Yeungnam Univ J Med.
2021 Jul;38(3):219-224. 10.12701/yujm.2020.00871.
Clinical effectiveness of omental transposition in facilitating perineal wound healing after abdominoperineal resection: a systematic review
- Affiliations
-
- 1Department of Surgery, Yeungnam University Hospital, Daegu, Korea
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2518663
- DOI: http://doi.org/10.12701/yujm.2020.00871
Abstract
- Background
Omental transposition has been used to facilitate perineal wound healing in patients undergoing abdominoperineal resection (APR). However, there is no high-level evidence supporting the effectiveness of omental transposition in this regard. This study aimed to investigate the clinical efficacy of omental transposition in facilitating perineal wound healing after APR.
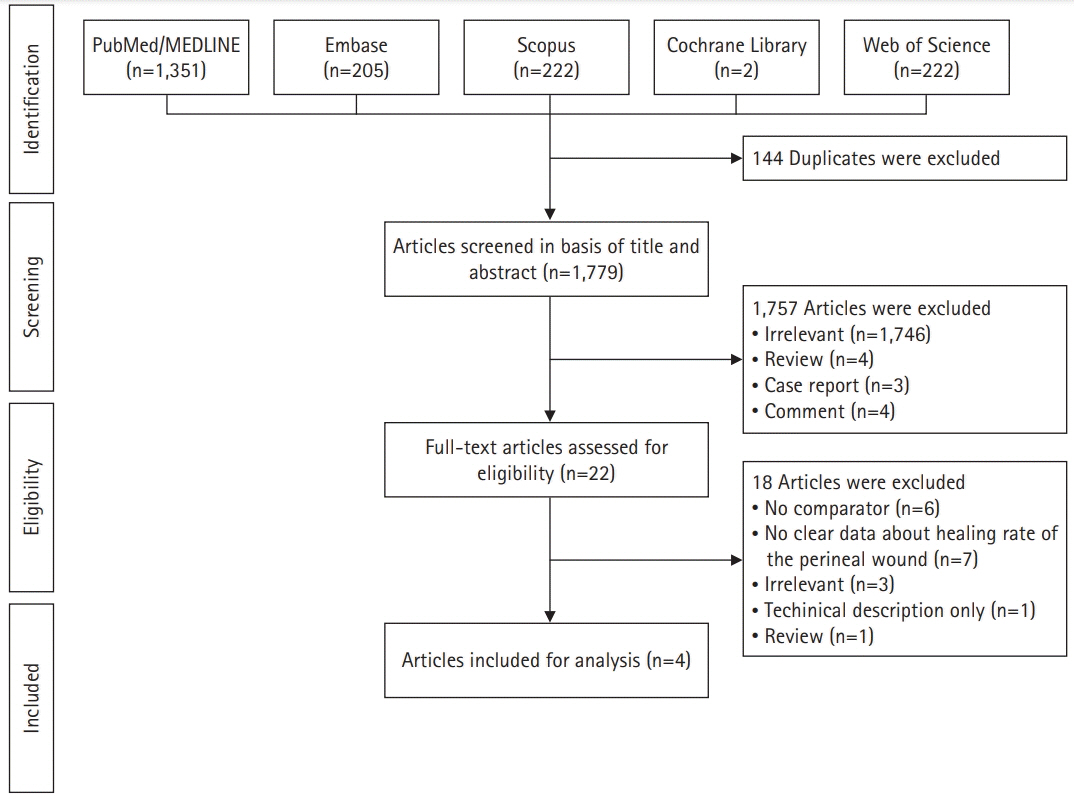
Methods
In this systematic review, we systematically searched the PubMed/MEDLINE, Embase, Scopus, Cochrane Library, and Web of Science databases for literature regarding the topic of our study. Studies published since the inception of each database were considered for review. The outcomes of interest were the perineal wound healing rate at 1 and 3 months postoperatively, perineal wound infection rate, and perineal wound healing period.
Results
Of the 1,923 studies identified, four articles representing 819 patients (omental transposition patients, n=295) were included in the final analysis. The wound healing rates at 1 and 3 months postoperatively in the omental transposition group (68.5% and 79.7%, respectively) did not significantly differ from those in the control group (57.4% and 78.7%, respectively) (p=0.759 and p=0.731, respectively). Perineal wound infection and chronic wound complication rates, including sinus, dehiscence, and fistula rates, also did not significantly differ between the omental transposition (8% and 7%, respectively) and control (11% and 7%, respectively) groups (p=0.221 and p=0.790, respectively).
Conclusion
Our results suggest that omental transposition does not affect perineal wound healing in patients who undergo APR.
Figure
Reference
-
References
1. Miles WE. A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon (1908). CA Cancer J Clin. 1971; 21:361–4.
Article2. Nilsson PJ. Omentoplasty in abdominoperineal resection: a review of the literature using a systematic approach. Dis Colon Rectum. 2006; 49:1354–61.
Article3. Mohammed S, Anaya DA, Awad SS, Albo D, Berger DH, Artinyan A. Sphincter preservation rates after radical resection for rectal cancer in the United States veteran population: opportunity for improvement in early disease. Ann Surg Oncol. 2015; 22:216–23.
Article4. Tompkins RG, Warshaw AL. Improved management of the perineal wound after proctectomy. Ann Surg. 1985; 202:760–5.5. Fingerhut A, Hay JM, Delalande JP, Paquet JC. Passive vs. closed suction drainage after perineal wound closure following abdominoperineal rectal excision for carcinoma. A multicenter, controlled trial. The French Association for Surgical Research. Dis Colon Rectum. 1995; 38:926–32.6. Artioukh DY, Smith RA, Gokul K. Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Colorectal Dis. 2007; 9:362–7.
Article7. Musters GD, Sloothaak DA, Roodbeen S, van Geloven AA, Bemelman WA, Tanis PJ. Perineal wound healing after abdominoperineal resection for rectal cancer: a two-centre experience in the era of intensified oncological treatment. Int J Colorectal Dis. 2014; 29:1151–7.
Article8. John H, Buchmann P. Improved perineal wound healing with the omental pedicle graft after rectal excision. Int J Colorectal Dis. 1991; 6:193–6.
Article9. Wiatrek RL, Thomas JS, Papaconstantinou HT. Perineal wound complications after abdominoperineal resection. Clin Colon Rectal Surg. 2008; 21:76–85.
Article10. El-Gazzaz G, Kiran RP, Lavery I. Wound complications in rectal cancer patients undergoing primary closure of the perineal wound after abdominoperineal resection. Dis Colon Rectum. 2009; 52:1962–6.
Article11. Nisar PJ, Scott HJ. Myocutaneous flap reconstruction of the pelvis after abdominoperineal excision. Colorectal Dis. 2009; 11:806–16.
Article12. Hultman CS, Sherrill MA, Halvorson EG, Lee CN, Boggess JF, Meyers MO, et al. Utility of the omentum in pelvic floor reconstruction following resection of anorectal malignancy: patient selection, technical caveats, and clinical outcomes. Ann Plast Surg. 2010; 64:559–62.13. de Bruin AF, Gosselink MP, Wijffels NA, Coene PP, van der Harst E. Local gentamicin reduces perineal wound infection after radiotherapy and abdominoperineal resection. Tech Coloproctol. 2008; 12:303–7.
Article14. Sumrien H, Newman P, Burt C, McCarthy K, Dixon A, Pullyblank A, et al. The use of a negative pressure wound management system in perineal wound closure after extralevator abdominoperineal excision (ELAPE) for low rectal cancer. Tech Coloproctol. 2016; 20:627–31.
Article15. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100.
Article16. Wang JY, Huang CJ, Hsieh JS, Huang YS, Juang YF, Huang TJ. Management of the perineal wounds following excision of the rectum for malignancy. Gaoxiong Yi Xue Ke Xue Za Zhi. 1994; 10:177–81.17. Hay JM, Fingerhut A, Paquet JC, Flamant Y. Management of the pelvic space with or without omentoplasty after abdominoperineal resection for carcinoma of the rectum: a prospective multicenter study. The French Association for Surgical Research. Eur J Surg. 1997; 163:199–206.18. Blok RD, Musters GD, Borstlap WA, Buskens CJ, Bemelman WA, Tanis PJ, et al. Snapshot study on the value of omentoplasty in abdominoperineal resection with primary perineal closure for rectal cancer. Ann Surg Oncol. 2018; 25:729–36.
Article19. Miles WE. Technique of the radical operation for cancer of the rectum. Br J Surg. 1914; 2:292–305.
Article20. Oates GD, Williams JA. Primary closure of the perineal wound in excision of the rectum. Proc R Soc Med. 1970; 63(Suppl 1):128.21. Broader JH, Masselink BA, Oates GD, Alexander-Williams J. Management of the pelvic space after proctectomy. Br J Surg. 1974; 61:94–7.
Article22. Ruckley CV, Smith AN, Balfour TW. Perineal closure by omental graft. Surg Gynecol Obstet. 1970; 131:300–2.23. Killeen S, Devaney A, Mannion M, Martin ST, Winter DC. Omental pedicle flaps following proctectomy: a systematic review. Colorectal Dis. 2013; 15:e634–45.
Article24. Collins D, Hogan AM, O’Shea D, Winter DC. The omentum: anatomical, metabolic, and surgical aspects. J Gastrointest Surg. 2009; 13:1138–46.
Article25. Moreaux J, Horiot A, Barrat F, Mabille J. Obliteration of the pelvic space with pedicled omentum after excision of the rectum for cancer. Am J Surg. 1984; 148:640–4.
Article26. Smith SR, Swift I, Gompertz H, Baker WN. Abdominoperineal and anterior resection of the rectum with retrocolic omentoplasty and no drainage. Br J Surg. 1988; 75:1012–5.
Article27. Marks CG, Leighton M, Ritchie JK, Hawley PR. Primary suture of the perineal wound following rectal excision for adenocarcinoma. Br J Surg. 1976; 63:322–6.
Article28. Dencker H, Norryd C, Tranberg KG. Management of the perineal wound after rectal excision. Acta Chir Scand. 1973; 139:568–70.29. Ferguson CM. Use of omental pedicle grafts in abdominoperineal resection. Am Surg. 1990; 56:310–2.30. Blok RD, Hagemans JA, Klaver CE, Hellinga J, van Etten B, Burger JW, et al. A systematic review and meta-analysis on omentoplasty for the management of abdominoperineal defects in patients treated for cancer. Ann Surg. 2020; 271:654–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mesh-Based Transperineal Repair of a Perineal Hernia After a Laparoscopic Abdominoperineal Resection
- Radiation Induced Perineo-Coccygeal Defect Coverage with Latissimus Dorsi Musculocutaneous Free Flap
- Omental Transposition Flap and Pectoralis Major Muscle Flap for Reconstruction of Wide Sternal Defect
- Effect of Arachnoid Dissection Upon Cerebral Vascularization in Omental Transposition to the Brain
- Clinical trial of Aromatherapy on Postpartum Mother's Perineal Healing