Acute Crit Care.
2021 Aug;36(3):269-273. 10.4266/acc.2021.00626.
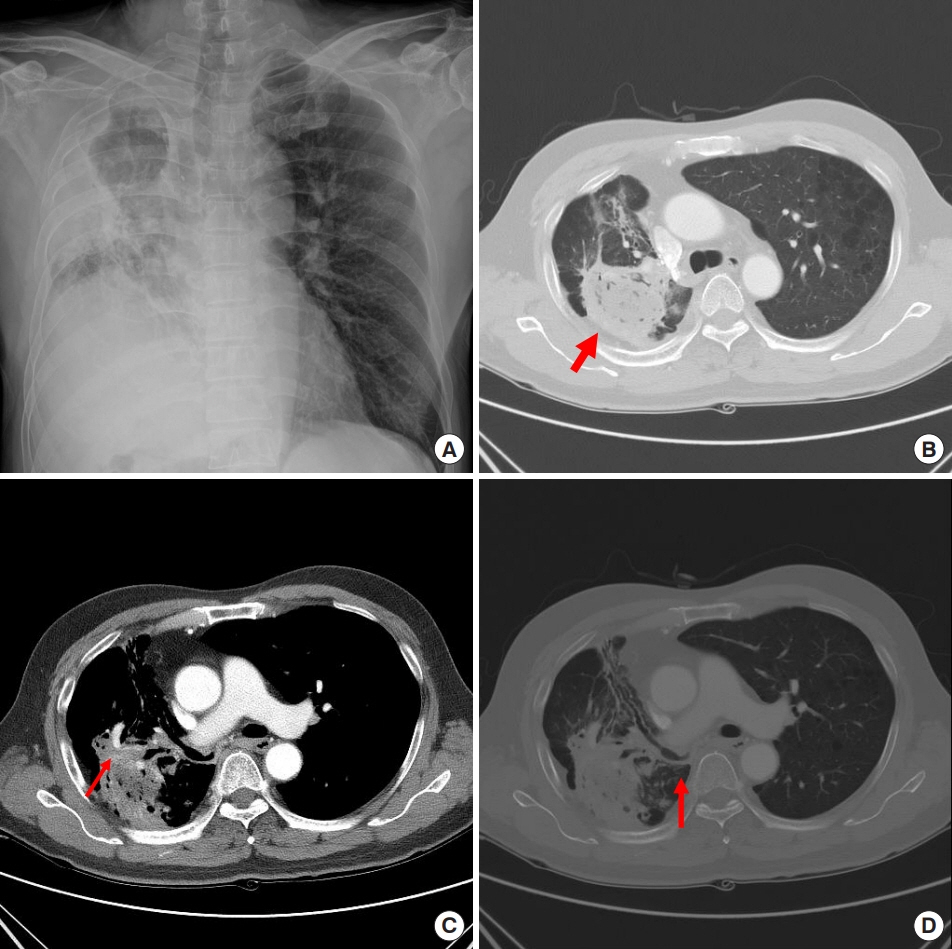
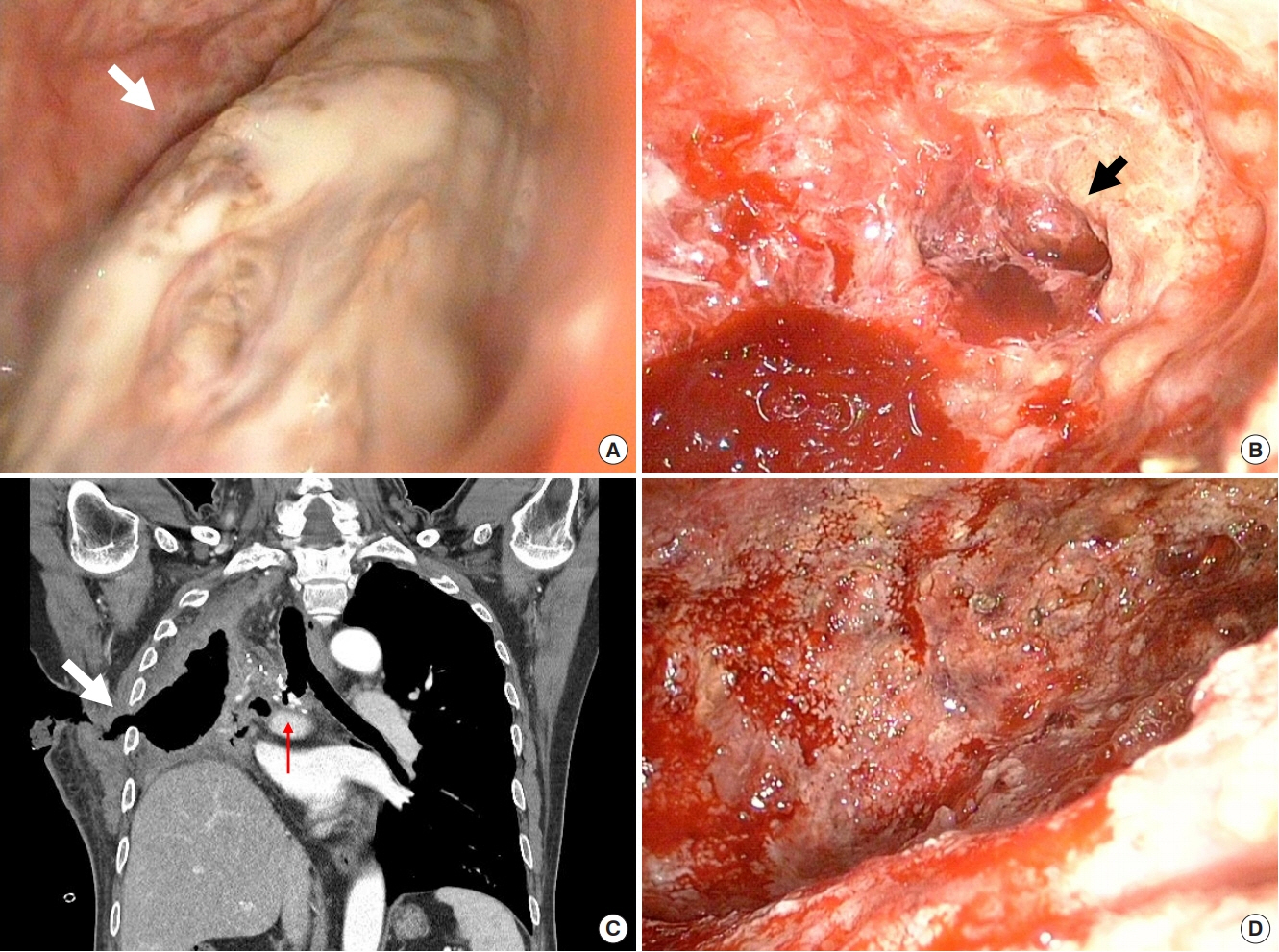
Thoracomyoplasty and perioperative negative wound pressure therapy for bronchopleural fistula after trans-sternal bronchial closure
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Department of Critical Care Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Division of Pulmonology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- KMID: 2519456
- DOI: http://doi.org/10.4266/acc.2021.00626
Figure
Reference
-
1. Abruzzini P. Surgical treatment of fistulae of the main bronchus after pneumonectomy in tuberculosis (personal technic). Thoraxchirurgie. 1963; 10:259–64.2. Fournier I, Krueger T, Wang Y, Meyer A, Ris HB, Gonzalez M. Tailored thoracomyoplasty as a valid treatment option for chronic postlobectomy empyema. Ann Thorac Surg. 2012; 94:387–93.
Article3. Botianu PV, Botianu AM. Thoracomyoplasty in the treatment of empyema: current indications, basic principles, and results. Pulm Med. 2012; 2012:418514.
Article4. Hysi I, Rousse N, Claret A, Bellier J, Pinçon C, Wallet F, et al. Open window thoracostomy and thoracoplasty to manage 90 postpneumonectomy empyemas. Ann Thorac Surg. 2011; 92:1833–9.
Article5. Haghshenasskashani A, Rahnavardi M, Yan TD, McCaughan BC. Intrathoracic application of a vacuum-assisted closure device in managing pleural space infection after lung resection: is it an option? Interact Cardiovasc Thorac Surg. 2011; 13:168–74.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Postpneumonectomy Empyema with Bronchopleural Fistula Treated with Vacuum-assisted Closure Device
- Use of the Free Flap for Large Defect with Bronchopleural Fistula: Case Report
- Endobronchial Closure of Postoperative Bronchopleural Fistula Using Vascular Occluding Coils
- Various Bronchial Fistulas: Pitfalls and Usefulness on CT. A Pictorial Review
- Bronchopleural Fistula after Pneumonectomy: Autosuture Versus Manual Suture