Korean J Women Health Nurs.
2021 Jun;27(2):141-152. 10.4069/kjwhn.2021.06.20.
Development and application of a couple-centered antenatal education program in Korea
- Affiliations
-
- 1College of Nursing, Yeoju Institute of Technology, Yeoju, Korea
- 2Department of Nursing, Woosong University, Daejeon, Korea
- 3College of Nursing, Chungnam National University, Daejeon, Korea
- KMID: 2517571
- DOI: http://doi.org/10.4069/kjwhn.2021.06.20
Abstract
- Purpose
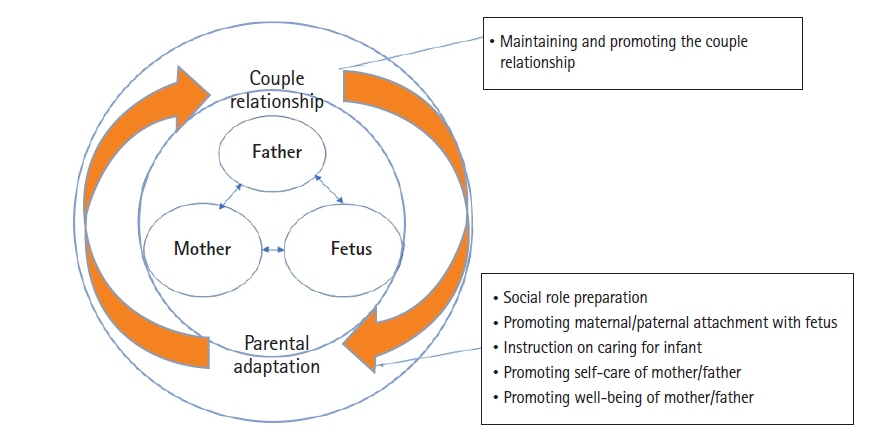
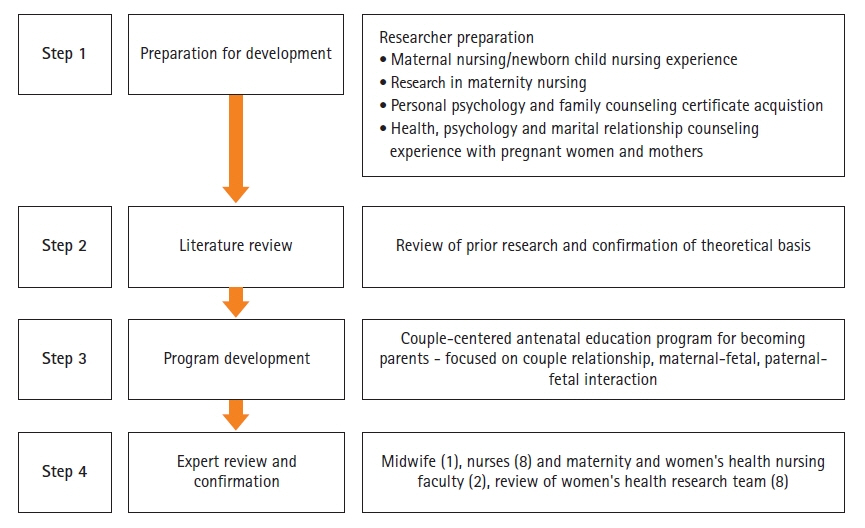
This study was conducted to develop a couple-centered antenatal education program and to test the program’s feasibility.
Methods
With a preliminary-experimental study design, 33 pregnant couples who were expecting their first child participated in this study. The program consisted of four sessions (1 hour/session/week) of education and counseling. Data were collected before and after the intervention from September 2018 to April 2019 at a women’s hospital in Daejeon, Korea, with demographic data forms, the Edinburgh Postnatal Depression Scale, Perceived Stress Scale, Maternal–Fetal Attachment Scale, Korean Newborn Care Confidence Scale, Wijma Delivery Expectancy/Experience Questionnaire, and Dyadic Adjustment Scale-10.
Results
The pregnant women and their husbands were on average 32.30±3.11 and 33.21±6.25 years old, respectively. The mean marriage duration was 2.34±1.63 years, the gestational age was 31.30±2.66 weeks, and 78.8% of the couples had a planned pregnancy. After the program, both the pregnant women and their husbands showed significant improvements in attachment to the fetus and confidence in providing infant care. Prenatal depression, prenatal stress, and fear of childbirth in pregnant women significantly decreased after completing the program. However, the dyadic adjustment score did not change significantly either in the pregnant women or their husbands.
Conclusion
A couple-centered antenatal education program seems to be effective for couples adjusting to parenthood, but further studies should explore ways to have a positive impact on couples’ relationships.
Keyword
Figure
Cited by 2 articles
-
Factors influencing prenatal and postpartum depression in Korea: a prospective cohort study
Hyeji Yoo, Sukhee Ahn, Seyeon Park, Jisoon Kim, Jiwon Oh, Minseon Koh
Korean J Women Health Nurs. 2021;27(4):326-336. doi: 10.4069/kjwhn.2021.11.17.An explanatory model of quality of life in high-risk pregnant women in Korea: a structural equation model
Mihyeon Park, Sukhee Ahn
Korean J Women Health Nurs. 2023;29(4):302-316. doi: 10.4069/kjwhn.2023.11.13.1.
Reference
-
References
1. Xuereb RB, Abela A, Spiteri G. Early parenting–portraits from the lives of first-time parents. J Reprod Infant Psychol. 2012; 30(5):468–482. https://doi.org/10.1080/02646838.2012.744961.
Article2. Molgora S, Fenaroli V, Prino LE, Rollè L, Sechi C, Trovato A, et al. Fear of childbirth in primiparous Italian pregnant women: the role of anxiety, depression, and couple adjustment. Women Birth. 2018; 31(2):117–123. https://doi.org/10.1016/j.wombi.2017.06.022.
Article3. Straub H, Adams M, Kim JJ, Silver RK. Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol. 2012; 207(4):329. e1-329.e3294. https://doi.org/10.1016/j.ajog.2012.06.033.
Article4. Emmanuel E, St John W. Maternal distress: a concept analysis. J Adv Nurs. 2010; 66(9):2104–15. https://doi.org/10.1111/j.1365-2648.2010.05371.x.
Article5. Baldwin S, Malone M, Sandall J, Bick D. Mental health and wellbeing during the transition to fatherhood: a systematic review of first time fathers’ experiences. JBI Database System Rev Implement Rep. 2018; 16(11):2118–2191. https://doi.org/10.11124/JBISRIR-2017-003773.
Article6. Alden KR, Lowdermilk DL, Cashion MC, Perry SE. Maternity and women’s health care. 12th ed. E-book: Elsevier Health Sciences; 2020.7. Darwin Z, Galdas P, Hinchliff S, Littlewood E, McMillan D, McGowan L, et al. Fathers’ views and experiences of their own mental health during pregnancy and the first postnatal year: a qualitative interview study of men participating in the UK Born and Bred in Yorkshire (BaBY) cohort. BMC Pregnancy Childbirth. 2017; 17(1):45. https://doi.org/10.1186/s12884-017-1229-4.
Article8. Brandão T, Brites R, Pires M, Hipólito J, Nunes O. Anxiety, depression, dyadic adjustment, and attachment to the fetus in pregnancy: actor-partner interdependence mediation analysis. J Fam Psychol. 2019; 33(3):294–303. https://doi.org/10.1037/fam0000513.
Article9. Habib C. The transition to fatherhood: a literature review exploring paternal involvement with identity theory. J Fam Stud. 2012; 18(2-3):103–120. https://doi.org/10.5172/jfs.2012.18.2-3.103.
Article10. Durtschi JA, Soloski KL, Kimmes J. The dyadic effects of supportive coparenting and parental stress on relationship quality across the transition to parenthood. J Marital Fam Ther. 2017; 43(2):308–321. https://doi.org/10.1111/jmft.12194.
Article11. Kaye DK, Kakaire O, Nakimuli A, Osinde MO, Mbalinda SN, Kakande N. Male involvement during pregnancy and childbirth: men’s perceptions, practices and experiences during the care for women who developed childbirth complications in Mulago Hospital, Uganda. BMC Pregnancy Childbirth. 2014; 14:54. https://doi.org/10.1186/1471-2393-14-54.
Article12. Ahldén I, Ahlehagen S, Dahlgren LO, Josefsson A. Parents’ expectations about participating in antenatal parenthood education classes. J Perinat Educ. 2012; 21(1):11–17. https://doi.org/10.1891/1058-1243.21.1.11.
Article13. Mercer RT. Becoming a mother versus maternal role attainment. J Nurs Scholarsh. 2004; 36(3):226–232. https://doi.org/10.1111/j.1547-5069.2004.04042.x.
Article14. Salmela AK. Personal goals and well-being during critical life transitions: the four C’s—channelling, choice, co-agency and compensation. Adv Life Course Res. 2009; 14(1-2):63–73. https://doi.org/10.1016/j.alcr.2009.03.003.
Article15. Donato S, Iafrate R, Barni D, Bertoni A, Bodenmann G, Gagliardi S. Measuring dyadic coping: the factorial structure of Bodenmann’s “Dyadic Coping Questionnaire” in an Italian sample. TPM Test Psychom Methodol Appl Psychol. 2009; 16(1):25–47.16. Pinquart M, Teubert D. A meta‐analytic study of couple interventions during the transition to parenthood. Fam Relat. 2010; 59(3):221–231. https://doi.org/10.1111/j.1741-3729.2010.00597.x.
Article17. Park S, Kim J, Oh J, Ahn S. Effects of psychoeducation on the mental health and relationships of pregnant couples: a systemic review and meta-analysis. Int J Nurs Stud. 2020; 104:103439. https://doi.org/10.1016/j.ijnurstu.2019.103439.
Article18. Kim SY, Kim HW. Prenatal nursing intervention studies published in Korean nursing journals: a scoping review. Korean J Women Health Nurs. 2020; 26(2):109–119. https://doi.org/10.4069/kjwhn.2020.06.12.
Article19. Delmore-Ko P, Pancer SM, Hunsberger B, Pratt M. Becoming a parent: the relation between prenatal expectations and postnatal experience. J Fam Psychol. 2000; 14(4):625–640. https://doi.org/10.1037//0893-3200.14.4.625.
Article20. Byrne J, Hauck Y, Fisher C, Bayes S, Schutze R. Effectiveness of a Mindfulness-Based Childbirth Education pilot study on maternal self-efficacy and fear of childbirth. J Midwifery Womens Health. 2014; 59(2):192–197. https://doi.org/10.1111/jmwh.12075.
Article21. Des Jarlais DC, Lyles C, Crepaz N; TREND Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004; 94(3):361–366. https://doi.org/10.2105/ajph.94.3.361.
Article22. Mercer RT, Walker LO. A review of nursing interventions to foster becoming a mother. J Obstet Gynecol Neonatal Nurs. 2006; 35(5):568–582. https://doi.org/10.1111/j.1552-6909.2006.00080.x.
Article23. Halford WK, Petch J. Couple psychoeducation for new parents: observed and potential effects on parenting. Clin Child Fam Psychol Rev. 2010; 13(2):164–180. https://doi.org/10.1007/s10567-010-0066-z.
Article24. Entsieh AA, Hallström IK. First-time parents’ prenatal needs for early parenthood preparation-a systematic review and meta-synthesis of qualitative literature. Midwifery. 2016; 39:1–11. https://doi.org/10.1016/j.midw.2016.04.006.
Article25. Delicate A, Ayers S, McMullen S. A systematic review and meta-synthesis of the impact of becoming parents on the couple relationship. Midwifery. 2018; 61:88–96. https://doi.org/10.1016/j.midw.2018.02.022.
Article26. Lunda P, Minnie CS, Benadé P. Women’s experiences of continuous support during childbirth: a meta-synthesis. BMC Pregnancy Childbirth. 2018; 18(1):167. https://doi.org/10.1186/s12884-018-1755-8.
Article27. de Moraes CJ, Granato TM. Becoming a father: an integrative literature on transition to parenthood. Psicologia em Estudo,. 2016; 21(4):557–567. https://doi.org/10.4025/psicolestud.v21i4.29871.
Article28. Xue WL, Shorey S, Wang W, He HG. Fathers’ involvement during pregnancy and childbirth: an integrative literature review. Midwifery. 2018; 62:135–145. https://doi.org/10.1016/j.midw.2018.04.013.
Article29. Petch J, Halford WK. Psycho-education to enhance couples’ transition to parenthood. Clin Psychol Rev. 2008; 28(7):1125–1137. https://doi.org/10.1016/j.cpr.2008.03.005.
Article30. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987; 150:782–786. https://doi.org/10.1192/bjp.150.6.782.
Article31. Kim YK, Hur JW, Kim KH, Oh KS, Shin YC. Clinical application of Korean version of Edinburgh postnatal depression scale. J Korean Neuropsychiatr Assoc. 2008; 47(1):36–44.32. Matthey S, Barnett B, Kavanagh DJ, Howie P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. J Affect Disord. 2001; 64(2-3):175–184. https://doi.org/10.1016/s0165-0327(00)00236-6.
Article33. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4):385–396. https://doi.org/10.2307/2136404.
Article34. Park J, Seo Y. Validation of the perceived stress scale (PSS) on samples of Korean university students. Korean J Psychol. 2010; 9(3):619–629.35. Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res. 1981; 30(5):281–284. https://doi.org/10.1097/00006199-198109000-00008.
Article36. Kim KY. Effects on maternal-infant attachment by the Taegyo prospective prenatal class [master’s thesis]. Seoul: Yonsei University;2000.37. Lee YW. A study of relationship between self-confidence in newborn care and postpartum depression of parturient women [master’s thesis]. Seoul: Yonsei University;1989.38. Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998; 19(2):84–97. https://doi.org/10.3109/01674829809048501.
Article39. Park SY, Ahn SH, Yoo HJ, Cho HJ, Kim SA. Validation of the Korean version of the Wijma delivery expectancy questionnaire (W-DEQ): version A. Poster session presented at: Sigma Theta Tau International, 30th International Nursing Research Congress; 2019 Jul 25-29; Calgary, Canada. Sigma Theta Tau International Honor Society of Nursing; 2019.40. Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976; 38(1):15–28. https://doi.org/10.2307/350547.
Article41. Cho H, Choi SM, Oh HJ, Kwon JH. Validity of the short forms of the Korean dyadic adjustment scale. Korean J Couns Psychother. 2011; 23(3):655–670.42. Bouchard G. The quality of the parenting alliance during the transition to parenthood. Canadian J Behav Sci. 2014; 46(1):20–28. https://doi.org/10.1037/a0031259.
Article43. Brady V, Lalor J. Space for human connection in antenatal education: uncovering women’s hopes using Participatory Action Research. Midwifery. 2017; 55:7–14. https://doi.org/10.1016/j.midw.2017.08.006.
Article44. Fontein-Kuipers YJ, Nieuwenhuijze MJ, Ausems M, Budé L, de Vries R. Antenatal interventions to reduce maternal distress: a systematic review and meta-analysis of randomised trials. BJOG. 2014; 121(4):389–397. https://doi.org/10.1111/1471-0528.12500.
Article45. Kang S, Kim G, Chung M. Changes in parenthood of pregnant couples participating in an education program for pregnant couples. J Child Lit Educ. 2017; 18(3):259–287. http://doi.org/10.22154/JCLE.18.3.12.
Article46. Svensson J, Barclay L, Cooke M. Randomised-controlled trial of two antenatal education programmes. Midwifery. 2009; 25(2):114–125. https://doi.org/10.1016/j.midw.2006.12.012.
Article47. Feinberg ME, Jones DE, Hostetler ML, Roettger ME, Paul IM, Ehrenthal DB. Couple-focused prevention at the transition to parenthood, a randomized trial: effects on coparenting, parenting, family violence, and parent and child adjustment. Prev Sci. 2016; 17(6):751–764. https://doi.org/10.1007/s11121-016-0674-z.
Article48. Serçekuş P, Başkale H. Effects of antenatal education on fear of childbirth, maternal self-efficacy and parental attachment. Midwifery. 2016; 34:166–172. https://doi.org/10.1016/j.midw.2015.11.016.
Article49. Halford WK, Bodenmann G. Effects of relationship education on maintenance of couple relationship satisfaction. Clin Psychol Rev. 2013; 33(4):512–525. https://doi.org/10.1016/j.cpr.2013.02.001.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Proposal for the Future of Medical Education Accreditation
- Development and Application of Sexual Health Education Program for Unmarried Mothers
- Effects of a Structure-centered Cooperative Learning Safety Education Program based on Blended Learning for Elementary School Students
- Development and Application of Web-based Nursing Informatics Education Program for Graduate Students
- Development and Application of an Education Program for Healthy Dietary Life for Elementary School Aftercare Class Children