Impact of prone position on outcomes of COVID-19 patients with spontaneous breathing
- Affiliations
-
- 1Department of Intensive Care, Habib Bourguiba University Hospital and Sfax University, Sfax, Tunisia
- 2Department of Radiology, Habib Bourguiba University Hospital and Sfax University, Sfax, Tunisia
- KMID: 2519447
- DOI: http://doi.org/10.4266/acc.2021.00500
Abstract
- Background
In this study, we explored whether early application of the prone position (PP) can improve severe hypoxemia and respiratory failure in coronavirus disease 2019 (COVID-19) patients with spontaneous breathing.
Methods
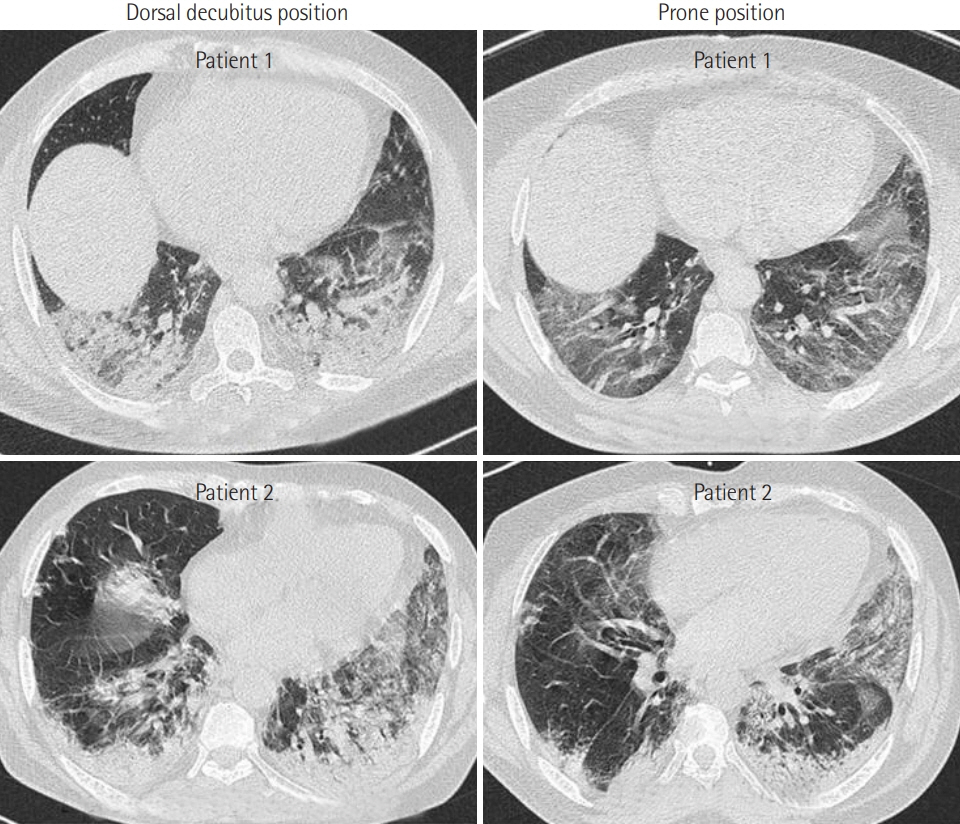
This is a prospective observational study of severe, critically ill adult COVID-19 patients admitted to the intensive care unit. All vital parameters were recorded in real time for all patients. Moreover, the results of chest computed tomography (CT), when available, were analyzed.
Results
PP was applied in 21 patients who were breathing spontaneously. The application of PP was associated with a significant increase in oxygen saturation measured by pulse oximetry (SpO2) from 82%±12% to 96%±3% (P<0.001) 1 hour later. Moreover, PP was associated with a significant reduction in respiratory rate from 31±10 to 21±4 breaths/min (P<0.001). Furthermore, the number of patients who exhibited signs of respiratory distress after PP was reduced from 10 (47%) to 3 (14%) (P=0.04). Early PP application also led to a clear improvement on CT imaging. It was not, however, associated with a reduction in mortality rate or in the use of invasive mechanical ventilation (P>0.05 for both).
Conclusions
Our study confirmed that the early application of PP can improve hypoxemia and tachypnea in COVID-19 patients with spontaneous breathing. Randomized controlled trials are needed to confirm the beneficial effects of PP in COVID-19 patients with spontaneous breathing.
Figure
Cited by 3 articles
-
Gravity-induced ischemia in the brain-and prone positioning for COVID-19 patients breathing spontaneously
J. Howard Jaster, Giulia Ottaviani
Acute Crit Care. 2022;37(1):131-133. doi: 10.4266/acc.2021.01739.Gravity-induced ischemia in the brain and prone positioning for COVID-19 patients breathing spontaneously: still far from the truth!
Mabrouk Bahloul, Sana Kharrat, Kamilia Chtara, Hedi Chelly, Chokri Ben Hamida, Mounir Bouaziz
Acute Crit Care. 2022;37(1):134-136. doi: 10.4266/acc.2022.00199.Awake prone positioning for COVID-19 acute hypoxemic respiratory failure in Tunisia
Khaoula Ben Ismail, Fatma Essafi, Imen Talik, Najla Ben Slimene, Ines Sdiri, Boudour Ben Dhia, Takoua Merhbene
Acute Crit Care. 2023;38(3):271-277. doi: 10.4266/acc.2023.00591.
Reference
-
1. Worldometer. Coronavirus update [Internet]. Worldometer;2020 [cited 2020 Jul 24]. Available from: https://www.worldometers.info/coronavirus/.2. Vetter P, Vu DL, L’Huillier AG, Schibler M, Kaiser L, Jacquerioz F. Clinical features of covid-19. BMJ. 2020; 369:m1470.
Article3. Bahloul M, Ketata W, Lahyeni D, Mayoufi H, Kotti A, Smaoui F, et al. Pulmonary capillary leak syndrome following COVID-19 virus infection. J Med Virol. 2021; 93:94–6.
Article4. Ferrando C, Mellado-Artigas R, Gea A, Arruti E, Aldecoa C, Adalia R, et al. Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care. 2020; 24:597.
Article5. Coppo A, Bellani G, Winterton D, Di Pierro M, Soria A, Faverio P, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020; 8:765–74.
Article6. Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad Emerg Med. 2020; 27:375–8.
Article7. Telias I, Katira BH, Brochard L. Is the prone position helpful during pontaneous breathing in patients with COVID-19? JAMA. 2020; 323:2265–7.8. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993; 270:2957–63.
Article9. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286:1754–8.
Article10. Hallifax RJ, Porter BM, Elder PJ, Evans SB, Turnbull CD, Hynes G, et al. Successful awake proning is associated with improved clinical outcomes in patients with COVID-19: single-centre high-dependency unit experience. BMJ Open Respir Res. 2020; 7:e000678.
Article11. Luks AM, Swenson ER. Pulse oximetry for monitoring patients with COVID-19 at home: potential pitfalls and practical guidance. Ann Am Thorac Soc. 2020; 17:1040–6.
Article12. Venus K, Munshi L, Fralick M. Prone positioning for patients with hypoxic respiratory failure related to COVID-19. CMAJ. 2020; 192:E1532–7.
Article13. Damarla M, Zaeh S, Niedermeyer S, Merck S, Niranjan-Azadi A, Broderick B, et al. Prone positioning of nonintubated patients with COVID-19. Am J Respir Crit Care Med. 2020; 202:604–6.
Article14. Ponnapa Reddy M, Subramaniam A, Afroz A, Billah B, Lim ZJ, Zubarev A, et al. Prone positioning of nonintubated patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care Med. 2021; Apr. 30. [Epub]. https://doi.org/10.1097/CCM.0000000000005086.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Awake prone positioning for COVID-19 acute hypoxemic respiratory failure in Tunisia
- The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department
- Impact of solid organ transplantation on the effectiveness of COVID-19 vaccination in hospitalized patients with COVID-19: a propensity score-matched cohort study
- Impact of liver cirrhosis on the clinical outcomes of patients with COVID-19: a nationwide cohort study of Korea
- The coronavirus disease 2019 pandemic and chronic diseases