J Korean Med Sci.
2021 Jul;36(28):e204. 10.3346/jkms.2021.36.e204.
Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Medical Use of Military Hospitals in Korea
- Affiliations
-
- 1Department of Internal Medicine, Division of Infectious Diseases, Armed Forces Capital Hospital, Seongnam, Korea
- 2Clinical Medical Research Center, Armed Forces Capital Hospital, Seongnam, Korea
- 3Department of Rehabilitation Medicine, Armed Forces Capital Hospital, Seongnam, Korea
- 4Department of Internal Medicine, Division of Pulmonary and Critical Care Medicine, Armed Forces Capital Hospital, Seongnam, Korea
- 5Department of Ophthalmology, Armed Forces Capital Hospital, Seongnam, Korea
- 6Department of Internal Medicine, Division of Allergy and Clinical Immunology, Armed Forces Capital Hospital, Seongnam, Korea
- KMID: 2518526
- DOI: http://doi.org/10.3346/jkms.2021.36.e204
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic began in December 2019. While it has not yet ended, COVID-19 has already created transitions in health care, one of which is a decrease in medical use for health-related issues other than COVID-19 infection. Korean soldiers are relatively homogeneous in terms of age and physical condition. They show a similar disease distribution pattern every year and are directly affected by changes in government attempts to control COVID-19 with nonpharmaceutical interventions. This study aimed to identify the changes in patterns of outpatient visits and admissions to military hospitals for a range of disease types during a pandemic.
Methods
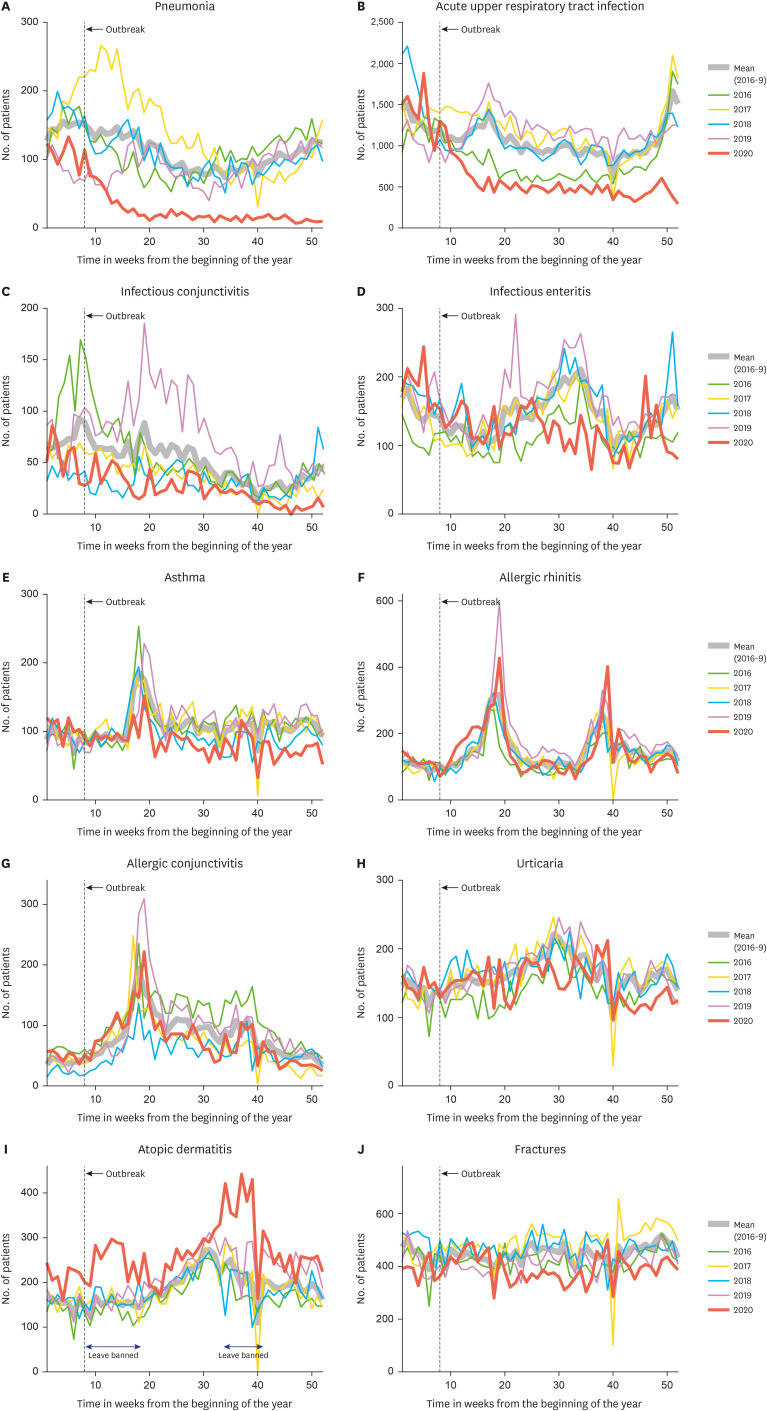
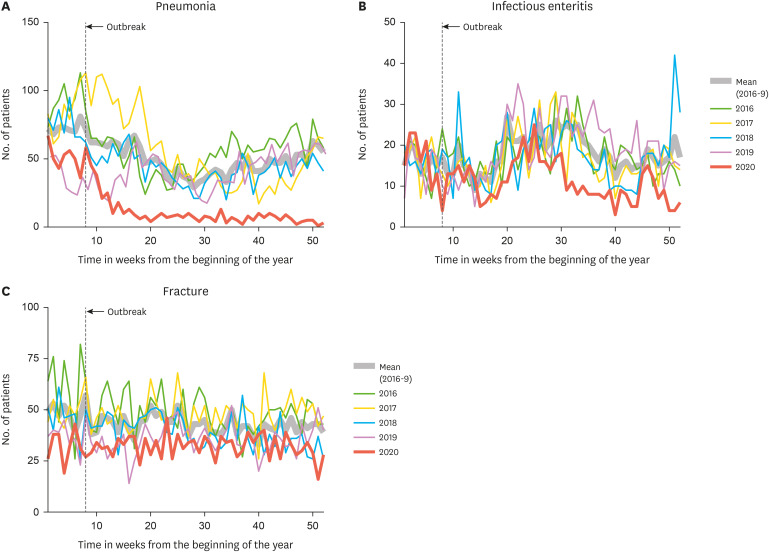
Outpatient attendance and admission data from all military hospitals in South Korea from January 2016 to December 2020 were analyzed. Only active enlisted soldiers aged 18–32 years were included. Outpatient visits where there was a diagnosis of pneumonia, acute upper respiratory tract infection, infectious conjunctivitis, infectious enteritis, asthma, allergic rhinitis, allergic conjunctivitis, atopic dermatitis, urticaria, and fractures were analyzed. Admissions for pneumonia, acute enteritis, and fractures were also analyzed. All outpatient visits and admissions in 2020 for each disease were counted on a weekly basis and compared with the average number of visits over the same period of each year from 2016 to 2019. The corrected value was calculated by dividing the ratio of total weekly number of outpatient visits or admissions to the corresponding medical department in 2020 to the average in 2016–2019.
Results
A total of 5,813,304 cases of outpatient care and 143,022 cases of admission were analyzed. For pneumonia, the observed and corrected numbers of outpatient visits and admissions in 2020 decreased significantly compared with the average of other years (P < 0.001). The results were similar for outpatient visits for acute upper respiratory tract infection and infectious conjunctivitis (P < 0.001), while the corrected number of outpatient visits for infectious enteritis showed a significant increase in 2020 (P = 0.005). The corrected number of outpatient visits for asthma in 2020 did not differ from the average of the previous 4 years but the number of visits for the other allergic diseases increased significantly (P < 0.001). For fractures, the observed and corrected numbers of outpatient visits and admissions in 2020 decreased significantly compared with the average of other years (P < 0.001).
Conclusion
During the COVID-19 pandemic, outpatient visits to military hospitals for respiratory and conjunctival infections and fractures decreased, whereas visits for allergic diseases did not change or increased only slightly. Admissions for pneumonia decreased significantly in 2020, while those for acute enteritis and fractures also decreased, but showed an increased proportion compared with previous years. These results are important because they illustrate the changing patterns in lifestyle as a result of public encouragement to adopt nonpharmaceutical interventions during the pandemic and their effect on medical needs for both infectious and noninfectious diseases in a select group.
Figure
Cited by 2 articles
-
The Comparison of Emergency Medical Service Responses to and Outcomes of Out-of-hospital Cardiac Arrest before and during the COVID-19 Pandemic in an Area of Korea
Daesung Lim, Song Yi Park, Byungho Choi, Sun Hyu Kim, Ji Ho Ryu, Yong Hwan Kim, Ae Jin Sung, Byung Kwan Bae, Han Byeol Kim
J Korean Med Sci. 2021;36(36):e255. doi: 10.3346/jkms.2021.36.e255.Trends in the Incidence and Etiology of Non-Traumatic Spinal Cord Injury in Korea: A Nationwide Population-Based Study From 2007 to 2020
Yoonjeong Choi, Ja-Ho Leigh, Jooeun Jeon, Goo Joo Lee, Hyung-Ik Shin, Moon Suk Bang
J Korean Med Sci. 2023;38(18):e158. doi: 10.3346/jkms.2023.38.e158.
Reference
-
1. Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020; 48(2):155–163. PMID: 32072569.
Article2. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2021. Accessed June 12, 2021. https://covid19.who.int/.3. Chu D, Chen RC, Ku CY, Chou P. The impact of SARS on hospital performance. BMC Health Serv Res. 2008; 8(1):228. PMID: 18990210.
Article4. Bennett D, Chiang CF, Malani A. Learning during a crisis: the SARS epidemic in Taiwan. J Dev Econ. 2015; 112:1–18. PMID: 32287877.
Article5. Lee H, Park JH. Changes in health care utilization during the MERS epidemic. Int J Infect Dis. 2018; 73:187.
Article6. Lee SY, Khang YH, Lim HK. Impact of the 2015 Middle East Respiratory Syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019; 60(8):796–803. PMID: 31347336.
Article7. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021; 174(1):129–131. PMID: 32776780.
Article8. Zhang YN, Chen Y, Wang Y, Li F, Pender M, Wang N, et al. Reduction in healthcare services during the COVID-19 pandemic in China. BMJ Glob Health. 2020; 5(11):e003421.
Article9. Baek S, Park K, Lee E, Park S, Lee S, Lee J, et al. Results of the national infectious disease surveillance, from January to April 2020. Public Health Wkly Rep. 2020; 13(21):1491–1502.10. Choi SY, Yoon CG. Urologic diseases in Korean military population: a 6-year epidemiological review of medical records. J Korean Med Sci. 2017; 32(1):135–142. PMID: 27914143.
Article11. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020; 35(5):e61. PMID: 32030925.
Article12. Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020; 96(1137):399–402. PMID: 32366457.
Article13. Oh HS, Woong S. Strict containment strategy and rigid social distancing successfully contained COVID-19 in the military in South Korea. Mil Med. 2020; 185(11-12):476–479.
Article14. Huh K, Kim YE, Ji W, Kim DW, Lee EJ, Kim JH, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax.
Article15. Heo JY, Lee JE, Kim HK, Choe KW. Acute lower respiratory tract infections in soldiers, South Korea, April 2011–March 2012. Emerg Infect Dis. 2014; 20(5):875–877. PMID: 24750820.
Article16. Yoo H, Gu SH, Jung J, Song DH, Yoon C, Hong DJ, et al. Febrile respiratory illness associated with human adenovirus type 55 in South Korea military, 2014–2016. Emerg Infect Dis. 2017; 23(6):1016–1020. PMID: 28518038.17. Huh K, Kim I, Jung J, Lee JE, Jhun BW, Gu SH, et al. Prolonged shedding of type 55 human adenovirus in immunocompetent adults with adenoviral respiratory infections. Eur J Clin Microbiol Infect Dis. 2019; 38(4):793–800. PMID: 30693422.
Article18. Asadi S, Cappa CD, Barreda S, Wexler AS, Bouvier NM, Ristenpart WD. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci Rep. 2020; 10(1):15665. PMID: 32973285.
Article19. Liang M, Gao L, Cheng C, Zhou Q, Uy JP, Heiner K, et al. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis. 2020; 36:101751. PMID: 32473312.
Article20. Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, et al. Decreased influenza activity during the COVID-19 pandemic-United States, Australia, Chile, and South Africa, 2020. Am J Transplant. 2020; 20(12):3681–3685. PMID: 33264506.
Article21. Korea Centers for Disease Control and Prevention. Disease surveillance statistics for week 52, 2020. Updated 2020. Accessed March 22, 2021. http://www.kdca.go.kr/board/board.es?mid=a30502000000&bid=0032.22. Cardemil CV, Parashar UD, Hall AJ. Norovirus infection in older adults: epidemiology, risk factors, and opportunities for prevention and control. Infect Dis Clin North Am. 2017; 31(4):839–870. PMID: 28911830.23. Bruggink LD, Garcia-Clapes A, Tran T, Druce JD, Thorley BR. Decreased incidence of enterovirus and norovirus infections during the COVID-19 pandemic, Victoria, Australia, 2020. Commun Dis Intell (2018). 2021; 45.
Article24. Eigner U, Verstraeten T, Weil J. Decrease in norovirus infections in Germany following COVID-19 containment measures. J Infect. 2021; 82(6):276–316.
Article