Clin Exp Otorhinolaryngol.
2021 Aug;14(3):338-346. 10.21053/ceo.2020.02180.
Real-Time Light-Guided Vocal Fold Injection: an In Vivo Feasibility Study in a Canine Model
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, The Dongnam Institute of Radiological and Medical Sciences (DIRAMS), Busan, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2519189
- DOI: http://doi.org/10.21053/ceo.2020.02180
Abstract
Objectives
. The transcutaneous approach is a good option for office-based vocal fold injection (VFI). However, precise localization requires extensive experience because the needle tip is invisible in small and complex laryngeal spaces. Recently, real-time light-guided VFI (RL-VFI) was proposed as a new technique that allows simultaneous injection under precise needle localization by light guidance. Herein, we aimed to verify the feasibility of RL-VFI in an in vivo canine model and explored its clinical usefulness.
Methods
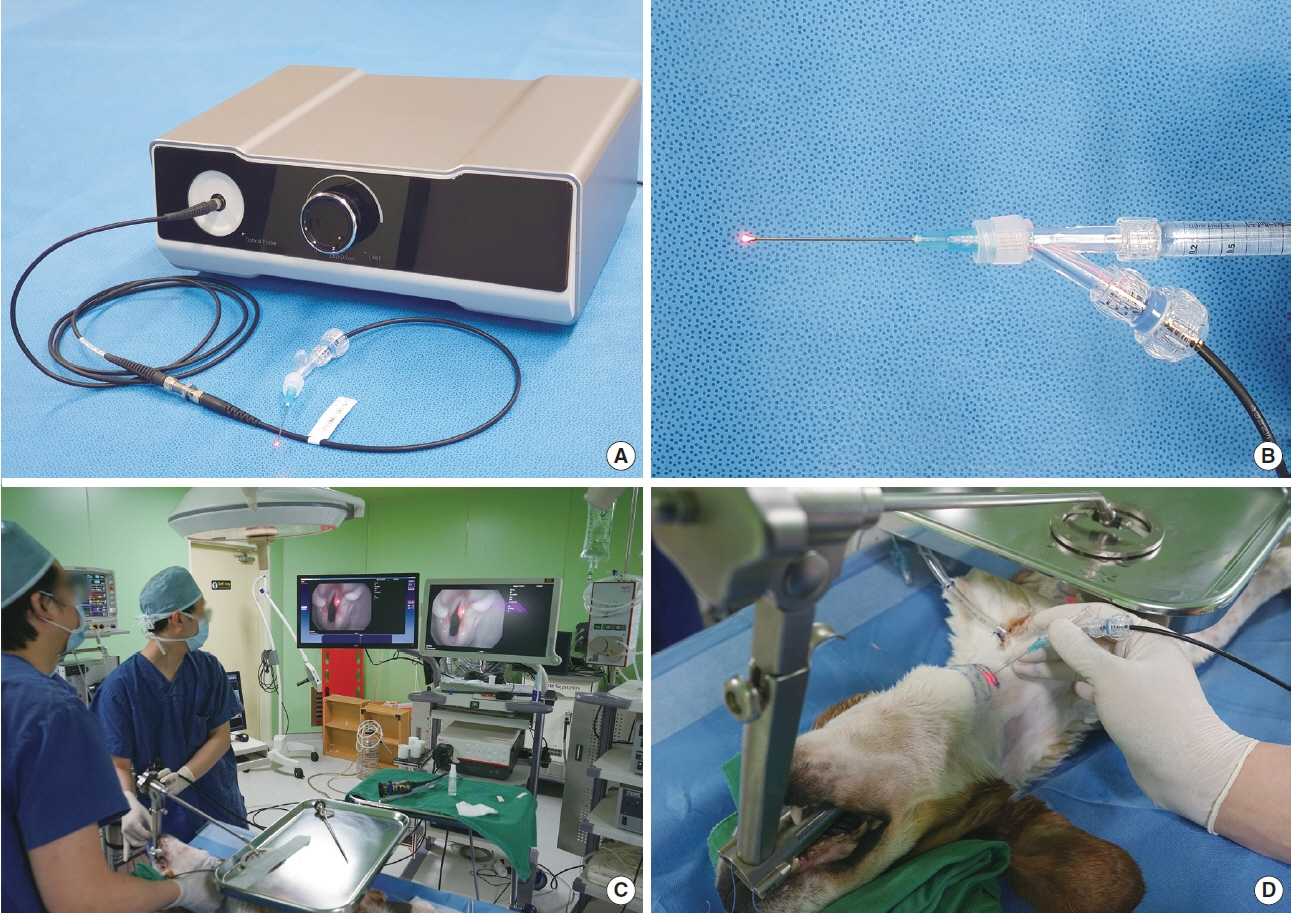
. The device for RL-VFI comprised a light source (light-emitting diode modules [10 W] of red color [650 nm]) and injectors (1.5 inches, 23 gauge). An adult male beagle was used for the experiment. After tracheostomy, a rigid laryngoscope was inserted and suspended to expose the larynx. A flexible naso-laryngoscopy system was used to visualize the vocal folds.
Results
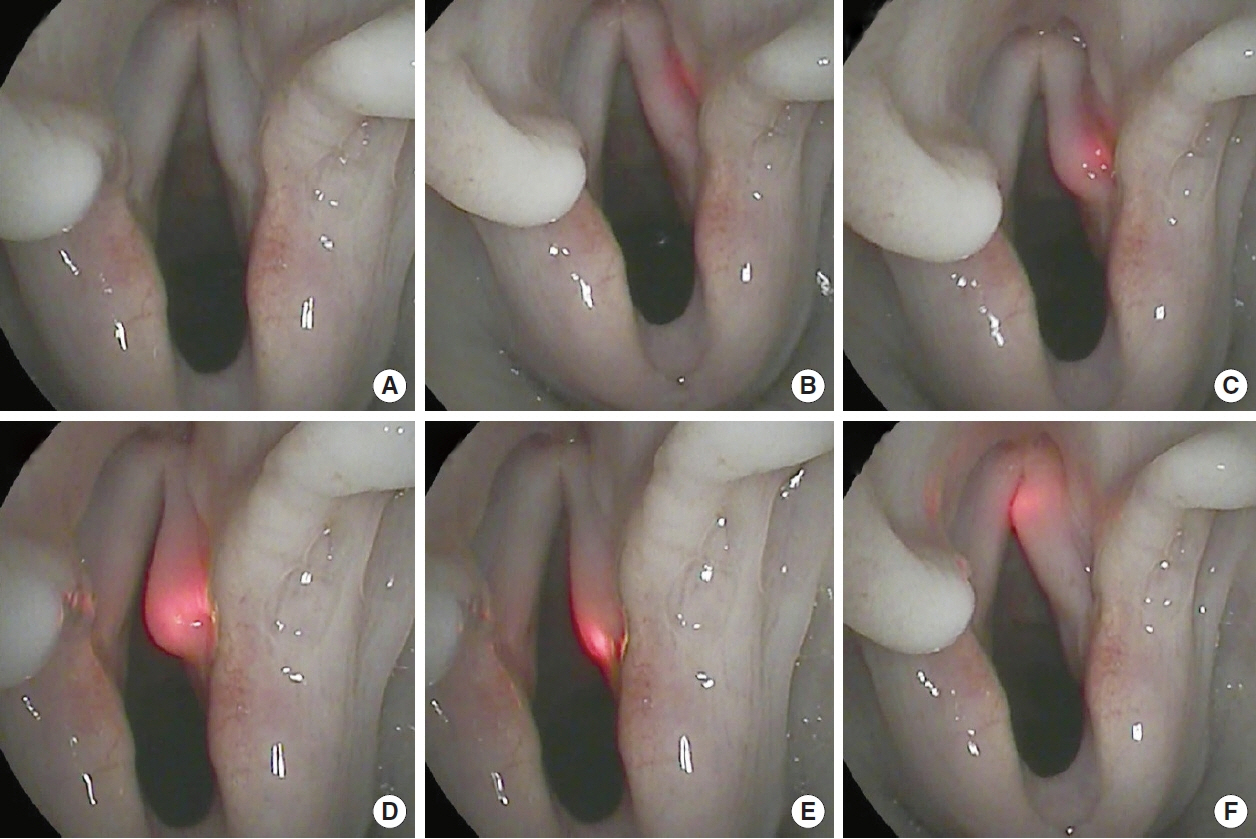
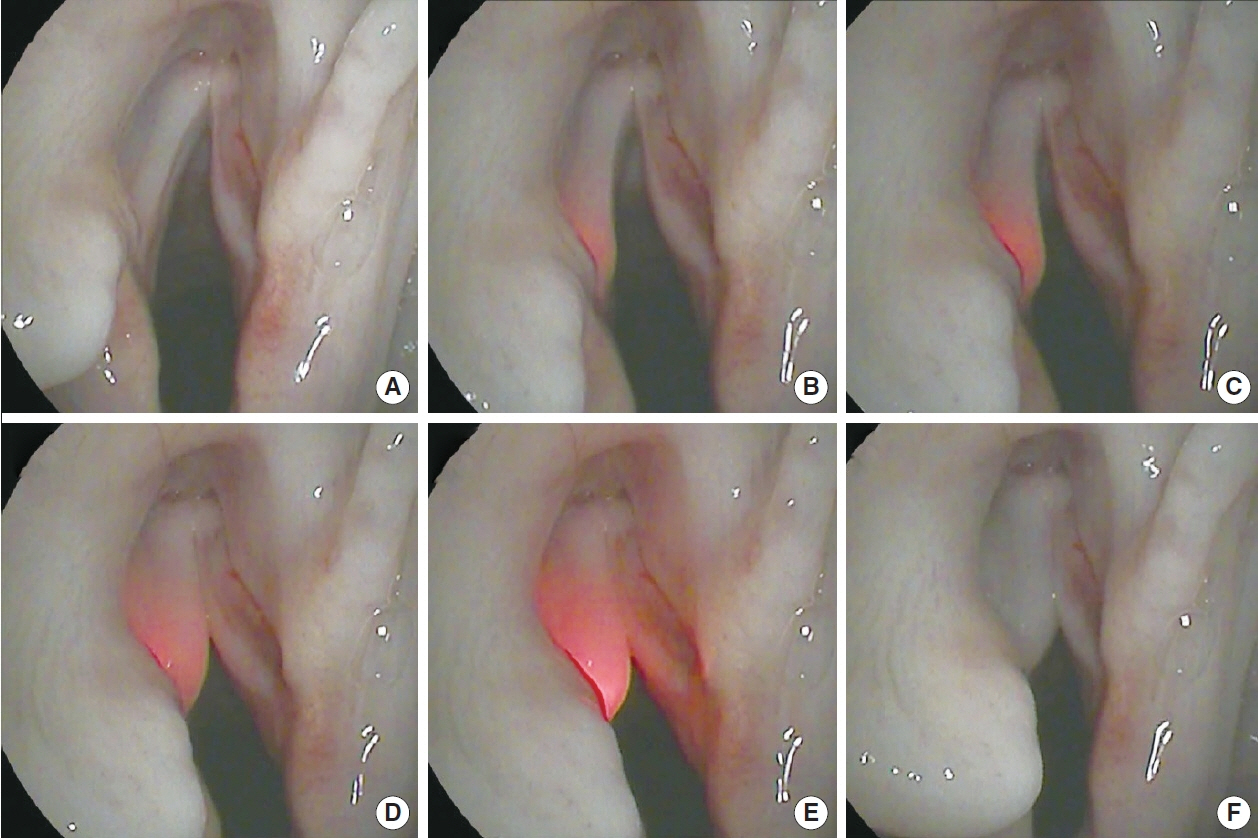
. RL-VFI was performed using various transcutaneous approaches, including the cricothyroid, transthyroid, and transhyoid approaches. Light guidance helped identify the path of the needle and prevent inadvertent penetration. The location of the needle tip was accurately indicated by the light. The illuminated needle could be easily placed at the intended points in the vocal fold with real-time visual-motor feedback. Hyaluronic acid could be simultaneously injected lateral to the vocal process under light guidance without manipulation of the device.
Conclusion
. RL-VFI was found to be safe and feasible in an in vivo canine model, providing precise localization and visualmotor feedback. The clinical application of RL-VFI is expected to improve the safety and precision of VFI.
Keyword
Figure
Reference
-
1. Rosen CA, Amin MR, Sulica L, Simpson CB, Merati AL, Courey MS, et al. Advances in office-based diagnosis and treatment in laryngology. Laryngoscope. 2009; Nov. 119 Suppl 2:S185–212.
Article2. Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clin Exp Otorhinolaryngol. 2010; Dec. 3(4):177–82.
Article3. Kwon TK, Buckmire R. Injection laryngoplasty for management of unilateral vocal fold paralysis. Curr Opin Otolaryngol Head Neck Surg. 2004; Dec. 12(6):538–42.
Article4. Cha W, Ro JH, Wang SG, Jang JY, Cho JK, Kim GH, et al. Development of a device for real-time light-guided vocal fold injection: a preliminary report. Laryngoscope. 2016; Apr. 126(4):936–40.
Article5. Cha W, Ro JH, Yang SC, Choi CJ, Yang I, Kang H, et al. Real-time light-guided vocal fold injection: ex vivo feasibility study in a canine model. Laryngoscope. 2019; Apr. 129(4):935–42.6. Lee SW, Kim JW, Koh YW, Shim SS, Son YI. Comparative analysis of efficiency of injection laryngoplasty technique for with or without neck treatment patients: a transcartilaginous approach versus the cricothyroid approach. Clin Exp Otorhinolaryngol. 2010; Mar. 3(1):37–41.
Article7. Chhetri DK, Jamal N. Percutaneous injection laryngoplasty. Laryngoscope. 2014; Mar. 124(3):742–5.
Article8. Achkar J, Song P, Andrus J, Franco R Jr. Double-bend needle modification for transthyrohyoid vocal fold injection. Laryngoscope. 2012; Apr. 122(4):865–7.
Article9. Amin MR. Thyrohyoid approach for vocal fold augmentation. Ann Otol Rhinol Laryngol. 2006; Sep. 115(9):699–702.
Article10. Zeitler DM, Amin MR. The thyrohyoid approach to in-office injection augmentation of the vocal fold. Curr Opin Otolaryngol Head Neck Surg. 2007; Dec. 15(6):412–6.
Article11. Rees CJ, Mouadeb DA, Belafsky PC. Thyrohyoid vocal fold augmentation with calcium hydroxyapatite. Otolaryngol Head Neck Surg. 2008; Jun. 138(6):743–6.
Article12. Pearson W, Hutchinson CT, Noordzij JP. Accessing the vocal folds by transcutaneous injection. Clin Anat. 2010; Apr. 23(3):270–6.
Article13. Clary MS, Milam BM, Courey MS. Office-based vocal fold injection with the laryngeal introducer technique. Laryngoscope. 2014; Sep. 124(9):2114–7.
Article14. Hoffman HT, Dailey SH, Bock JM, Thibeault SL, McCulloch TM. Transillumination for needle localization in the larynx. Laryngoscope. 2015; Oct. 125(10):2341–8.
Article15. Statistics Korea; National Health Insurance Corporation Healthcare Bigdata Hub; Health Insurance Review & Assessment Service. Statistics of vocal fold injection, thyroplasty and arytenoid adduction using operation code by O1264, O1265 and O1266 [Internet]. Wonju: Health Insurance Review & Assessment Service;2017 [cited 2020 Oct 6]. Available from: http://opendata.hira.or.kr/op/opc/olapDiagBhvInfo.do.16. Jin SM, Park CY, Lee JK, Ban JH, Lee SH, Lee KC. Transcutaneous injection laryngoplasty through the cricothyroid space in the sitting position: anatomical information and technique. Eur Arch Otorhinolaryngol. 2008; Mar. 265(3):313–9.
Article17. Su MC, Yeh TH, Tan CT, Lin CD, Linne OC, Lee SY. Measurement of adult vocal fold length. J Laryngol Otol. 2002; Jun. 116(6):447–9.
Article18. Chheda NN, Rosen CA, Belafsky PC, Simpson CB, Postma GN. Revision laryngeal surgery for the suboptimal injection of calcium hydroxylapatite. Laryngoscope. 2008; Dec. 118(12):2260–3.
Article19. Kim J, Seo HS, Na HS, Son HY, Lee DK, Jeong WJ, et al. Real-time light-guided vocal fold injection as a simulation-based training tool. Auris Nasus Larynx. 2020. Aug. 12:[Epub]. https://doi.org/10.1016/j.anl.2020.07.011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Clinical Application of Real-Time Light-Guided Vocal Fold Injection
- Vocal Fold Injection: Review of Indications, Techniques, and Materials for Augmentation
- Real-Time Light-Guided Vocal Fold Injection via the Cricothyroid Membrane in Unilateral Vocal Fold Paralysis: A Human Pilot Study
- Function of the interarytenoid(IA) muscle in phonation: in vivo laryngeal model
- Histology and Stroboscopic Findings after Injection of Artecoll(R) and Restylane(R) into Paralyzed Canine Vocal Fold: in vivo Canine Study