. PMID: 18280387.
Article32. Ellis OG, David MC, Park DJ, Batstone MD. 2016; High-volume surgeons deliver larger surgical margins in oral cavity cancer. J Oral Maxillofac Surg. 74:1466–72. https://doi.org/10.1016/j.joms.2016.01.026 . DOI: 10.1016/j.joms.2016.01.026. PMID: 26896758.
Article33. Brinkman D, Callanan D, O'Shea R, Jawad H, Feeley L, Sheahan P. 2020; Impact of 3 mm margin on risk of recurrence and survival in oral cancer. Oral Oncol. 110:104883. https://doi.org/10.1016/j.oraloncology.2020.104883 . DOI: 10.1016/j.oraloncology.2020.104883. PMID: 32659737.
Article34. Chen TC, Wang CP, Ko JY, Yang TL, Lou PJ. 2012; The impact of pathologic close margin on the survival of patients with early stage oral squamous cell carcinoma. Oral Oncol. 48:623–8. https://doi.org/10.1016/j.oraloncology.2012.01.015 . DOI: 10.1016/j.oraloncology.2012.01.015. PMID: 22349276.
Article35. Sutton DN, Brown JS, Rogers SN, Vaughan ED, Woolgar JA. 2003; The prognostic implications of the surgical margin in oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 32:30–4. https://doi.org/10.1054/ijom.2002.0313 . DOI: 10.1054/ijom.2002.0313. PMID: 12653229.
Article36. Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, et al. SEER Cancer Statistics Review, 1975-2008 [Internet]. National Cancer Institute;Bethesda (MD): Available from: https://seer.cancer.gov/csr/1975_2008/ . cited 2020 Sep 9.37. Dieleman FJ, Phan TTT, van den Hoogen FJA, Kaanders JHAM, Merkx MAW. 2017; The efficacy of hyperbaric oxygen therapy related to the clinical stage of osteoradionecrosis of the mandible. Int J Oral Maxillofac Surg. 46:428–33. https://doi.org/10.1016/j.ijom.2016.12.004 . DOI: 10.1016/j.ijom.2016.12.004. PMID: 28043745.
Article38. Curi MM, Dib LL. 1997; Osteoradionecrosis of the jaws: a retrospective study of the background factors and treatment in 104 cases. J Oral Maxillofac Surg. 55:540–4. discussion 545–6. https://doi.org/10.1016/s0278-2391(97)90478-x . DOI: 10.1016/s0278-2391(97)90478-x. PMID: 9191633.
Article39. Nabil S, Samman N. 2012; Risk factors for osteoradionecrosis after head and neck radiation: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 113:54–69. https://doi.org/10.1016/j.tripleo.2011.07.042 . DOI: 10.1016/j.tripleo.2011.07.042. PMID: 22669065.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tumor resection from retromolar trigone, posterolateral maxilla, and anterior mandibular ramus using lower cheek flap approach: a case report and review of literature
- Elective Neck Dissection in Oral Squamous Cell Carcinoma
- Overall Five-Year Survival Rate in Squamous Cell Carcinoma of Oral Cavity
- Pseudoangiosarcomatous Squamous Cell Carcinoma of the Face
- A Case of Squamous Cell Carcinoma in Situ in Renal Transplant Patient Treated with 5% Imiquimod