Korean Circ J.
2021 Jul;51(7):626-638. 10.4070/kcj.2020.0527.
Percutaneous Left Atrial Appendage Occlusion Yields Favorable Neurological Outcomes in Patients with Non-Valvular Atrial Fibrillation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine and Cardiovascular Center, Yongin Severance Hospital, Yongin, Korea
- 2Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Data Science Team (Biostatistician), Center for Digital Health, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 5Department of Cardiology, Cardiovascular Center, Korea University Anam Hospital, Seoul, Korea
- 6Department of Internal Medicine, Sejong General Hospital, Bucheon, Korea
- 7Division of Cardiology, Gachon University Gil Medical Center, Incheon, Korea
- 8Division of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 9Department of Neurology, Changwon Fatima Hospital, Changwon, Korea
- 10Department of Neurology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- 11Department of Neurology, Gangnam Severance Hospital, Severance Institute for Vascular and Metabolic Research, Yonsei University College of Medicine, Seoul, Korea
- 12Department of Neurology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 13Department of Neurology, Pusan National University Hospital, Pusan National University College of Medicine and Biomedical Research Institute, Busan, Korea
- 14Department of Medicine and Therapeutics, Prince of Wales Hospital, Hong Kong, China
- 15Department of Cardiology, Hospital Clinic of Barcelona, University of Barcelona, Catalonia, Spain
- 16Department of Cardiology, AHEPA University Hospital, Thessaloniki, Greece
- 17Department of Cardiology, Charite University Hospital Campus Benjamin Franklin, Berlin, Germany
- KMID: 2517492
- DOI: http://doi.org/10.4070/kcj.2020.0527
Abstract
- Background and Objectives
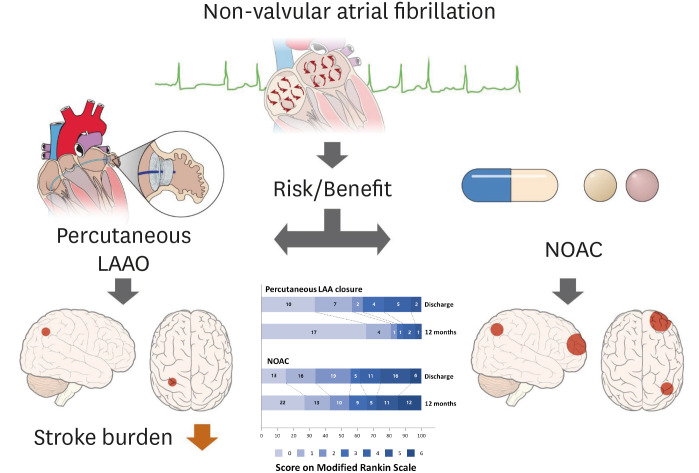
Prior studies have shown that stroke patients treated with percutaneous left atrial appendage occlusion (LAAO) for non-valvular atrial fibrillation (NVAF) experience better outcomes than similar patients treated with warfarin. We investigated the impact of percutaneous left atrial appendage closure on post-stroke neurological outcomes in NVAF patients, compared with non-vitamin K antagonist oral anticoagulant (NOAC) therapy.
Methods
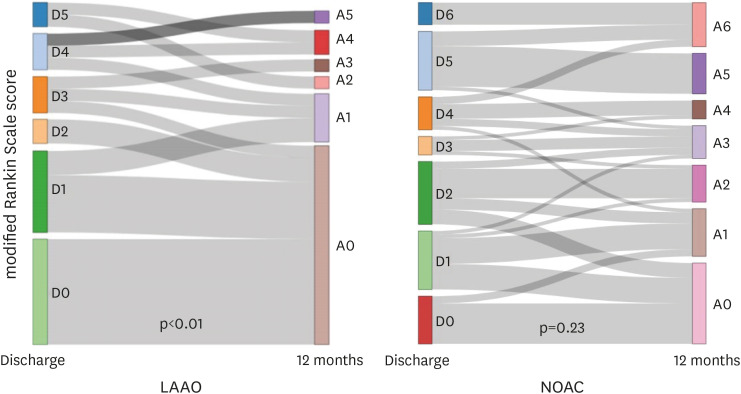
Medical records for 1,427 patients in multiple registries and for 1,792 consecutive patients at 6 Korean hospitals were reviewed with respect to LAAO or NOAC treatment. Stroke severity in patients who experienced ischemic stroke or transient ischemic attack after either treatment was assessed with modified Rankin Scale (mRS) scoring at hospital discharge and at 3 and 12 months post-stroke.
Results
mRS scores were significantly lower in LAAO patients at 3 (p<0.01) and 12 months (p<0.01) post-stroke, despite no significant differences in scores before the ischemic cerebrovascular event (p=0.22). The occurrences of disabling ischemic stroke in the LAAO and NOAC groups were 36.7% and 44.2% at discharge (p=0.47), 23.3% and 44.2% at 3 months post-stroke (p=0.04), and 13.3% and 43.0% at 12 months post-stroke (p=0.01), respectively. Recovery rates for disabling ischemic stroke at discharge to 12 months post-stroke were significantly higher for LAAO patients (50.0%) than for NOAC patients (5.6%) (p<0.01).
Conclusions
Percutaneous LAAO was associated with more favorable neurological outcomes after ischemic cerebrovascular event than NOAC treatment.
Figure
Cited by 1 articles
-
Is Left Atrial Appendage Occlusion Always Better than Direct Oral Anticoagulants?
Jun Kim
Korean Circ J. 2021;51(7):639-641. doi: 10.4070/kcj.2021.0194.
Reference
-
1. Lee H, Kim TH, Baek YS, et al. The trends of atrial fibrillation-related hospital visit and cost, treatment pattern and mortality in Korea: 10-year nationwide sample cohort data. Korean Circ J. 2017; 47:56–64. PMID: 28154592.
Article2. Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996; 61:755–759. PMID: 8572814.
Article3. Anderson DC, Kappelle LJ, Eliasziw M, Babikian VL, Pearce LA, Barnett HJ. Occurrence of hemispheric and retinal ischemia in atrial fibrillation compared with carotid stenosis. Stroke. 2002; 33:1963–1967. PMID: 12154246.
Article4. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021; 42:373–498. PMID: 32860505.5. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962. PMID: 24315724.
Article6. Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014; 64:1–12. PMID: 24998121.7. Freixa X, Llull L, Gafoor S, et al. Characterization of cerebrovascular events after left atrial appendage occlusion. Am J Cardiol. 2016; 118:1836–1841. PMID: 27745964.
Article8. Lee OH, Kim YD, Kim JS, et al. Favorable neurological outcome after ischemic cerebrovascular events in patients treated with percutaneous left atrial appendage occlusion compared with warfarin. Catheter Cardiovasc Interv. 2019; 94:E23–9. PMID: 30280479.
Article9. Reddy VY, Sievert H, Halperin J, et al. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation: a randomized clinical trial. JAMA. 2014; 312:1988–1998. PMID: 25399274.10. Meier B, Blaauw Y, Khattab AA, et al. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion. EuroIntervention. 2015; 10:1109–1125. PMID: 25169595.
Article11. Tzikas A, Shakir S, Gafoor S, et al. Left atrial appendage occlusion for stroke prevention in atrial fibrillation: multicentre experience with the AMPLATZER cardiac plug. EuroIntervention. 2016; 11:1170–1179. PMID: 25604089.
Article12. Tzikas A, Holmes DR Jr, Gafoor S, et al. Percutaneous left atrial appendage occlusion: the Munich consensus document on definitions, endpoints, and data collection requirements for clinical studies. Europace. 2017; 19:4–15. PMID: 27540038.
Article13. de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of Rankin ‘handicap’ grades after stroke. Stroke. 1995; 26:2027–2030. PMID: 7482643.
Article14. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015; 34:3661–3679. PMID: 26238958.
Article15. Holmes DR, Reddy VY, Turi ZG, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009; 374:534–542. PMID: 19683639.
Article16. Coisne A, Pilato R, Brigadeau F, et al. Percutaneous left atrial appendage closure improves left atrial mechanical function through Frank-Starling mechanism. Heart Rhythm. 2017; 14:710–716. PMID: 28188931.
Article17. Gupta S, Matulevicius SA, Ayers CR, et al. Left atrial structure and function and clinical outcomes in the general population. Eur Heart J. 2013; 34:278–285. PMID: 22782941.
Article18. Kawabata M, Goya M, Sasaki T, et al. Left atrial appendage thrombi formation in Japanese non-valvular atrial fibrillation patients during anticoagulation therapy - warfarin vs. direct oral anticoagulants. Circ J. 2017; 81:645–651. PMID: 28179613.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Electrical Cardioversion for Atrial Fibrillation on Left Atrial Appendage Function: A Transesophageal Echocardiography Study
- Cardioembolic Stroke in Atrial Fibrillation-Rationale for Preventive Closure of the Left Atrial Appendage
- Persistent Atrial Fibrillation Related to a Congenital Pericardial Defect and Left Atrial Appendage Herniation
- Simultaneous Closure of a Left Atrial Appendage through an Atrial Septal Defect and the Atrial Septal Defect
- Underdevelopment of Left Atrial Appendage