Nutr Res Pract.
2021 Aug;15(4):468-478. 10.4162/nrp.2021.15.4.468.
Association between dietary omega-3 fatty acid intake and depression in postmenopausal women
- Affiliations
-
- 1Department of Food and Nutrition, Yeungnam University, Gyeongsan 38541, Korea
- KMID: 2518757
- DOI: http://doi.org/10.4162/nrp.2021.15.4.468
Abstract
- BACKGROUND/OBJECTIVES
This study aimed to analyze the association between dietary omega-3 fatty acid intake and depression in postmenopausal women using data from the Korea National Health and Nutrition Examination Survey (KNHANES) VI.
SUBJECTS/METHODS
The KNHANES is a cross-sectional nationwide health and nutrition survey. Dietary data, including omega-3 fatty acids, were assessed using the 24-h recall method. Depression was evaluated using a survey questionnaire. The association between dietary omega-3 fatty acids and depression was evaluated using multivariate logistic regression analysis. Depression, according to the dietary omega-3 fatty acid intake, was expressed as the odds ratio (OR) with a 95% confidence interval (CI). A total of 4,150 postmenopausal women were included in the analysis.
RESULTS
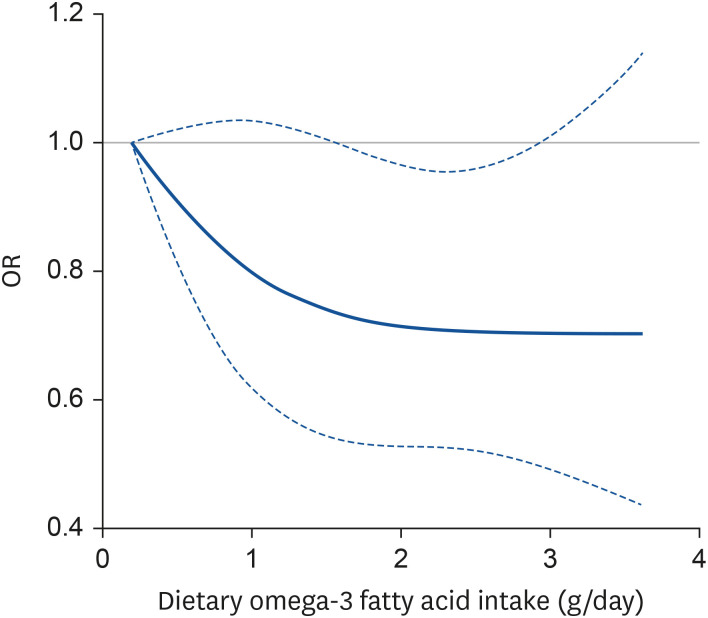
In the fully-adjusted model, the group with the highest dietary omega-3 fatty acid intake significantly showed lower prevalence of depression than the group with the lowest intake (OR, 0.52; 95% CI, 0.33–0.83); a significant linear trend was detected (P for trend = 0.04). According to the dose-response analysis using cubic restricted spline regression, this association was linear and monotonic (P for non-linearity = 0.32).
CONCLUSIONS
In this study, the dietary omega-3 fatty acid intake in postmenopausal women was inversely proportional to depression in a dose-response manner. Large cohort studies are needed to verify the causality between omega-3 fatty acids and depression in Korean postmenopausal women.
Keyword
Figure
Reference
-
1. World Health Organization. Research on the Menopause in the 1990s. Geneva: World Health Organization;1996. p. 12–14.2. Oppermann K, Fuchs SC, Donato G, Bastos CA, Spritzer PM. Physical, psychological, and menopause-related symptoms and minor psychiatric disorders in a community-based sample of Brazilian premenopausal, perimenopausal, and postmenopausal women. Menopause. 2012; 19:355–360. PMID: 21971211.
Article3. Freeman EW, Sammel MD, Lin H, Gracia CR, Pien GW, Nelson DB, Sheng L. Symptoms associated with menopausal transition and reproductive hormones in midlife women. Obstet Gynecol. 2007; 110:230–240. PMID: 17666595.
Article4. Joffe H, Hall JE, Soares CN, Hennen J, Reilly CJ, Carlson K, Cohen LS. Vasomotor symptoms are associated with depression in perimenopausal women seeking primary care. Menopause. 2002; 9:392–398. PMID: 12439097.
Article5. de Kruif M, Spijker AT, Molendijk ML. Depression during the perimenopause: a meta-analysis. J Affect Disord. 2016; 206:174–180. PMID: 27475888.
Article6. Molendijk M, Molero P, Ortuño Sánchez-Pedreño F, Van der Does W, Angel Martínez-González M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. 2018; 226:346–354. PMID: 29031185.
Article7. Grosso G, Micek A, Marventano S, Castellano S, Mistretta A, Pajak A, Galvano F. Dietary n-3 PUFA, fish consumption and depression: a systematic review and meta-analysis of observational studies. J Affect Disord. 2016; 205:269–281. PMID: 27544316.
Article8. Bai ZG, Bo A, Wu SJ, Gai QY, Chi I. Omega-3 polyunsaturated fatty acids and reduction of depressive symptoms in older adults: a systematic review and meta-analysis. J Affect Disord. 2018; 241:241–248. PMID: 30138808.
Article9. Giacobbe J, Benoiton B, Zunszain P, Pariante CM, Borsini A. The anti-inflammatory role of omega-3 polyunsaturated fatty acids metabolites in pre-clinical models of psychiatric, neurodegenerative, and neurological disorders. Front Psychiatry. 2020; 11:122. PMID: 32180741.
Article10. Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006; 63:385–390. PMID: 16585467.11. Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006; 63:375–382. PMID: 16585466.
Article12. Bromberger JT, Assmann SF, Avis NE, Schocken M, Kravitz HM, Cordal A. Persistent mood symptoms in a multiethnic community cohort of pre- and perimenopausal women. Am J Epidemiol. 2003; 158:347–356. PMID: 12915500.
Article13. Brinton RD, Tran J, Proffitt P, Montoya M. 17 Beta-estradiol enhances the outgrowth and survival of neocortical neurons in culture. Neurochem Res. 1997; 22:1339–1351. PMID: 9355106.14. Keenan PA, Ezzat WH, Ginsburg K, Moore GJ. Prefrontal cortex as the site of estrogen’s effect on cognition. Psychoneuroendocrinology. 2001; 26:577–590. PMID: 11403979.
Article15. Borrow AP, Cameron NM. Estrogenic mediation of serotonergic and neurotrophic systems: implications for female mood disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2014; 54:13–25. PMID: 24865152.
Article16. Decsi T, Kennedy K. Sex-specific differences in essential fatty acid metabolism. Am J Clin Nutr. 2011; 94:1914S–1919S. PMID: 22089435.
Article17. Freeman MP, Hibbeln JR, Silver M, Hirschberg AM, Wang B, Yule AM, Petrillo LF, Pascuillo E, Economou NI, Joffe H, et al. Omega-3 fatty acids for major depressive disorder associated with the menopausal transition: a preliminary open trial. Menopause. 2011; 18:279–284. PMID: 21037490.18. Masoumi SZ, Kazemi F, Tavakolian S, Rahimi A, Oshvandi K, Soltanian A, Shobeiri F. Effect of citalopram in combination with omega-3 on depression in post-menopausal women: a triple blind randomized controlled trial. J Clin Diagn Res. 2016; 10:QC01–05.19. Yang Y, Je Y. Fish consumption and depression in Korean adults: the Korea National Health and Nutrition Examination Survey, 2013–2015. Eur J Clin Nutr. 2018; 72:1142–1149. PMID: 29339828.
Article20. Park SJ, Lee DK, Kim B, Na KS, Lee CH, Son YD, Lee HJ. The association between omega-3 fatty acid intake and human brain connectivity in middle-aged depressed women. Nutrients. 2020; 12:2191.
Article21. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID: 24585853.
Article22. Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986; 124:17–27. PMID: 3521261.
Article23. World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia;2000. p. 15–21.24. Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993; 25:71–80. PMID: 8292105.
Article25. Korea Health Industry Development Institute. Development of Nutrient Database. Cheongju: Korea Health Industry Development Institute;2000. p. 26–164.26. National Institute of Agricultural Sciences. Food Composition Table. 8th ed. Suwon: National Institute of Agricultural Sciences;2011.27. Yoon MO, Kim K, Hwang JY, Lee HS, Son TY, Moon HK, Shim JE. Development of a fatty acids database using the Korea National Health and Nutrition Examination Survey data. J Nutr Health. 2014; 47:435–442.
Article28. Korea Centers for Disease Control and Prevention. Guidebook for Data Users of the Sixth Korea National Health and Nutriton Examination Survey (KNHANES VI), 2013–2015. Cheongju: Korea Centers for Disease Control and Prevention;2015.29. National Fisheries Research & Development Institute (KR). Fatty Acid Composition of Fisheries Products in Korea. Busan: National Fisheries Research & Development Institute;2012. p. 2–123.30. Rural Development Administration. Fatty acid and cholesterol content of foods. Food Composition Table. 7th ed. Suwon: Rural Development Administration;2006. p. 277–380.31. United States Development of Agriculture, Agricultural Research Service. USDA national nutrient database for standard reference. release 25 [Internet]. Washington D.C.: United States Development of Agriculture;2012. cited 2013 August 19. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/methods-and-application-of-food-composition-laboratory/mafcl-site-pages/sr11-sr28.32. Ministry of Education, Culture, Sports, Science and Technology. The Council for Science and Technology, Subdivision on Resources. Standard Tables of Food Composition in Japan (Fifth Revised and Enlarged Edition). Tokyo: Ministry of Education, Culture, Sports, Science and Technology;2005.33. Korea Centers for Disease Control and Prevention. Korea National Health and Nutrition Survey VI-1 (2013) Health Examination Guidelines. Cheongju: Ministry of Health and Welfare of Korea;2014. p. 46–48.34. Willett W. Nutritional Epidemiology. 3rd ed. New York (NY): Oxford University Press, USA;2012. p. 274–275.35. Persons JE, Robinson JG, Ammann EM, Coryell WH, Espeland MA, Harris WS, Manson JE, Fiedorowicz JG. Omega-3 fatty acid biomarkers and subsequent depressive symptoms. Int J Geriatr Psychiatry. 2014; 29:747–757. PMID: 24338726.
Article36. Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine Care J. 2012; 3:9–12.
Article37. Carver JD, Benford VJ, Han B, Cantor AB. The relationship between age and the fatty acid composition of cerebral cortex and erythrocytes in human subjects. Brain Res Bull. 2001; 56:79–85. PMID: 11704343.
Article38. Logan AC. Neurobehavioral aspects of omega-3 fatty acids: possible mechanisms and therapeutic value in major depression. Altern Med Rev. 2003; 8:410–425. PMID: 14653768.39. Owen C, Rees AM, Parker G. The role of fatty acids in the development and treatment of mood disorders. Curr Opin Psychiatry. 2008; 21:19–24. PMID: 18281836.
Article40. Mizuno M, Yamada K, Olariu A, Nawa H, Nabeshima T. Involvement of brain-derived neurotrophic factor in spatial memory formation and maintenance in a radial arm maze test in rats. J Neurosci. 2000; 20:7116–7121. PMID: 10995859.
Article41. Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006; 59:1116–1127. PMID: 16631126.
Article42. Zunszain PA, Hepgul N, Pariante CM. Inflammation and depression. Curr Top Behav Neurosci. 2013; 14:135–151. PMID: 22553073.
Article43. Pfeilschifter J, Köditz R, Pfohl M, Schatz H. Changes in proinflammatory cytokine activity after menopause. Endocr Rev. 2002; 23:90–119. PMID: 11844745.
Article44. Saldeen P, Saldeen T. Women and omega-3 fatty acids. Obstet Gynecol Surv. 2004; 59:722–730. PMID: 15385858.
Article45. Lamers F, Milaneschi Y, Smit JH, Schoevers RA, Wittenberg G, Penninx BW. Longitudinal association between depression and inflammatory markers: results from the Netherlands study of depression and anxiety. Biol Psychiatry. 2019; 85:829–837. PMID: 30819515.
Article46. Chamani S, Bianconi V, Tasbandi A, Pirro M, Barreto GE, Jamialahmadi T, Sahebkar A. Resolution of Inflammation in neurodegenerative diseases: the role of resolvins. Mediators Inflamm. 2020; 2020:3267172. PMID: 32308554.
Article47. Bove M, Mhillaj E, Tucci P, Giardino I, Schiavone S, Morgese MG, Trabace L. Effects of n-3 PUFA enriched and n-3 PUFA deficient diets in naïve and Aβ-treated female rats. Biochem Pharmacol. 2018; 155:326–335. PMID: 30028991.
Article48. Turkmen S, Hernández-Cruz CM, Zamorano MJ, Fernández-Palacios H, Montero D, Afonso JM, Izquierdo M. Long-chain PUFA profiles in parental diets induce long-term effects on growth, fatty acid profiles, expression of fatty acid desaturase 2 and selected immune system-related genes in the offspring of gilthead seabream. Br J Nutr. 2019; 122:25–38. PMID: 31266551.
Article49. Horikawa C, Otsuka R, Kato Y, Nishita Y, Tange C, Rogi T, Kawashima H, Shibata H, Ando F, Shimokata H. Longitudinal association between n-3 long-chain polyunsaturated fatty acid intake and depressive symptoms: a population-based cohort study in Japan. Nutrients. 2018; 10:1655.50. Liao Y, Xie B, Zhang H, He Q, Guo L, Subramaniapillai M, Fan B, Lu C, Mclntyer RS. Efficacy of omega-3 PUFAs in depression: a meta-analysis. Transl Psychiatry. 2019; 9:190. PMID: 31383846.
Article51. Guu TW, Mischoulon D, Sarris J, Hibbeln J, McNamara RK, Hamazaki K, Freeman MP, Maes M, Matsuoka YJ, Belmaker RH, et al. A multi-national, multi-disciplinary Delphi consensus study on using omega-3 polyunsaturated fatty acids (n-3 PUFAs) for the treatment of major depressive disorder. J Affect Disord. 2020; 265:233–238. PMID: 32090746.
Article52. Bozzatello P, Rocca P, Mantelli E, Bellino S. Polyunsaturated fatty acids: what is their role in treatment of psychiatric disorders? Int J Mol Sci. 2019; 20:5257.
Article53. Wani AL, Bhat SA, Ara A. Omega-3 fatty acids and the treatment of depression: a review of scientific evidence. Integr Med Res. 2015; 4:132–141. PMID: 28664119.
Article54. Logan AC. Omega-3 fatty acids and major depression: a primer for the mental health professional. Lipids Health Dis. 2004; 3:25. PMID: 15535884.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dietary Intake of Nutrients and Food in Postmenopausal Korean Women
- Association between Omega Fatty Acid Intake and Suicidality : Sex Differences in the General Korean Population
- Omega-3 and Menopause
- Omega-3 Index as a Risk Factor for Cardiovascular Disease and Its Application to Korean Population
- Omega-3 and -6 Fatty Acid Intake and Colorectal Cancer Risk in Swedish Women’s Lifestyle and Health Cohort