Endocrinol Metab.
2021 Jun;36(3):491-499. 10.3803/EnM.2021.1070.
Antithyroid Drug Treatment in Graves’ Disease
- Affiliations
-
- 1Division of Endocrinology & Metabolism, Department of Medicine, Thyroid Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2517638
- DOI: http://doi.org/10.3803/EnM.2021.1070
Abstract
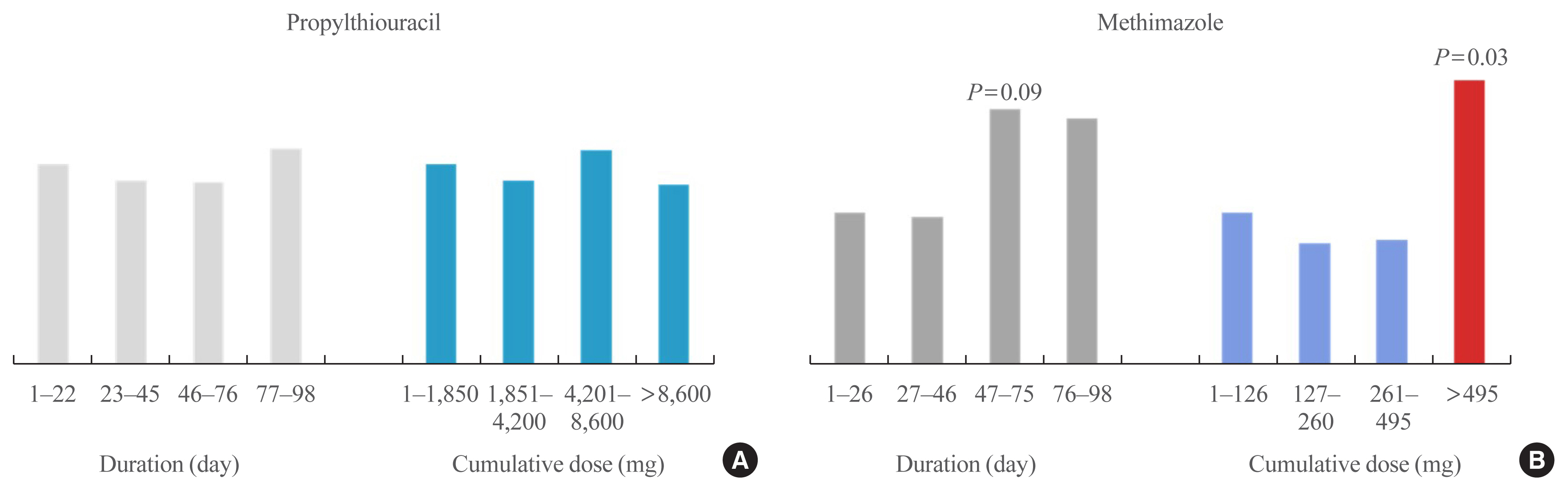
- Graves’ disease is associated with thyrotropin (TSH) receptor stimulating antibody, for which there is no therapeutic agent. This disease is currently treated through inhibition of thyroid hormone synthesis or destruction of the thyroid gland. Recurrence after antithyroid drug (ATD) treatment is common. Recent studies have shown that the longer is the duration of use of ATD, the higher is the remission rate. Considering the relationship between clinical outcomes and iodine intake, recurrence of Graves’ disease is more common in iodine-deficient areas than in iodine-sufficient areas. Iodine restriction in an iodine-excessive area does not improve the effectiveness of ATD or increase remission rates. Recently, Danish and Korean nationwide studies noted significantly higher prevalence of birth defects in newborns exposed to ATD during the first trimester compared to that of those who did not have such exposure. The prevalence of birth defects was lowest when propylthiouracil (PTU) was used and decreased by only 0.15% when methimazole was changed to PTU in the first trimester. Therefore, it is best not to use ATD in the first trimester or to change to PTU before pregnancy.
Figure
Cited by 2 articles
-
Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinol Metab. 2021;36(6):1277-1286. doi: 10.3803/EnM.2021.1251.Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinol Metab. 2022;37(2):323-332. doi: 10.3803/EnM.2022.1413.
Reference
-
1. Seo GH, Kim SW, Chung JH. Incidence & prevalence of hyperthyroidism and preference for therapeutic modalities in Korea. J Korean Thyroid Assoc. 2013; 6:56–63.
Article2. Smith TJ, Hegedus L. Graves’ disease. N Engl J Med. 2016; 375:1552–65.
Article3. Sundaresh V, Brito JP, Wang Z, Prokop LJ, Stan MN, Murad MH, et al. Comparative effectiveness of therapies for Graves’ hyperthyroidism: a systematic review and network meta-analysis. J Clin Endocrinol Metab. 2013; 98:3671–7.
Article4. Codaccioni JL, Orgiazzi J, Blanc P, Pugeat M, Roulier R, Carayon P. Lasting remissions in patients treated for Graves’ hyperthyroidism with propranolol alone: a pattern of spontaneous evolution of the disease. J Clin Endocrinol Metab. 1988; 67:656–62.
Article5. Nagai Y, Toya T, Fukuoka K, Tanaka N, Yanagi S, Kobayashi K. Occurrence and spontaneous remission of Graves’ hyperthyroidism preceded by painless thyroiditis. Endocr J. 1997; 44:881–5.
Article6. Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001; 344:501–9.
Article7. Abraham-Nordling M, Torring O, Hamberger B, Lundell G, Tallstedt L, Calissendorff J, et al. Graves’ disease: a long-term quality-of-life follow up of patients randomized to treatment with antithyroid drugs, radioiodine, or surgery. Thyroid. 2005; 15:1279–86.
Article8. Brandt F, Thvilum M, Almind D, Christensen K, Green A, Hegedus L, et al. Graves’ disease and toxic nodular goiter are both associated with increased mortality but differ with respect to the cause of death: a Danish population-based register study. Thyroid. 2013; 23:408–13.
Article9. Cramon P, Winther KH, Watt T, Bonnema SJ, Bjorner JB, Ekholm O, et al. Quality-of-life impairments persist six months after treatment of Graves’ hyperthyroidism and toxic nodular goiter: a prospective cohort study. Thyroid. 2016; 26:1010–8.
Article10. Giesecke P, Rosenqvist M, Frykman V, Friberg L, Wallin G, Hoijer J, et al. Increased cardiovascular mortality and morbidity in patients treated for toxic nodular goiter compared to Graves’ disease and nontoxic goiter. Thyroid. 2017; 27:878–85.
Article11. Sohn SY, Lee E, Lee MK, Lee JH. The association of overt and subclinical hyperthyroidism with the risk of cardiovascular events and cardiovascular mortality: meta-analysis and systematic review of cohort studies. Endocrinol Metab (Seoul). 2020; 35:786–800.
Article12. Kim HJ, Kang T, Kang MJ, Ahn HS, Sohn SY. Incidence and mortality of myocardial infarction and stroke in patients with hyperthyroidism: a nationwide cohort study in Korea. Thyroid. 2020; 30:955–65.
Article13. Burggraaf J, Lalezari S, Emeis JJ, Vischer UM, de Meyer PH, Pijl H, et al. Endothelial function in patients with hyperthyroidism before and after treatment with propranolol and thiamazol. Thyroid. 2001; 11:153–60.
Article14. Matsuura E, Atzeni F, Sarzi-Puttini P, Turiel M, Lopez LR, Nurmohamed MT. Is atherosclerosis an autoimmune disease? BMC Med. 2014; 12:47.
Article15. Bano A, Chaker L, de Maat MPM, Atiq F, Kavousi M, Franco OH, et al. Thyroid function and cardiovascular disease: the mediating role of coagulation factors. J Clin Endocrinol Metab. 2019; 104:3203–12.
Article16. Wartofsky L, Glinoer D, Solomon B, Nagataki S, Lagasse R, Nagayama Y, et al. Differences and similarities in the diagnosis and treatment of Graves’ disease in Europe, Japan, and the United States. Thyroid. 1991; 1:129–35.
Article17. Burch HB, Burman KD, Cooper DS. A 2011 survey of clinical practice patterns in the management of Graves’ disease. J Clin Endocrinol Metab. 2012; 97:4549–58.
Article18. Brito JP, Schilz S, Singh Ospina N, Rodriguez-Gutierrez R, Maraka S, Sangaralingham LR, et al. Antithyroid drugs: the most common treatment for Graves’ disease in the United States. A nationwide population-based study. Thyroid. 2016; 26:1144–5.
Article19. Cho BY, Koh CS. Current trends in the diagnosis and treatment of Graves’ disease in Korea. J Korean Soc Endocrinol. 1992; 7:216–27.20. Yi KH, Moon JH, Kim IJ, Bom HS, Lee J, Chung WY, et al. The diagnosis and management of hyperthyroidism consensus: report of the Korean Thyroid Association. J Korean Thyroid Assoc. 2013; 6:1–11.
Article21. Chung JH. Treatment of relapsed hyperthyroidism. J Korean Med Assoc. 2018; 61:248–52.
Article22. Kim YA, Cho SW, Choi HS, Moon S, Moon JH, Kim KW, et al. The second antithyroid drug treatment is effective in relapsed Graves’ disease patients: a median 11-year follow-up study. Thyroid. 2017; 27:491–6.
Article23. Cooper DS. Propylthiouracil levels in hyperthyroid patients unresponsive to large doses. Evidence of poor patient compliance. Ann Intern Med. 1985; 102:328–31.
Article24. Villagelin D, Romaldini JH, Santos RB, Milkos AB, Ward LS. Outcomes in relapsed Graves’ disease patients following radioiodine or prolonged low dose of methimazole treatment. Thyroid. 2015; 25:1282–90.
Article25. Vos XG, Endert E, Zwinderman AH, Tijssen JG, Wiersinga WM. Predicting the risk of recurrence before the start of antithyroid drug therapy in patients with Graves’ hyperthyroidism. J Clin Endocrinol Metab. 2016; 101:1381–9.
Article26. Giuliani C, Cerrone D, Harii N, Thornton M, Kohn LD, Dagia NM, et al. A TSHR-LH/CGR chimera that measures functional thyroid-stimulating autoantibodies (TSAb) can predict remission or recurrence in Graves’ patients undergoing antithyroid drug (ATD) treatment. J Clin Endocrinol Metab. 2012; 97:E1080–7.
Article27. Kwon H, Kim WG, Jang EK, Kim M, Park S, Jeon MJ, et al. Usefulness of measuring thyroid stimulating antibody at the time of antithyroid drug withdrawal for predicting relapse of Graves disease. Endocrinol Metab (Seoul). 2016; 31:300–10.
Article28. Weetman AP, McGregor AM, Hall R. Evidence for an effect of antithyroid drugs on the natural history of Graves’ disease. Clin Endocrinol (Oxf). 1984; 21:163–72.
Article29. Davies TF. Autoimmune thyroid disease genes come in many styles and colors. J Clin Endocrinol Metab. 1998; 83:3391–3.
Article30. Feldt-Rasmussen U, Schleusener H, Carayon P. Meta-analysis evaluation of the impact of thyrotropin receptor antibodies on long term remission after medical therapy of Graves’ disease. J Clin Endocrinol Metab. 1994; 78:98–102.
Article31. Laurberg P, Wallin G, Tallstedt L, Abraham-Nordling M, Lundell G, Torring O. TSH-receptor autoimmunity in Graves’ disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur J Endocrinol. 2008; 158:69–75.
Article32. Laurberg P, Krejbjerg A, Andersen SL. Relapse following antithyroid drug therapy for Graves’ hyperthyroidism. Curr Opin Endocrinol Diabetes Obes. 2014; 21:415–21.
Article33. Mohlin E, Filipsson Nystrom H, Eliasson M. Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000–2010. Eur J Endocrinol. 2014; 170:419–27.
Article34. Tamai H, Nakagawa T, Fukino O, Ohsako N, Shinzato R, Suematsu H, et al. Thionamide therapy in Graves’ disease: relation of relapse rate to duration of therapy. Ann Intern Med. 1980; 92:488–90.
Article35. Schleusener H, Schwander J, Fischer C, Holle R, Holl G, Badenhoop K, et al. Prospective multicentre study on the prediction of relapse after antithyroid drug treatment in patients with Graves’ disease. Acta Endocrinol (Copenh). 1989; 120:689–701.
Article36. Hedley AJ, Young RE, Jones SJ, Alexander WD, Bewsher PD. Antithyroid drugs in the treatment of hyperthyroidism of Graves’ disease: long-term follow-up of 434 patients. Scottish Automated Follow-Up Register Group. Clin Endocrinol (Oxf). 1989; 31:209–18.37. Garcia-Mayor RV, Paramo C, Luna Cano R, Perez Mendez LF, Galofre JC, Andrade A. Antithyroid drug and Graves’ hyperthyroidism. Significance of treatment duration and TRAb determination on lasting remission. J Endocrinol Invest. 1992; 15:815–20.
Article38. Klein I, Becker DV, Levey GS. Treatment of hyperthyroid disease. Ann Intern Med. 1994; 121:281–8.
Article39. Mazza E, Carlini M, Flecchia D, Blatto A, Zuccarini O, Gamba S, et al. Long-term follow-up of patients with hyperthyroidism due to Graves’ disease treated with methimazole. Comparison of usual treatment schedule with drug discontinuation vs continuous treatment with low methimazole doses: a retrospective study. J Endocrinol Invest. 2008; 31:866–72.
Article40. Abraham P, Avenell A, Park CM, Watson WA, Bevan JS. A systematic review of drug therapy for Graves’ hyperthyroidism. Eur J Endocrinol. 2005; 153:489–98.
Article41. Abraham P, Avenell A, McGeoch SC, Clark LF, Bevan JS. Antithyroid drug regimen for treating Graves’ hyperthyroidism. Cochrane Database Syst Rev. 2010; 2010:CD003420.
Article42. Azizi F, Malboosbaf R. Long-term antithyroid drug treatment: a systematic review and meta-analysis. Thyroid. 2017; 27:1223–31.
Article43. Azizi F, Amouzegar A, Tohidi M, Hedayati M, Khalili D, Cheraghi L, et al. Increased remission rates after long-term methimazole therapy in patients with Graves’ disease: results of a randomized clinical trial. Thyroid. 2019; 29:1192–200.
Article44. Konishi T, Okamoto Y, Ueda M, Fukuda Y, Harusato I, Tsukamoto Y, et al. Drug discontinuation after treatment with minimum maintenance dose of an antithyroid drug in Graves’ disease: a retrospective study on effects of treatment duration with minimum maintenance dose on lasting remission. Endocr J. 2011; 58:95–100.
Article45. Park SY, Kim BH, Kim M, Hong AR, Park J, Park H, et al. The longer the antithyroid drug is used, the lower the relapse rate in Graves’ disease: a retrospective multicenter cohort study in Korea. Endocrine. 2021. Apr. 15. [Epub]. https://doi.org/10.1007/s12020-021-02725-x .
Article46. Bandai S, Okamura K, Fujikawa M, Sato K, Ikenoue H, Kitazono T. The long-term follow-up of patients with thionamide-treated Graves’ hyperthyroidism. Endocr J. 2019; 66:535–45.
Article47. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1343–421.
Article48. Azizi F. Environmental iodine intake affects the response to methimazole in patients with diffuse toxic goiter. J Clin Endocrinol Metab. 1985; 61:374–7.
Article49. Solomon BL, Evaul JE, Burman KD, Wartofsky L. Remission rates with antithyroid drug therapy: continuing influence of iodine intake? Ann Intern Med. 1987; 107:510–2.
Article50. Roti E, Gardini E, Minelli R, Bianconi L, Salvi M, Gavaruzzi G, et al. Effects of chronic iodine administration on thyroid status in euthyroid subjects previously treated with antithyroid drugs for Graves’ hyperthyroidism. J Clin Endocrinol Metab. 1993; 76:928–32.
Article51. Pramyothin P, Leung AM, Pearce EN, Malabanan AO, Braverman LE. Clinical problem-solving. A hidden solution. N Engl J Med. 2011; 365:2123–7.52. Lumholtz IB, Poulsen DL, Siersbaek-Nielsen K, Friis T, Rogowski P, Kirkegaard C, et al. Outcome of long-term antithyroid treatment of Graves’ disease in relation to iodine intake. Acta Endocrinol (Copenh). 1977; 84:538–41.
Article53. Pedersen IB, Knudsen N, Carle A, Vejbjerg P, Jorgensen T, Perrild H, et al. A cautious iodization programme bringing iodine intake to a low recommended level is associated with an increase in the prevalence of thyroid autoantibodies in the population. Clin Endocrinol (Oxf). 2011; 75:120–6.
Article54. Huang H, Shi Y, Lin L, Li L, Lin X, Li X, et al. Inhibition of thyroid-restricted genes by follicular thyroglobulin involves iodinated degree. J Cell Biochem. 2011; 112:971–7.
Article55. Huang H, Chen L, Liang B, Cai H, Cai Q, Shi Y. Upregulation of TSHR, TTF-1, and PAX8 in nodular goiter is associated with iodine deficiency in the follicular lumen. Int J Endocrinol. 2016; 2016:2492450.
Article56. Huang H, Shi Y, Liang B, Cai H, Cai Q, Lin R. Optimal iodine supplementation during antithyroid drug therapy for Graves’ disease is associated with lower recurrence rates than iodine restriction. Clin Endocrinol (Oxf). 2018; 88:473–8.
Article57. Hiraiwa T, Ito M, Imagawa A, Takamatsu J, Kuma K, Miyauchi A, et al. Restriction of dietary iodine does not ameliorate the early effect of anti-thyroid drug therapy for Graves’ disease in an area of excessive iodine intake. J Endocrinol Invest. 2006; 29:380–4.
Article58. Park SM, Cho YY, Joung JY, Sohn SY, Kim SW, Chung JH. Excessive iodine intake does not increase the recurrence rate of Graves’ disease after withdrawal of the antithyroid drug in an iodine-replete area. Eur Thyroid J. 2015; 4:36–42.
Article59. Wing DA, Millar LK, Koonings PP, Montoro MN, Mestman JH. A comparison of propylthiouracil versus methimazole in the treatment of hyperthyroidism in pregnancy. Am J Obstet Gynecol. 1994; 170(1 Pt 1):90–5.
Article60. Mortimer RH, Cannell GR, Addison RS, Johnson LP, Roberts MS, Bernus I. Methimazole and propylthiouracil equally cross the perfused human term placental lobule. J Clin Endocrinol Metab. 1997; 82:3099–102.
Article61. Rivkees SA, Mattison DR. Ending propylthiouracil-induced liver failure in children. N Engl J Med. 2009; 360:1574–5.
Article62. Bahn RS, Burch HS, Cooper DS, Garber JR, Greenlee CM, Klein IL, et al. The role of propylthiouracil in the management of Graves’ disease in adults: report of a meeting jointly sponsored by the American Thyroid Association and the Food and Drug Administration. Thyroid. 2009; 19:673–4.
Article63. Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011; 21:593–646.
Article64. Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017; 27:315–89.
Article65. Andersen SL, Olsen J, Wu CS, Laurberg P. Birth defects after early pregnancy use of antithyroid drugs: a Danish nationwide study. J Clin Endocrinol Metab. 2013; 98:4373–81.
Article66. Andersen SL, Knosgaard L, Olsen J, Vestergaard P, Andersen S. Maternal thyroid function, use of antithyroid drugs in early pregnancy, and birth defects. J Clin Endocrinol Metab. 2019; 104:6040–8.
Article67. Seo GH, Kim TH, Chung JH. Antithyroid drugs and congenital malformations: a nationwide Korean cohort study. Ann Intern Med. 2018; 168:405–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Agranulocytosis due to secondary exposure to antithyroid drugs in a relapsed Graves' disease patient
- The treatment of Graves' disease in children and adolescents
- Medical Treatment of Graves' Disease
- Remission Predictors of Graves' Disease in Children
- Changes of Intercellular Adhesion Molecule-1 (ICAM-1) in Sera of Patients with Graves' Diease before and after Treatment with Antithyroid Drug