Intest Res.
2021 Jul;19(3):313-322. 10.5217/ir.2020.00017.
Incidence and risk factors for venous thrombosis among patients with inflammatory bowel disease in China: a multicenter retrospective study
- Affiliations
-
- 1Inflammatory Bowel Disease Center, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 2Department of Internal Medicine, Peking Union Medical College Hospital, Beijing, China
- 3Department of Gastroenterology, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
- 4Department of Gastroenterology, Nanfang Hospital of Southern Medical University, Guangzhou, China
- 5Department of Gastroenterology, The First Affiliated Hospital of Anhui Medical University, Hefei, China
- 6Department of Gastroenterology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 7Department of Gastroenterology, Peking Union Medical College Hospital, Beijing, China
- KMID: 2518687
- DOI: http://doi.org/10.5217/ir.2020.00017
Abstract
- Background/Aims
Risk of venous thrombosis is increased in patients with inflammatory bowel disease (IBD); data on Asian IBD patients is limited and status quo of thrombosis screening and prophylaxis are unknown. Therefore, we aimed to investigate the incidence, screening, prophylaxis, and risk factors for venous thrombosis among Asian IBD patients.
Methods
Medical files of patients with Crohn’s disease (CD) and ulcerative colitis (UC) from 17 hospitals across China between 2011 and 2016 were reviewed for venous thrombosis, use of screening and prophylaxis. A case-control study was performed among hospitalized patients with venous thrombosis and their age-, sex-matched IBD controls hospitalized around the same period; disease characteristics and known provoking factors of venous thrombosis were recorded. Risk factors were analyzed in both univariate and logistic regression analyses.
Results
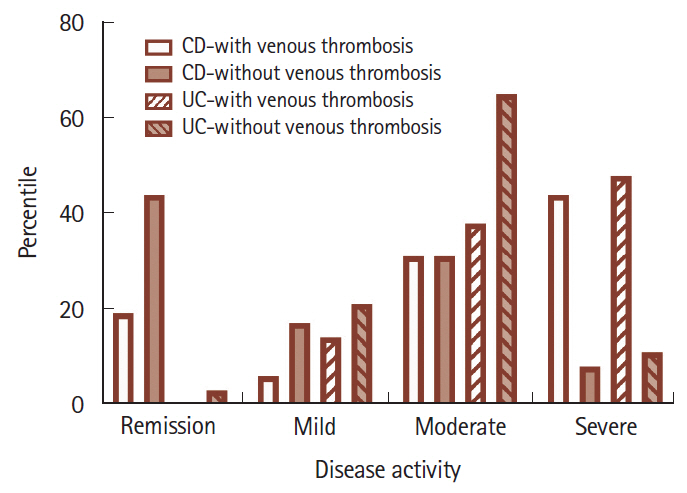
A total of 8,459 IBD patients were followed for 12,373 person-year. Forty-six patients (0.54%) had venous thrombosis, yielding an incidence of 37.18 per 10,000 person-year. Incidence increased with age, especially among CD. Less than 20% of patients received screening tests and 35 patients (0.41%) received prophylaxis. Severe disease flare was an independent risk factor for venous thrombosis (odds ratio [95% confidence interval]: CD, 9.342 [1.813– 48.137]; UC, 5.198 [1.268–21.305]); past use of steroids and extensive involvement were 2 additional risk factors in CD and UC, respectively.
Conclusions
Incidence of venous thrombosis in China was 37.18 per 10,000 person-year (0.54%). Use of screening and prophylaxis were rare. Severe disease flare was an independent risk factor for thrombosis among hospitalized patients.
Figure
Reference
-
1. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–663.
Article2. Nguyen GC, Bernstein CN, Bitton A, et al. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease: Canadian Association of Gastroenterology. Gastroenterology. 2014; 146:835–848.
Article3. Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001; 85:430–434.
Article4. Kappelman MD, Horvath-Puho E, Sandler RS, et al. Thromboembolic risk among Danish children and adults with inflammatory bowel diseases: a population-based nationwide study. Gut. 2011; 60:937–943.
Article5. Jess T, Gamborg M, Munkholm P, Sørensen TI. Overall and cause-specific mortality in ulcerative colitis: meta-analysis of population-based inception cohort studies. Am J Gastroentero. 2007; 102:609–617.
Article6. Andrade AR, Barros LL, Azevedo MF, et al. Risk of thrombosis and mortality in inflammatory bowel disease. Clin Transl Gastroenterol. 2018; 9:142.
Article7. Danese S, Papa A, Saibeni S, Repici A, Malesci A, Vecchi M. Inflammation and coagulation in inflammatory bowel disease: the clot thickens. Am J Gastroenterol. 2007; 102:174–186.
Article8. Raskob GE, Angchaisuksiri P, Blanco AN, et al. Thrombosis: a major contributor to global disease burden. Semin Thromb Hemost. 2014; 40:724–735.
Article9. Ng SC, Leung WK, Shi HY, et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territory-wide population-based registry in Hong Kong. Inflamm Bowel Dis. 2016; 22:1954–1960.10. Song HK, Lee KM, Jung SA, et al. Quality of care in inflammatory bowel disease in Asia: the results of a multinational webbased survey in the 2(nd) Asian Organization of Crohn’s and Colitis (AOCC) meeting in Seoul. Intest Res. 2016; 14:240–247.
Article11. Chung WS, Lin CL, Hsu WH, Kao CH. Inflammatory bowel disease increases the risks of deep vein thrombosis and pulmonary embolism in the hospitalized patients: a nationwide cohort study. Thromb Res. 2015; 135:492–496.
Article12. Weng MT, Park SH, Matsuoka K, et al. Incidence and risk factor analysis of thromboembolic events in East Asian patients with inflammatory bowel disease, a multinational collaborative study. Inflamm Bowel Dis. 2018; 24:1791–1800.
Article13. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19 Suppl A:5A–36A.
Article14. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629.
Article15. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976; 70:439–444.16. Miehsler W, Reinisch W, Valic E, et al. Is inflammatory bowel disease an independent and disease specific risk factor for thromboembolism? Gut. 2004; 53:542–548.
Article17. Lin H, Lim WC. Venous thromboembolism in Asian patients with inflammatory bowel disease. J Crohns Colitis. 2014; 8 Suppl 1:S311–S312.18. Weng MT, Tung CC, Wong JM, Wei SC. Should Asian inflammatory bowel disease patients need routine thromboprophylaxis? Intest Res. 2018; 16:312–314.
Article19. Lightner AL. Should surgical inflammatory bowel disease patients be given extended venous thromboembolic prophylaxis postoperatively? Inflamm Bowel Dis. 2020; 26:289–290.
Article20. Faye AS, Hung KW, Cheng K, et al. Minor hematochezia decreases use of venous thromboembolism prophylaxis in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2020; 26:1394–1400.
Article21. Ando K, Fujiya M, Nomura Y, et al. The incidence and risk factors of venous thromboembolism in Japanese inpatients with inflammatory bowel disease: a retrospective cohort study. Intest Res. 2018; 16:416–425.
Article22. Ando K, Fujiya M, Nomura Y, et al. The incidence and risk factors of venous thromboembolism in patients with inflammatory bowel disease: a prospective multicenter cohort study. Digestion. 2019; 100:229–237.
Article23. Kayal M, Radcliffe M, Plietz M, et al. Portomesenteric venous thrombosis in patients undergoing surgery for medically refractory ulcerative colitis. Inflamm Bowel Dis. 2020; 26:283–288.
Article24. Ohta Y, Arai M, Nakagawa T, et al. Comparison of a novel predictor of venous thromboembolic complications in inflammatory bowel disease with current predictors. J Gastroenterol Hepatol. 2019; 34:870–879.
Article25. Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e691S–e736S.26. Higgins PD, Skup M, Mulani PM, Lin J, Chao J. Increased risk of venous thromboembolic events with corticosteroid vs biologic therapy for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015; 13:316–321.
Article27. Koutroubakis IE. Therapy insight: vascular complications in patients with inflammatory bowel disease. Nat Clin Pract Gastroenterol Hepatol. 2005; 2:266–272.
Article28. Papay P, Miehsler W, Tilg H, et al. Clinical presentation of venous thromboembolism in inflammatory bowel disease. J Crohns Colitis. 2013; 7:723–729.
Article29. Scoville EA, Konijeti GG, Nguyen DD, Sauk J, Yajnik V, Ananthakrishnan AN. Venous thromboembolism in patients with inflammatory bowel diseases: a case-control study of risk factors. Inflamm Bowel Dis. 2014; 20:631–636.30. Zezos P, Kouklakis G, Saibil F. Inflammatory bowel disease and thromboembolism. World J Gastroenterol. 2014; 20:13863–13878.
Article31. Tichelaar YI, Kluin-Nelemans HJ, Meijer K. Infections and inflammatory diseases as risk factors for venous thrombosis: a systematic review. Thromb Haemost. 2012; 107:827–837.
Article32. Zöller B, Li X, Sundquist J, Sundquist K. Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden. Lancet. 2012; 379:244–249.
Article33. Wong T, Nightingale J, Winter M, Muller AF. Spontaneous venous thrombosis in inflammatory bowel disease: relevance of factor V Leiden and the prothrombin gene mutation. J Thromb Haemost. 2003; 1:1326–1328.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory bowel disease and superior mesenteric artery thromboembolism
- The incidence and risk factors of venous thromboembolism in Japanese inpatients with inflammatory bowel disease: a retrospective cohort study
- SMV Thrombosis on Taking Oral Contraceptive with Protein C and Protein S Deficiency
- Cerebral venous thrombosis in a patient with Crohn's disease
- Prevention and Treatment of Thromboembolism in Patients with Inflammatory Bowel Disease