Endocrinol Metab.
2021 Aug;36(4):778-789. 10.3803/EnM.2021.1101.
The Positive Association between Subclinical Hypothyroidism and Newly-Diagnosed Hypertension Is More Explicit in Female Individuals Younger than 65
- Affiliations
-
- 1Department of Endocrinology and Metabolism and the Institute of Endocrinology, The NHC Key Laboratory of Diagnosis and Treatment of Thyroid Diseases, The First Hospital of China Medical University, Shenyang, China
- 2Department of Endocrinology and Metabolism, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
- 3Department of Endocrinology and Metabolism, People’s Hospital of the Tibet Autonomous Region, Lhasa, Tibet, China
- 4Department of Endocrinology, The First People’s Hospital of Yunnan Province, Kunming, China
- 5Department of Endocrinology, The First Hospital of Shanxi Medical University, Taiyuan, China
- 6Department of Endocrinology, Qinghai Provincial People’s Hospital, Xining, China
- 7Department of Endocrinology, The First Hospital of Lanzhou University, Lanzhou, China
- 8Department of Endocrinology and Metabolism, State Key Laboratory of Biotherapy, West China Hospital, Sichuan University, Chengdu, China
- 9Department of Endocrinology and Metabolism, The First Hospital of Jilin University, Changchun, China
- 10Department of Endocrinology, Health Science Affiliated Zhoupu Hosipital, Shanghai University of Medicine, Shanghai, China
- 11Department of Endocrinology, The First Hospital of An Hui Medical University, Hefei, China
- 12Department of Endocrinology, Chinese PLA General Hospital, Beijing, China
- 13Department of Endocrinology, Southwest Hospital, Third Military Medical University, Chongqing, China
- 14Department of Endocrinology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
- 15Department of Endocrinology, Cardiovascular and Cerebrovascular Disease Hospital of Ningxia Medical University, Yinchuan, China
- 16Department of Endocrinology and Metabolism, The Second Affiliated Hospital of Nanchang University, Nanchang, China
- 17Department of Endocrinology, The First Affiliated Hospital of Harbin Medical University, Harbin, China
- 18Department of Endocrinology, The Affiliated Hospital of Inner Mongolia Medical University. Hohhot, China
- 19Department of Endocrinology and Metabolism, The Second Xiangya Hospital, Central South University, Changsha, China
- 20Research Center of Endocrine and Metabolic Diseases, Affiliated Hospital of Integrated Traditional Chinese and Western Medicine, Nanjing University of Chinese Medicine, Nanjing, China
- 21Department of Endocrinology and Metabolism, Fujian Institute of Endocrinology, Fujian Medical University Union Hospital, Fuzhou, China
- 22Division of Endocrinology, Department of Internal Medicine, The First Affiliated Hospital, Zhengzhou University, Zhengzhou, China
- 23Department of Endocrine, First Affiliated Hospital of Guangxi Medical University, Nanning, China
- 24Department of Endocrinology, Hainan General Hospital, Haikou, China
- 25Department of Endocrinology, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
- 26Department of Endocrinology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 27Zhejiang Provincial Center for Disease Control and Prevention, Hangzhou, China
- 28Department of Endocrinology and Metabolism, Affiliated Hospital of Guiyang Medical University, Guiyang, China
- 29Department of Endocrinology, Second Hospital of Hebei Medical University, Shijiazhuang, China
- 30Department of Endocrinology, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
- 31Department of Endocrinology and Metabolism, Tianjin Medical University General Hospital, Tianjin, China
- KMID: 2519666
- DOI: http://doi.org/10.3803/EnM.2021.1101
Abstract
- Background
Subclinical hypothyroidism (SCH) is the most common thyroid dysfunction, and its relationship with blood pressure (BP) has been controversial. The aim of the study was to analyze the association between SCH and newly-diagnosed hypertension.
Methods
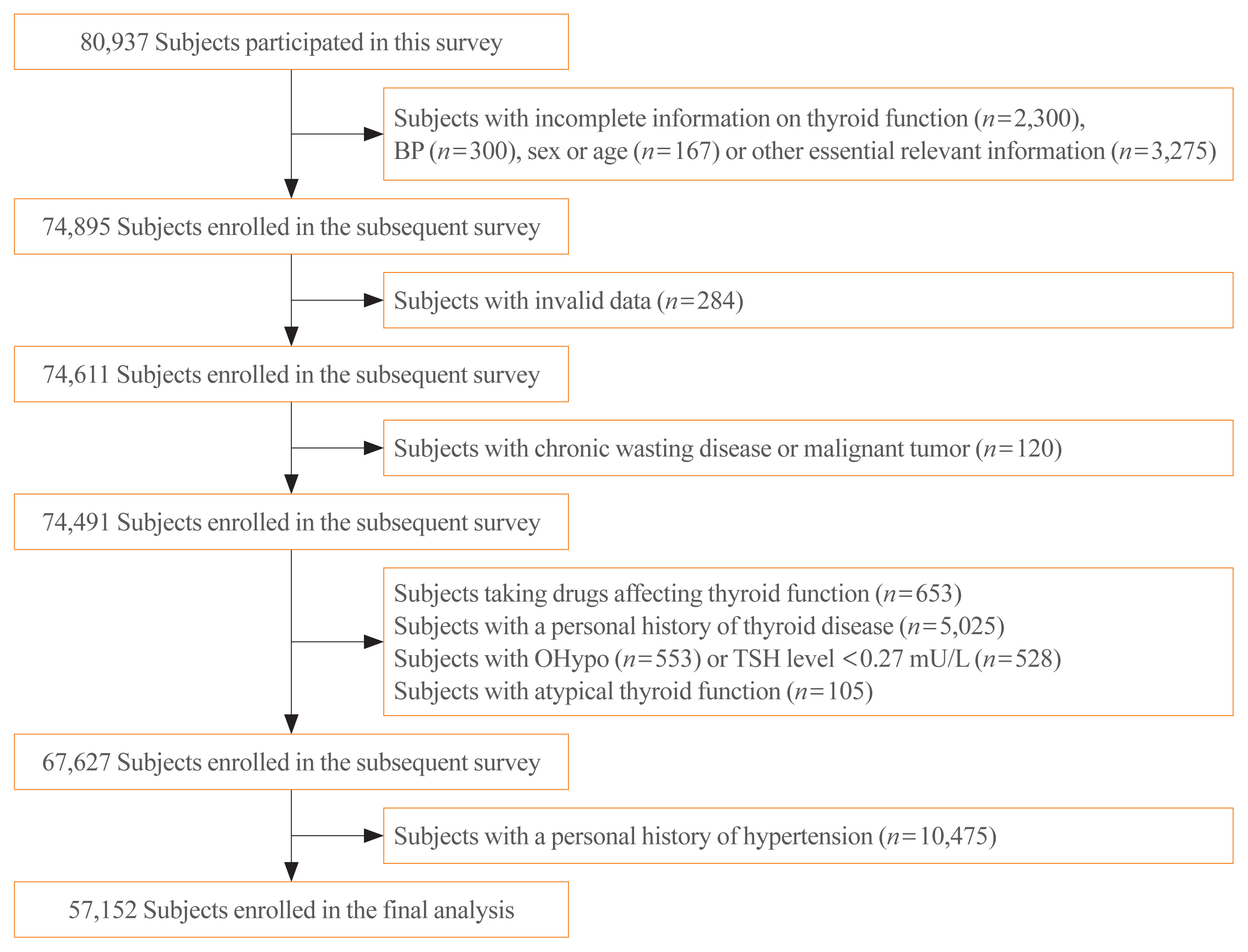
Based on data from the Thyroid disease, Iodine nutrition and Diabetes Epidemiology (TIDE) study, 49,433 euthyroid individuals and 7,719 SCH patients aged ≥18 years were enrolled. Patients with a history of hypertension or thyroid disease were excluded. SCH was determined by manufacturer reference range. Overall hypertension and stage 1 and 2 hypertension were diagnosed according to the guidelines issued by the American College of Cardiology/American Heart Association in 2017.
Results
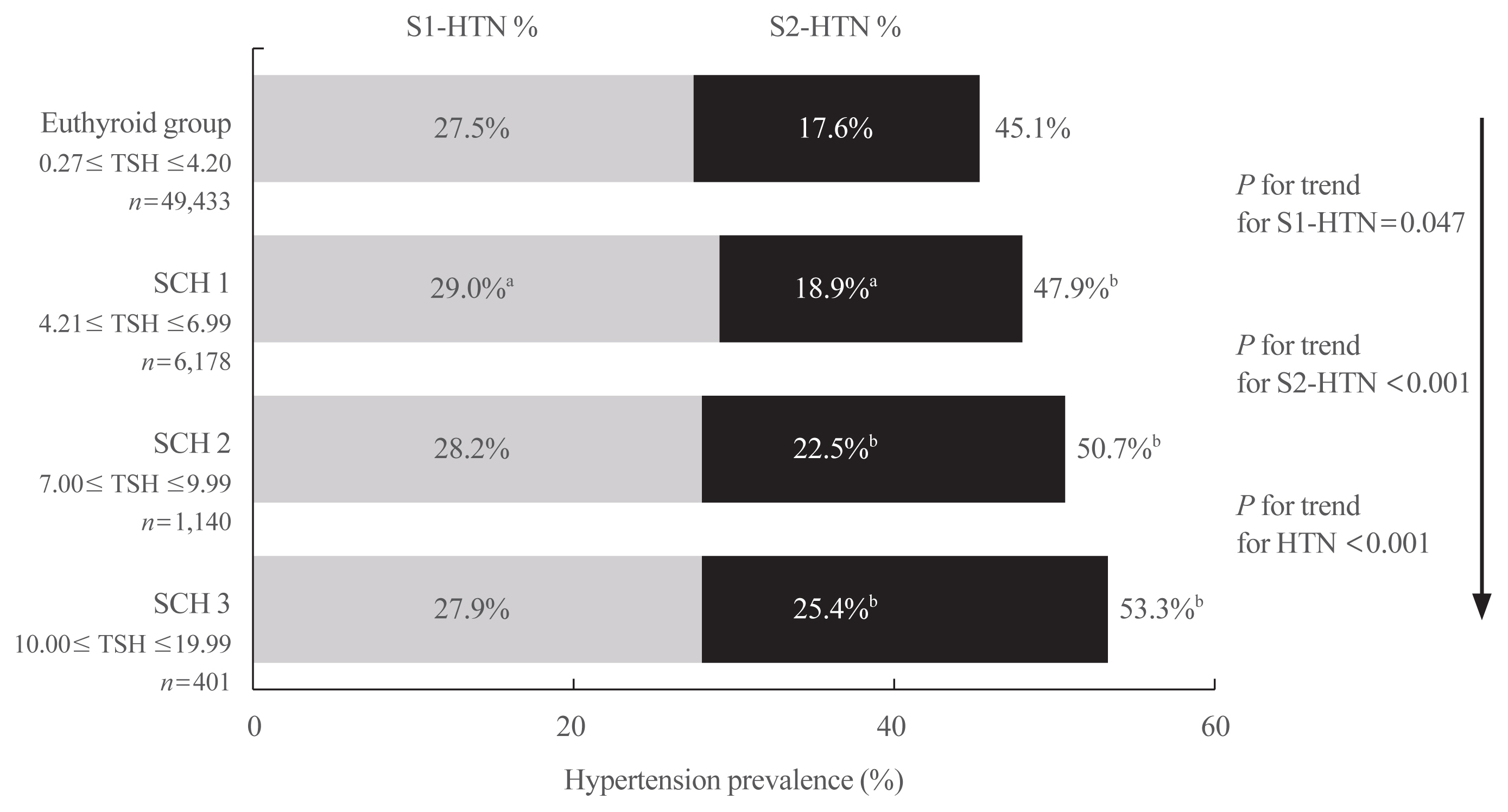
The prevalence of overall hypertension (48.7%), including stage 1 (28.9%) and 2 (19.8%) hypertension, increased significantly in SCH patients compared with euthyroid subjects. With elevated serum thyroid stimulating hormone (TSH) level, the hypertension prevalence also increased significantly from the euthyroid to different SCH subgroups, which was more profound in females or subjects aged <65 years. The age- and sex-specific regression analysis further demonstrated the same trends in the general population and in the 1:1 propensity matched population. Similarly, several BP components (i.e., systolic, diastolic, and mean arterial BP) were positively associated with TSH elevation, and regression analysis also confirmed that all BP components were closely related with SCH in female subjects aged <65 years.
Conclusion
The prevalence of hypertension increases for patients with SCH. SCH tends to be associated with hypertension and BP components in females younger than 65 years.
Keyword
Figure
Reference
-
1. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press. 2018; 27:314–40.
Article2. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; 390:1151–210.3. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015; 385:117–71.4. Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M, de la Cruz JJ, et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018; 378:1509–20.
Article5. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018; 137:2344–56.6. Jabbar A, Pingitore A, Pearce SH, Zaman A, Iervasi G, Razvi S. Thyroid hormones and cardiovascular disease. Nat Rev Cardiol. 2017; 14:39–55.
Article7. Hennessey JV, Espaillat R. Subclinical hypothyroidism: a historical view and shifting prevalence. Int J Clin Pract. 2015; 69:771–82.
Article8. Li Y, Teng D, Ba J, Chen B, Du J, He L, et al. Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 provinces of mainland China. Thyroid. 2020; 30:568–79.
Article9. Chen H, Xi Q, Zhang H, Song B, Liu X, Mao X, et al. Investigation of thyroid function and blood pressure in school-aged subjects without overt thyroid disease. Endocrine. 2012; 41:122–9.
Article10. Liu D, Jiang F, Shan Z, Wang B, Wang J, Lai Y, et al. A cross-sectional survey of relationship between serum TSH level and blood pressure. J Hum Hypertens. 2010; 24:134–8.
Article11. Walsh JP, Bremner AP, Bulsara MK, O’Leary P, Leedman PJ, Feddema P, et al. Subclinical thyroid dysfunction and blood pressure: a community-based study. Clin Endocrinol (Oxf). 2006; 65:486–91.
Article12. Luboshitzky R, Aviv A, Herer P, Lavie L. Risk factors for cardiovascular disease in women with subclinical hypothyroidism. Thyroid. 2002; 12:421–5.
Article13. Takashima N, Niwa Y, Mannami T, Tomoike H, Iwai N. Characterization of subclinical thyroid dysfunction from cardiovascular and metabolic viewpoints: the Suita study. Circ J. 2007; 71:191–5.
Article14. Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020; 369:m997.
Article15. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018; 71:e127–248.16. Biondi B, Cappola AR, Cooper DS. Subclinical hypothyroidism: a review. JAMA. 2019; 322:153–60.17. Chaker L, Baumgartner C, den Elzen WP, Ikram MA, Blum MR, Collet TH, et al. Subclinical hypothyroidism and the risk of stroke events and fatal stroke: an individual participant data analysis. J Clin Endocrinol Metab. 2015; 100:2181–91.
Article18. Gencer B, Collet TH, Virgini V, Bauer DC, Gussekloo J, Cappola AR, et al. Subclinical thyroid dysfunction and the risk of heart failure events: an individual participant data analysis from 6 prospective cohorts. Circulation. 2012; 126:1040–9.
Article19. Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010; 304:1365–74.
Article20. Floriani C, Gencer B, Collet TH, Rodondi N. Subclinical thyroid dysfunction and cardiovascular diseases: 2016 update. Eur Heart J. 2018; 39:503–7.
Article21. Pearce SH, Brabant G, Duntas LH, Monzani F, Peeters RP, Razvi S, et al. 2013 ETA guideline: management of subclinical hypothyroidism. Eur Thyroid J. 2013; 2:215–28.
Article22. Moon S, Kim MJ, Yu JM, Yoo HJ, Park YJ. Subclinical hypothyroidism and the risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Thyroid. 2018; 28:1101–10.
Article23. Garin MC, Arnold AM, Lee JS, Tracy RP, Cappola AR. Subclinical hypothyroidism, weight change, and body composition in the elderly: the Cardiovascular Health Study. J Clin Endocrinol Metab. 2014; 99:1220–6.
Article24. Cappola AR, Fried LP, Arnold AM, Danese MD, Kuller LH, Burke GL, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006; 295:1033–41.
Article25. Stott DJ, Rodondi N, Kearney PM, Ford I, Westendorp RG, Mooijaart SP, et al. Thyroid hormone therapy for older adults with subclinical hypothyroidism. N Engl J Med. 2017; 376:2534–44.26. Cai P, Peng Y, Chen Y, Li L, Chu W, Wang Y, et al. Association of thyroid function with white coat hypertension and sustained hypertension. J Clin Hypertens (Greenwich). 2019; 21:674–83.
Article27. Talwalkar P, Deshmukh V, Bhole M. Prevalence of hypothyroidism in patients with type 2 diabetes mellitus and hypertension in India: a cross-sectional observational study. Diabetes Metab Syndr Obes. 2019; 12:369–76.28. Lee MK, Kim YM, Sohn SY, Lee JH, Won YJ, Kim SH. Evaluation of the relationship of subclinical hypothyroidism with metabolic syndrome and its components in adolescents: a population-based study. Endocrine. 2019; 65:608–15.
Article29. Tseng FY, Lin WY, Lin CC, Lee LT, Li TC, Sung PK, et al. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults. J Am Coll Cardiol. 2012; 60:730–7.
Article30. Gonzalez Gil L, de la Sierra A. Prevalence of hypertension and other cardiovascular risk factors in subjects with subclinical hypothyroidism. Med Clin (Barc). 2017; 148:351–3.
Article31. Liu C, Scherbaum WA, Schott M, Schinner S. Subclinical hypothyroidism and the prevalence of the metabolic syndrome. Horm Metab Res. 2011; 43:417–21.
Article32. Asvold BO, Bjoro T, Nilsen TI, Vatten LJ. Association between blood pressure and serum thyroid-stimulating hormone concentration within the reference range: a population-based study. J Clin Endocrinol Metab. 2007; 92:841–5.
Article33. Zhang J, Huang C, Meng Z, Fan Y, Yang Q, Zhang W, et al. Gender-specific differences on the association of hypertension with subclinical thyroid dysfunction. Int J Endocrinol. 2019; 2019:6053068.
Article34. Mehran L, Amouzegar A, Rahimabad PK, Tohidi M, Tahmasebinejad Z, Azizi F. Thyroid function and metabolic syndrome: a population-based thyroid study. Horm Metab Res. 2017; 49:192–200.
Article35. Wu J, Li T, Song X, Sun W, Zhang Y, Liu Y, et al. Prevalence and distribution of hypertension and related risk factors in Jilin Province, China 2015: a cross-sectional study. BMJ Open. 2018; 8:e020126.
Article36. Zhao L, Teng D, Shi X, Li Y, Ba J, Chen B, et al. The effect of increased iodine intake on serum thyrotropin: a cross-sectional, Chinese nationwide study. Thyroid. 2020; 30:1810–9.
Article37. Cai Y, Ren Y, Shi J. Blood pressure levels in patients with subclinical thyroid dysfunction: a meta-analysis of cross-sectional data. Hypertens Res. 2011; 34:1098–105.
Article38. Gong N, Gao C, Chen X, Fang Y, Tian L. Endothelial function in patients with subclinical hypothyroidism: a meta-analysis. Horm Metab Res. 2019; 51:691–702.
Article39. Ye Y, Xie H, Zeng Y, Zhao X, Tian Z, Zhang S. Association between subclinical hypothyroidism and blood pressure: a meta-analysis of observational studies. Endocr Pract. 2014; 20:150–8.40. Ittermann T, Tiller D, Meisinger C, Agger C, Nauck M, Rettig R, et al. High serum thyrotropin levels are associated with current but not with incident hypertension. Thyroid. 2013; 23:955–63.
Article41. Wolffenbuttel BH, Wouters HJ, Slagter SN, van Waateringe RP, Muller Kobold AC, van Vliet-Ostaptchouk JV, et al. Thyroid function and metabolic syndrome in the population-based LifeLines cohort study. BMC Endocr Disord. 2017; 17:65.
Article42. Kus A, Marouli E, Del Greco MF, Chaker L, Bednarczuk T, Peeters RP, et al. Variation in normal range thyroid function affects serum cholesterol levels, blood pressure, and type 2 diabetes risk: a mendelian randomization study. Thyroid. 2021; 31:721–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Depression in Patients with Subclinical Hypothyroidism: A Systematic Review and Meta-Analysis
- Subclinical Thyroid Dysfunction in the Elderly
- Plasma Lipid Concentrations and Blood Pressure in Women with Subclinical Hypothyroidism
- Comparison of Common Carotid Artery Intima-Media Thickness between Subclinical Hypothyroidism and Euthyroidism
- The Association between Subclinical Hypothyroidism and Cardiovascular Risk Factors in Post-menopausal Women