Korean J Women Health Nurs.
2021 Jun;27(2):93-103. 10.4069/kjwhn.2021.05.06.
Factors affecting unmet healthcare needs of low-income overweight and obese women in Korea: analysis of the Korean National Health and Nutrition Examination Survey 2017
- Affiliations
-
- 1College of Nursing, Jeonbuk National University, Jeonju, Korea
- KMID: 2517567
- DOI: http://doi.org/10.4069/kjwhn.2021.05.06
Abstract
- Purpose
The purpose of this study was to explore unmet healthcare needs among low-income overweight and obese women and to identify the factors affecting unmet healthcare needs.
Methods
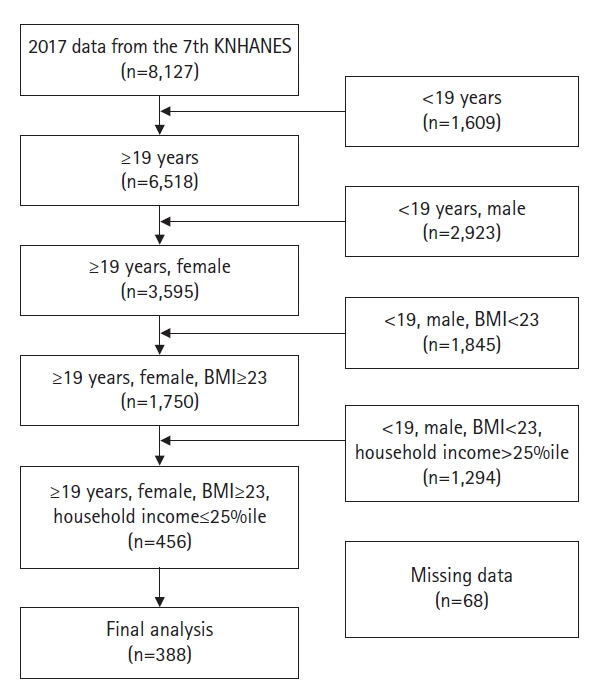
The study was a secondary analysis of data from the 2017 Korea National Health and Nutrition Examination Survey. A final sample of 388 out of 8,127 participants was analyzed using complex descriptive statistics, the chi-square test, the independent t-test, and logistic regression.
Results
The mean age of the participants was 66.51±1.05 years. Unmet healthcare needs were experienced by 19.4% of low-income overweight and obese women. Women with depression, stress, and poor self-reported health status were significantly more likely than their counterparts to experience unmet healthcare needs. Poor self-reported health status was confirmed to be related to unmet health needs in low-income overweight and obese women (odds ratio, 2.65; p=.011).
Conclusion
The study provides the novel insight that the unmet healthcare needs of low-income overweight and obese women were influenced by self-reported health status. Healthcare providers should make efforts to develop strategies to reduce unmet healthcare needs among low-income overweight and obese women, who constitute a vulnerable population.
Keyword
Figure
Cited by 1 articles
-
Health promoting behaviors in low-income overweight and obese women in Korea: an exploratory qualitative study
Ju-Hee Nho, Eun Jin Kim
Korean J Women Health Nurs. 2021;27(4):348-357. doi: 10.4069/kjwhn.2021.11.30.
Reference
-
References
1. Korea Disease Control and Prevention Agency. Korea Health Statistics 2019: Korea National Health and Nutrition Examination Survey (KNHANES Ⅷ-1) [Internet]. Cheongju: Author; 2020 [cited 2021 Jan 16]. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do.2. De Lorenzo A, Gratteri S, Gualtieri P, Cammarano A, Bertucci P, Di Renzo L. Why primary obesity is a disease? J Transl Med. 2019; 17(1):169. https://doi.org/10.1186/s12967-019-1919-y.
Article3. Kulie T, Slattengren A, Redmer J, Counts H, Eglash A, Schrager S. Obesity and women's health: an evidence-based review. J Am Board Fam Med. 2011; 24(1):75–85. https://doi.org/10.3122/jabfm.2011.01.100076.
Article4. Simon GE, Ludman EJ, Linde JA, Operskalski BH, Ichikawa L, Rohde P, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008; 30(1):32–39. https://doi.org/ 10.1016/j.genhosppsych.2007.09.001.
Article5. Pureza IR, Melo IS, Macena ML, Praxedes DR, Vasconcelos LG, Silva-Júnior AE, et al. Acute effects of time-restricted feeding in low-income women with obesity placed on hypoenergetic diets: randomized trial. Nutrition. 2020; 77:110796. https://doi.org/10.1016/j.nut.2020.110796.
Article6. An SJ, Park EJ, Cheon JH, Hwang HJ, Kim MJ. Prospective study for evaluating therapeutic efficacy of obese patients of low socioeconomic status in Korea. Korean J Health Promot. 2017; 17(2):54–63. https://doi.org/10.15384/kjhp.2017.17.2.54.
Article7. Lee HM, Jung HJ, Jung IK. Relationships among metabolically healthy status, physical activity, and sedentary behavior according to obesity in low-income menopause women. Asian J Physical Educ Sport Sci. 2020; 8(2):75–89. https://doi.org/10.16915/jkapesgw.2018.06.32.2.131.
Article8. Donabedian A. Aspects of medical care administration: specifying requirements for health care. Cambridge: Harvard University Press;1973. p. 65–68.9. Diamant AL, Hays RD, Morales LS, Ford W, Calmes D, Asch S, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. Am J Public Health. 2004; 94(5):783–789. https://doi.org/10.2105/ajph.94.5.783.
Article10. Kim TH. The challenges of social welfare education in the health and medical service sector: focusing on relationship between unmet health services needs and social isolation. Korean J Soc Welf Educ. 2014; 25:123–146.11. Lee HK, Kim MS, Choi SS, Choi MK. Eco-systematic analysis on the factors related to the Korean elderly suicide ideation. Health Soc Welfare Rev. 2014; 34:430–451. https://doi.org/10.15709/hswr.2014.34.3.430.
Article12. Heo J, Oh J, Kim J, Lee M, Lee JS, Kwon S, et al. Poverty in the midst of plenty: unmet needs and distribution of health care resources in South Korea. PLoS One. 2012; 7(11):e51004. https://doi.org/10.1371/journal.pone.0051004.
Article13. Chae HJ, Kim M. Unmet healthcare needs and related factors according to gender differences in single-person household. Korean J Women Health Nurs. 2020; 26(1):93–103. https://doi.org/10.4069/kjwhn.2020.03.23.
Article14. Reeves A, McKee M, Mackenbach J, Whitehead M, Stuckler D. Public pensions and unmet medical need among older people: cross-national analysis of 16 European countries, 2004-2010. J Epidemiol Community Health. 2017; 71(2):174–180. https://doi.org/10.1136/jech-2015-206257.
Article15. Karanikolos M, Gordeev VS, Mackenbach JP, McKee M. Access to care in the Baltic States: did crisis have an impact? Eur J Public Health. 2016; 26(2):236–241. https://doi.org/10.1093/eurpub/ckv205.
Article16. Kim Y, Kim S, Jeong S, Cho SG, Hwang SS. Poor people and poor health: examining the mediating effect of unmet healthcare needs in Korea. J Prev Med Public Health. 2019; 52(1):51–59. https://doi.org/10.3961/jpmph.18.162.
Article17. Hwang J. Understanding reasons for unmet health care needs in Korea: what are health policy implications? BMC Health Serv Res. 2018; 18(1):557. https://doi.org/10.1186/s12913-018-3369-2.
Article18. Kim SH, Lee CY. Analysis of factors affecting unmet healthcare needs of married immigrant women. J Korean Acad Nurs. 2013; 43(6):770–780. https://doi.org/10.4040/jkan.2013.43.6.770.
Article19. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995; 36(1):1–10.
Article20. Marshall EG. Do young adults have unmet healthcare needs? J Adolesc Health. 2011; 49(5):490–497. https://doi.org/10.1016/j.jadohealth.2011.03.005.
Article21. Regional Office for the Western Pacific, World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia;2000.22. U.S. Department of Health & Human Services; National Centers for Chronic Disease Prevention and Health Promotion. About Chronic diseases [Internet]. Atlanta: Author; 2021 [cited 2021 Apr 8]. Available from: https://www.cdc.gov/chronicdisease/about/index.htm#:~:text=Chronic%20diseases%20are%20defined%20broadly,disability%20in%20the%20United%20States.23. Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000; 34(6):1273–1302.24. Korea Disease Control and Prevention Agency. Chronic disease statistics [Internet]. Cheongju: Author; 2020 [cited 2021 Mar 10]. Available from: https://health.cdc.go.kr/healthinfo/biz/pblcVis/details.do?ctgrSn=54.25. Nho JH, Hwang ES. Effects of multidisciplinary lifestyle modification program on health-promoting behavior, psychological distress, body composition and reproductive symptoms among overweight and obese middle-aged women. Korean J Adult Nurs. 2019; 31(6):663–676. https://doi.org/10.7475/kjan.2019.31.6.663.
Article26. Kim SR, Nho JH, Kim JY, Hur J. Effects of a lifestyle intervention based on type D personality in overweight and obese middle-aged women: a feasibility study. Worldviews Evid Based Nurs. 2020; 17(5):393–403. https://doi.org/10.1111/wvn.12457.
Article27. Jeon JA. Korean Women’s mental health indicators. Health Welf Forum. 2016; 5:47–60.28. Statistics Korea. Subjective health status [Internet]. Daejeon: K-indicator; 2021 [cited 2021 Mar 11]. Available from: https://www.index.go.kr/unify/idx-info.do?idxCd=4235.29. Thammatacharee N, Tisayaticom K, Suphanchaimat R, Limwattananon S, Putthasri W, Netsaengtip R, et al. Prevalence and profiles of unmet healthcare need in Thailand. BMC Public Health. 2012; 12:923. https://doi.org/10.1186/1471-2458-12-923.
Article30. Ko H. Unmet healthcare needs and health status: panel evidence from Korea. Health Policy. 2016; 120(6):646–653. https://doi.org/10.1016/j.healthpol.2016.04.005.
Article31. Bryant T, Leaver C, Dunn J. Unmet healthcare need, gender, and health inequalities in Canada. Health Policy. 2009; 91(1):24–32. https://doi.org/10.1016/j.healthpol.2008.11.002.
Article32. Park EH, Park EC, Oh DH, Cho E. The effect of stress and depression on unmet medical needs. Korean J Clin Pharm. 2017; 27(1):44–54. https://doi.org/10.24304/kjcp.2017.27.1.44.
Article33. Stein J, Liegert P, Dorow M, König HH, Riedel-Heller SG. Unmet health care needs in old age and their association with depression - results of a population-representative survey. J Affect Disord. 2019; 245:998–1006. https://doi.org/10.1016/j.jad.2018.11.096.
Article34. Kim YR. A study on the factors related to unmet medical needs among some injury patient. J Digit Converg. 2019; 17(12):535–543. https://doi.org/10.14400/JDC.2019.17.12.535.
Article35. Gonda X, Pompili M, Serafini G, Carvalho AF, Rihmer Z, Dome P. The role of cognitive dysfunction in the symptoms and remission from depression. Ann Gen Psychiatry. 2015; 14:27. https://doi.org/10.1186/s12991-015-0068-9.
Article36. Lam RW, Kennedy SH, Mclntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. 2014; 59(12):649–654. https://doi.org/10.1177/070674371405901206.
Article37. Cummings SM, Cassie KM. Perceptions of biopsychosocial services needs among older adults with severe mental illness: met and unmet needs. Health Soc Work. 2008; 33(2):133–143. https://doi.org/10.1093/hsw/33.2.133.
Article38. Martino SC, Elliott MN, Kanouse DE, Farley DO, Burkhart Q, Hays RD. Depression and the health care experiences of Medicare beneficiaries. Health Serv Res. 2011; 46(6pt1):1883–1904. https://doi.org/10.1111/j.1475-6773.2011.01293.x.
Article39. Papageorgiou K, Vermeulen KM, Schroevers MJ, Stiggelbout AM, Buskens E, Krabbe PF, et al. Do individuals with and without depression value depression differently? And if so, why? Qual Life Res. 2015; 24(11):2565–75. https://doi.org/10.1007/s11136-015-1018-3.
Article40. Kim J. The impact of health care coverage on changes in self-rated health: comparison between the near poor and the upper middle class. Health Policy Manag. 2016; 26(4):390–398. https://doi.org/10.4332/KJHPA.2016.26.4.390.
Article41. Yoon YS, Jung B, Kim D, Ha IH. Factors underlying unmet medical needs: a cross-sectional study. Int J Environ Res Public Health. 2019; 16(13):2391. https://doi.org/10.3390/ijerph16132391.
Article42. Moon J, Kang M. The prevalence and predictors of unmet medical needs among the elderly living alone in Korea: an application of the behavioral model for vulnerable populations. Health Soc Welf Rev. 2016; 36(2):480–451. https://doi.org/10.15709/hswr.2016.36.2.480.
Article43. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997; 38(1):21–37. https://doi.org/10.2307/2955359.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unmet Healthcare Needs Status and Trend of Korea in 2017
- Factors Affecting Unmet Healthcare Needs among Adults with Chronic Diseases
- Unmet healthcare needs and related factors according to gender differences in single-person households
- Unmet Healthcare Needs Status and Trend of Korea in 2015
- Analysis of pregnant and breast-feeding women’s unmet healthcare needs