Endocrinol Metab.
2021 Aug;36(4):769-777. 10.3803/EnM.2021.1109.
Thyroid Hormone Profile and Its Prognostic Impact on the Coronavirus Disease 2019 in Korean Patients
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- KMID: 2519665
- DOI: http://doi.org/10.3803/EnM.2021.1109
Abstract
- Background
Data on the association between coronavirus disease 2019 (COVID-19) and thyroid have been reported, including overt thyrotoxicosis and suppression of thyroid function. We aimed to evaluate the thyroid hormone profile and its association with the prognosis of COVID-19 in Korean patients.
Methods
The clinical data of 119 patients with COVID-19, admitted in the Myongji Hospital, Goyang, South Korea, were retrospectively evaluated. The thyroid hormone profiles were analyzed and compared based on disease severity (non-severe disease vs. severe to critical disease). Clinical outcomes were analyzed according to the tertiles of thyroid hormones.
Results
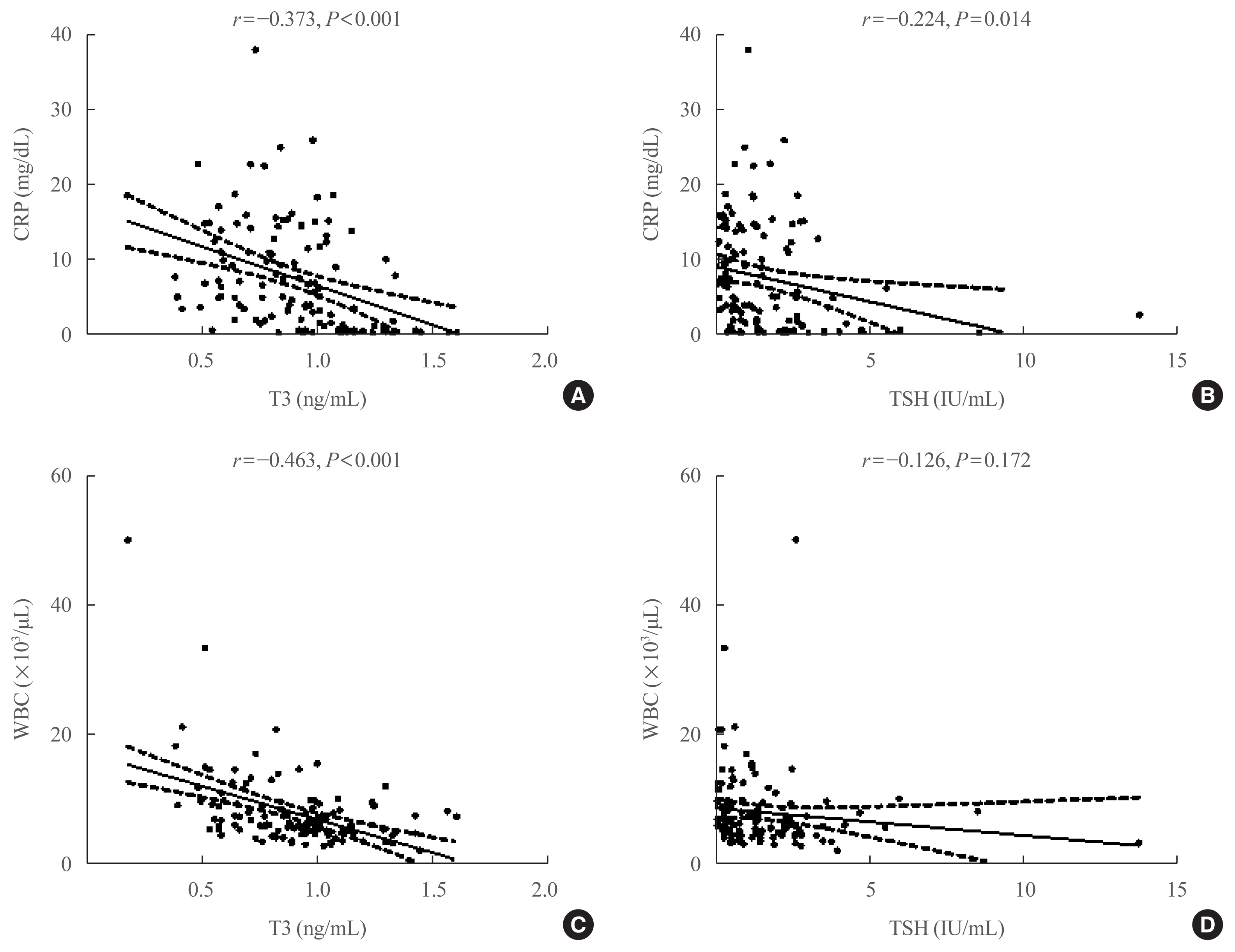
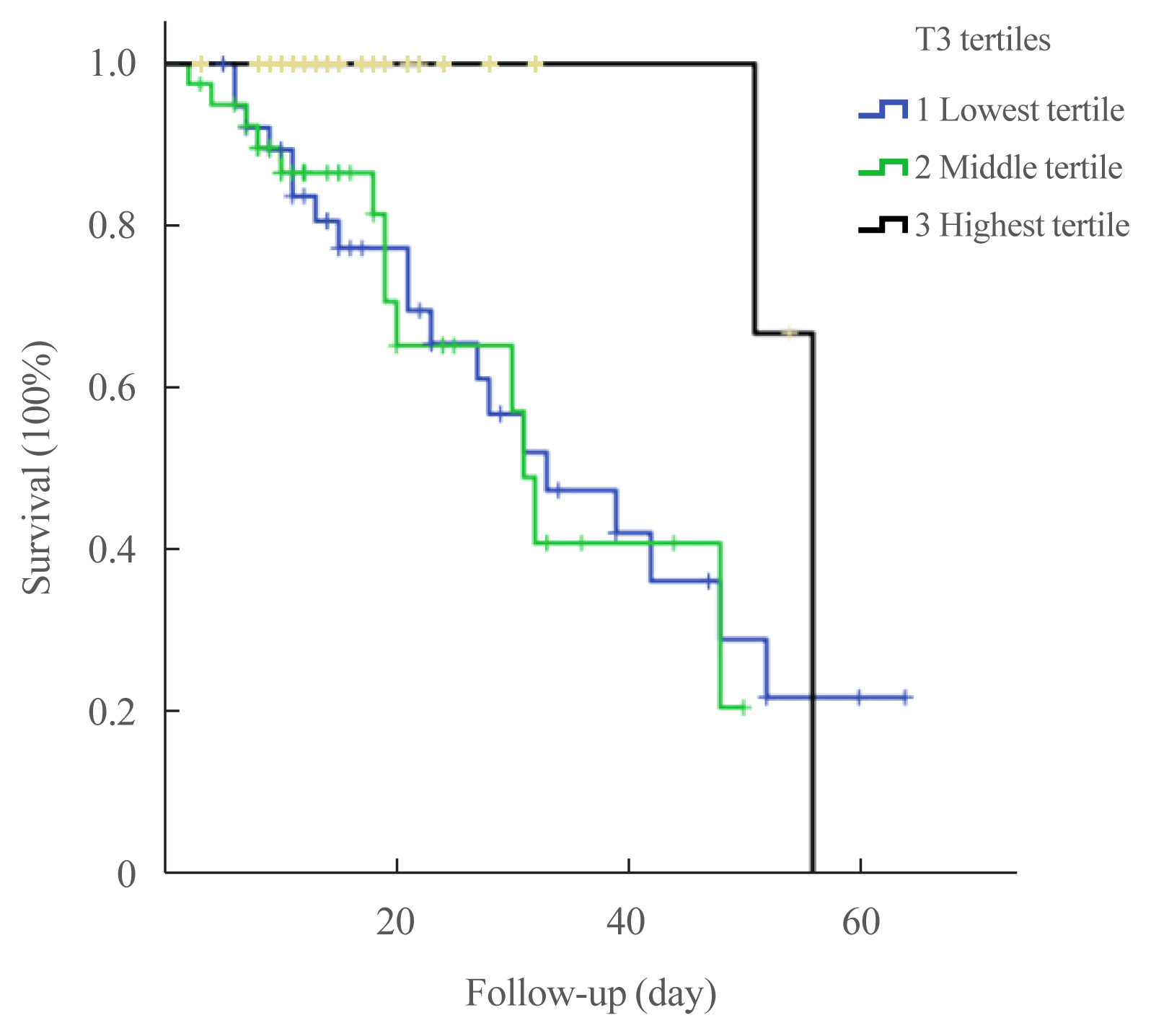
Of the 119 patients, 76 (63.9%) were euthyroid, and none presented with overt thyroid dysfunction. Non-thyroidal illness syndrome was the most common manifestation (18.5%), followed by subclinical thyrotoxicosis (14.3%) among patients with thyroid dysfunction. Thyroid stimulating hormone (TSH) and triiodothyronine (T3) levels were significantly lower in patients with severe to critical disease than in those with non-severe disease (P<0.05). Patients in the lowest T3 tertile (<0.77 ng/mL) had higher rates of mechanical ventilation, intensive care unit admission, and death than those in the middle and highest (>1.00 ng/mL) T3 tertiles (P<0.05). COVID-19 patients in the lowest T3 tertile were independently associated with mortality (hazard ratio, 5.27; 95% confidence interval, 1.09 to 25.32; P=0.038) compared with those in the highest T3 tertile.
Conclusion
Thyroid dysfunction is common in COVID-19 patients. Changes in serum TSH and T3 levels may be important markers of disease severity in COVID-19. Decreased T3 levels may have a prognostic significance in COVID-19 related outcome.
Figure
Reference
-
1. World Health Organization. Coronavirus disease (COVID-19) outbreak [Internet]. Geneva: WHO;2021. [cited 2021 Jul 24]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 .2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727–33.
Article3. Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020; 9:45.
Article4. Brancatella A, Ricci D, Cappellani D, Viola N, Sgro D, Santini F, et al. Is subacute thyroiditis an underestimated manifestation of SARS-CoV-2 infection? Insights from a case series. J Clin Endocrinol Metab. 2020; 105:dgaa537.
Article5. Lania A, Sandri MT, Cellini M, Mirani M, Lavezzi E, Mazziotti G. Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol. 2020; 183:381–7.
Article6. Ruggeri RM, Campenni A, Siracusa M, Frazzetto G, Gullo D. Subacute thyroiditis in a patient infected with SARS-COV-2: an endocrine complication linked to the COVID-19 pandemic. Hormones (Athens). 2021; 20:219–21.
Article7. Muller I, Cannavaro D, Dazzi D, Covelli D, Mantovani G, Muscatello A, et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020; 8:739–41.
Article8. Asfuroglu Kalkan E, Ates I. A case of subacute thyroiditis associated with COVID-19 infection. J Endocrinol Invest. 2020; 43:1173–4.
Article9. Chen M, Zhou W, Xu W. Thyroid function analysis in 50 patients with COVID-19: a retrospective study. Thyroid. 2021; 31:8–11.
Article10. Khoo B, Tan T, Clarke SA, Mills EG, Patel B, Modi M, et al. Thyroid function before, during, and after COVID-19. J Clin Endocrinol Metab. 2021; 106:e803–11.
Article11. Zou R, Wu C, Zhang S, Wang G, Zhang Q, Yu B, et al. Euthyroid sick syndrome in patients with COVID-19. Front Endocrinol (Lausanne). 2020; 11:566439.
Article12. Zhang Y, Lin F, Tu W, Zhang J, Choudhry AA, Ahmed O, et al. Thyroid dysfunction may be associated with poor outcomes in patients with COVID-19. Mol Cell Endocrinol. 2021; 521:111097.
Article13. Schwarz Y, Percik R, Oberman B, Yaffe D, Zimlichman E, Tirosh A. Sick euthyroid syndrome on presentation of patients with COVID-19: a potential marker for disease severity. Endocr Pract. 2021; 27:101–9.
Article14. Gao W, Guo W, Guo Y, Shi M, Dong G, Wang G, et al. Thyroid hormone concentrations in severely or critically ill patients with COVID-19. J Endocrinol Invest. 2021; 44:1031–40.
Article15. Van den Berghe G. Non-thyroidal illness in the ICU: a syndrome with different faces. Thyroid. 2014; 24:1456–65.
Article16. Su W, Zhao XQ, Wang M, Chen H, Li HW. Low T3 syndrome improves risk prediction of in-hospital cardiovascular death in patients with acute myocardial infarction. J Cardiol. 2018; 72:215–9.
Article17. Todd SR, Sim V, Moore LJ, Turner KL, Sucher JF, Moore FA. The identification of thyroid dysfunction in surgical sepsis. J Trauma Acute Care Surg. 2012; 73:1457–60.
Article18. Guo J, Hong Y, Wang Z, Li Y. Prognostic value of thyroid hormone FT3 in general patients admitted to the intensive care unit. Biomed Res Int. 2020; 2020:6329548.
Article19. Angelousi AG, Karageorgopoulos DE, Kapaskelis AM, Falagas ME. Association between thyroid function tests at baseline and the outcome of patients with sepsis or septic shock: a systematic review. Eur J Endocrinol. 2011; 164:147–55.
Article20. Wu Y, You S, Zang H, Liu H, Mao Y, Mao P, et al. Usefulness of serum thyroid-stimulation hormone (TSH) as a prognostic indicator for acute-on-chronic liver failure. Ann Hepatol. 2015; 14:218–24.
Article21. Ceresini G, Marina M, Lauretani F, Maggio M, Bandinelli S, Ceda GP, et al. Relationship between circulating thyroid-stimulating hormone, free thyroxine, and free triiodothyronine concentrations and 9-year mortality in euthyroid elderly adults. J Am Geriatr Soc. 2016; 64:553–60.
Article22. Lee KD, Lee SB, Lim JK, Kang YM, Kim IB, Moon HJ, et al. Providing essential clinical care for non-COVID-19 patients in a Seoul metropolitan acute care hospital amidst ongoing treatment of COVID-19 patients. J Hosp Infect. 2020; 106:673–7.
Article23. China National Health Commission. Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment (7th edition) [Internet]. Beijing: Chinese Society of Cardiology;2020. [cited 2021 Jul 24]. Available from: http://kjfy.meetingchina.org/msite/news/show/cn/3337.html .24. Lui DTW, Lee CH, Chow WS, Lee ACH, Tam AR, Fong CHY, et al. Role of non-thyroidal illness syndrome in predicting adverse outcomes in COVID-19 patients predominantly of mild-to-moderate severity. Clin Endocrinol (Oxf). 2021. Apr. 4. [Epub]. https://doi.org/10.1111/cen.14476 .
Article25. Docter R, van Toor H, Krenning EP, de Jong M, Hennemann G. Free thyroxine assessed with three assays in sera of patients with nonthyroidal illness and of subjects with abnormal concentrations of thyroxine-binding proteins. Clin Chem. 1993; 39:1668–74.
Article26. Peeters RP, Wouters PJ, Kaptein E, van Toor H, Visser TJ, Van den Berghe G. Reduced activation and increased inactivation of thyroid hormone in tissues of critically ill patients. J Clin Endocrinol Metab. 2003; 88:3202–11.
Article27. Monig H, Arendt T, Meyer M, Kloehn S, Bewig B. Activation of the hypothalamo-pituitary-adrenal axis in response to septic or non-septic diseases: implications for the euthyroid sick syndrome. Intensive Care Med. 1999; 25:1402–6.28. Wajner SM, Goemann IM, Bueno AL, Larsen PR, Maia AL. IL-6 promotes nonthyroidal illness syndrome by blocking thyroxine activation while promoting thyroid hormone inactivation in human cells. J Clin Invest. 2011; 121:1834–45.
Article29. McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020; 19:102537.
Article30. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine storm’ in COVID-19. J Infect. 2020; 80:607–13.
Article31. Tan T, Khoo B, Mills EG, Phylactou M, Patel B, Eng PC, et al. Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol. 2020; 8:659–60.
Article32. Torpy DJ, Tsigos C, Lotsikas AJ, Defensor R, Chrousos GP, Papanicolaou DA. Acute and delayed effects of a single-dose injection of interleukin-6 on thyroid function in healthy humans. Metabolism. 1998; 47:1289–93.
Article33. Wei L, Sun S, Zhang J, Zhu H, Xu Y, Ma Q, et al. Endocrine cells of the adenohypophysis in severe acute respiratory syndrome (SARS). Biochem Cell Biol. 2010; 88:723–30.34. Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS, et al. C-reactive protein and clinical outcomes in patients with COVID-19. Eur Heart J. 2021; 42:2270–9.
Article35. Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020; 146:110–8.
Article36. Wang Z. Identification of risk factors for in-hospital death of COVID-19 pneumonia-lessions from the early outbreak. BMC Infect Dis. 2021; 21:113.37. Chang MC, Hwang JM, Jeon JH, Kwak SG, Park D, Moon JS. Fasting plasma glucose level independently predicts the mortality of patients with coronavirus disease 2019 infection: a multicenter, retrospective cohort study. Endocrinol Metab (Seoul). 2020; 35:595–601.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bisphenols and Thyroid Hormone
- Best Achievements in Clinical Thyroidology in 2020
- Clinical Impact of Empirical Antibiotic Therapy in Patients With Coronavirus Disease 2019 Requiring Oxygen Therapy
- Resistance to thyroid hormone due to a novel mutation of thyroid hormone receptor beta gene
- Monogenic Thyroid Disorder