Korean J Gastroenterol.
2021 Aug;78(2):144-146. 10.4166/kjg.2021.104.
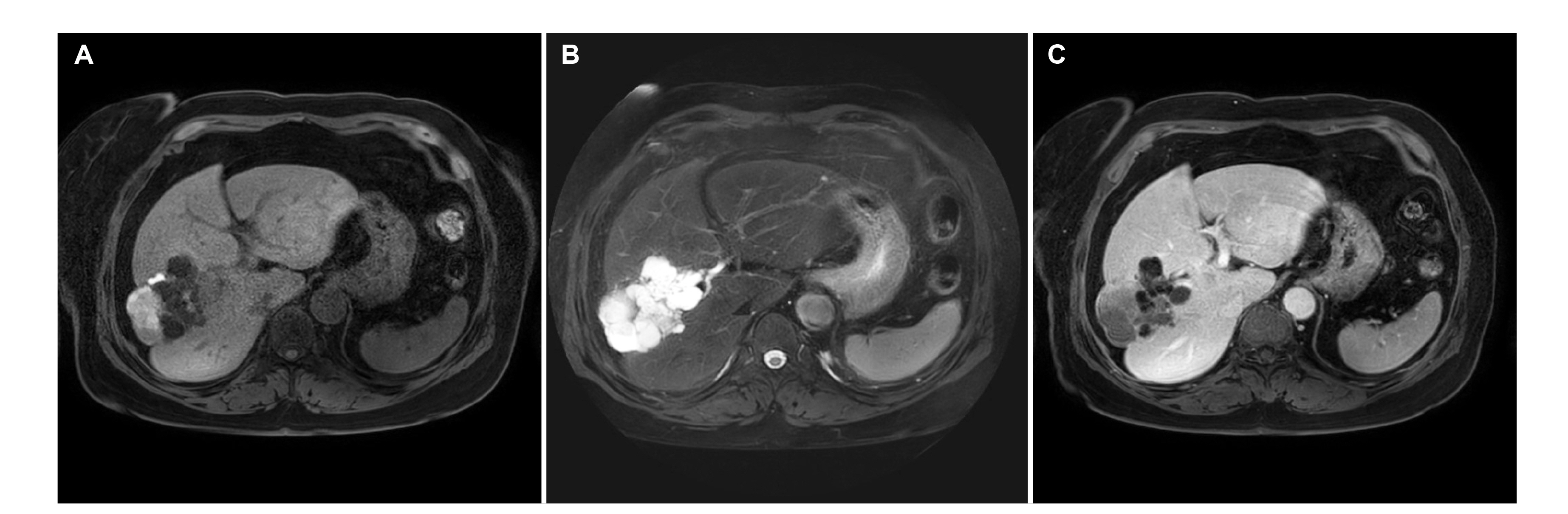
Mucinous Cystic Neoplasm of the Liver Mimicking Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- Affiliations
-
- 1Departments of Gastroenterology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 2Departments of Radiology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 3Departments of Pathology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- KMID: 2519384
- DOI: http://doi.org/10.4166/kjg.2021.104
Figure
Reference
-
1. Kunovsky L, Kala Z, Svaton R, et al. 2018; Mucinous cystic neoplasm of the liver or intraductal papillary mucinous neoplasm of the bile duct? A case report and a review of literature. Ann Hepatol. 17:519–524. DOI: 10.5604/01.3001.0011.7397. PMID: 29735801.
Article2. Kubota K, Nakanuma Y, Kondo F, et al. 2014; Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 21:76–185. DOI: 10.1002/jhbp.23. PMID: 23908126.
Article3. Nakayama Y, Kato Y, Okubo S, et al. 2015; A case of mucinous cystic neoplasm of the liver: a case report. Surg Case Rep. 1:9. DOI: 10.1186/s40792-014-0007-z. PMID: 26943377. PMCID: PMC4747937.
Article4. Li T, Ji Y, Zhi XT, et al. 2009; A comparison of hepatic mucinous cystic neoplasms with biliary intraductal papillary neoplasms. Clin Gastroenterol Hepatol. 7:586–593. DOI: 10.1016/j.cgh.2009.02.019. PMID: 19245849.
Article5. Zen Y, Pedica F, Patcha VR, et al. 2011; Mucinous cystic neoplasms of the liver: a clinicopathological study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol. 4:1079–1089. DOI: 10.1038/modpathol.2011.71. PMID: 21516077.
Article6. Wang X, Cai YQ, Chen YH, Liu XB. 2015; Biliary tract intraductal papillary mucinous neoplasm: report of 19 cases. World J Gastroenterol. 21:4261–4267. DOI: 10.3748/wjg.v21.i14.4261. PMID: 25892877. PMCID: PMC4394088.
Article7. Budzynska A, Hartleb M, Nowakowska-Dulawa E, Krol R, Remiszewski P, Mazurkiewicz M. 2014; Simultaneous liver mucinous cystic and intraductal papillary mucinous neoplasms of the bile duct: a case report. World J Gastroenterol. 20:4102–4105. DOI: 10.3748/wjg.v20.i14.4102. PMID: 24744602. PMCID: PMC3983469.
Article8. Zen Y, Jang KT, Ahn S, et al. 2014; Intraductal papillary neoplasms and mucinous cystic neoplasms of the hepatobiliary system: demographic differences between Asian and Western populations, and comparison with pancreatic counterparts. Histopathology. 65:164–173. DOI: 10.1111/his.12378. PMID: 24456415.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- Pedunculated mucinous cystic neoplasm of the liver: a case report
- Oncocytic Type Intraductal Papillary Mucinous Neoplasm Mimicking Mucinous Cystic Neoplasm of the Pancreas: A Case Report
- Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
- Unexpected Metastasis of Intraductal Papillary Mucinous Neoplasm of the Bile Duct into Thoracic Cavity with Direct Extension: Case Report