J Cerebrovasc Endovasc Neurosurg.
2021 Jun;23(2):152-158. 10.7461/jcen.2021.E2020.12.002.
Middle meningeal artery embolization for postoperative supratentorial chronic subdural hematoma occurring after posterior fossa neurosurgery
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2517029
- DOI: http://doi.org/10.7461/jcen.2021.E2020.12.002
Abstract
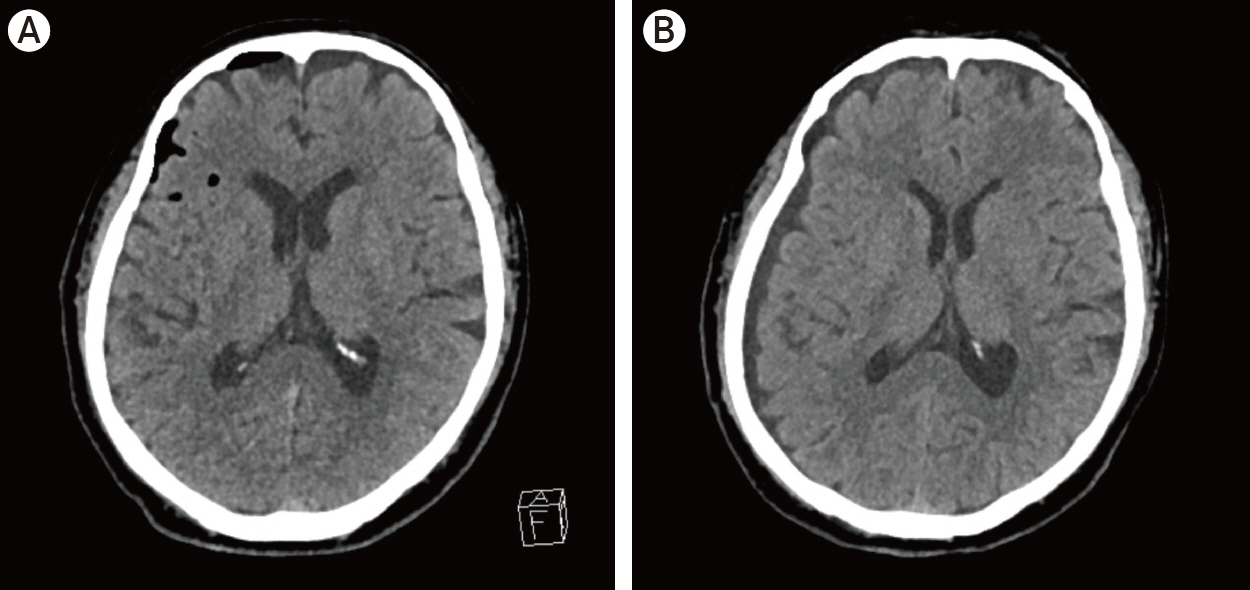
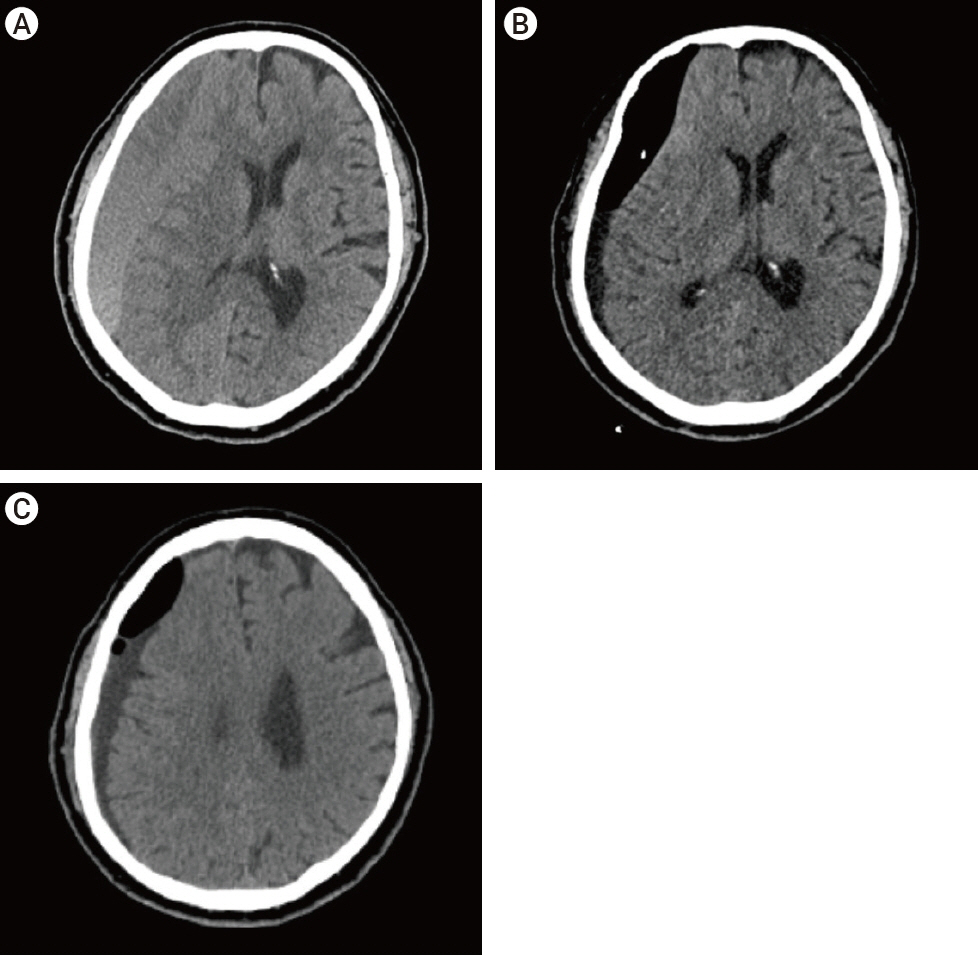
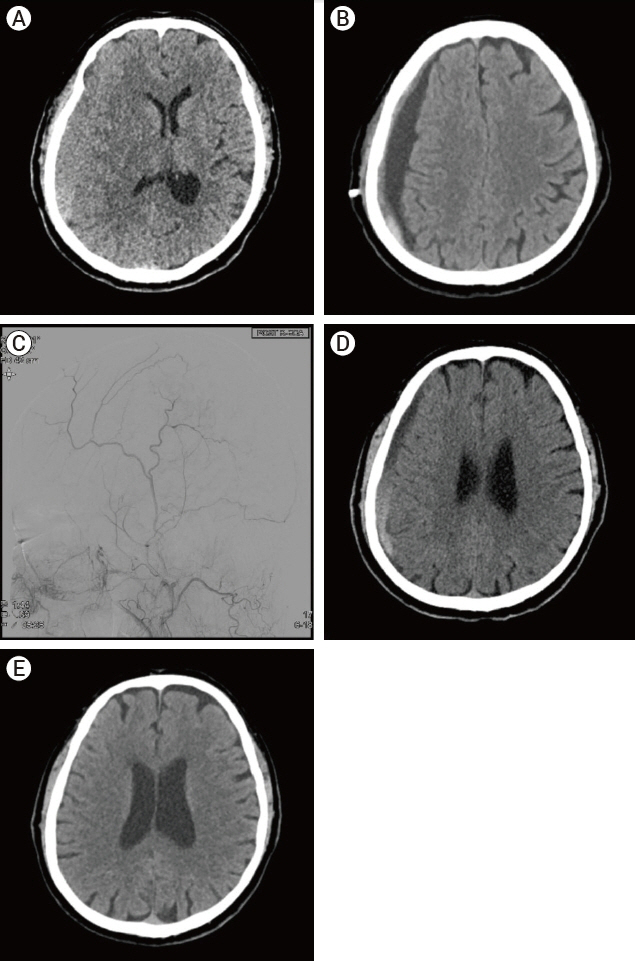
- Chronic subdural hematoma (CSDH) after posterior fossa surgery is rare but may occur. A 70-year-old man with trigeminal neuralgia underwent microvascular decompression. The patient took several medications for trigeminal neuralgia and tremor for a long time. The patient tended to bleed easily and did not stop well, but the bleeding was thoroughly controlled intraoperatively. A month later, he presented with left side weakness, and brain computed tomography showed huge amount of CSDH in the right cerebral convex with midline shifting. Although CSDH was completely drained via burr hole trephination, the brain was not fully expanded, and the CSDH recurred a month later. CSDH was evacuated, but there was still considerable subdural space and remained small CSDH in another superficial subdural space. We considered that the patient was at high risk of recurrence of CSDH and performed middle meningeal artery (MMA) embolization. Afterward, he did not suffer a recurrence. Here, we reviewed the risk factors of CSDH recurrence and the usefulness of MMA embolization in the treatment of CSDH, and we recommend upfront MMA embolization as an effective adjuvant to treat CSDH in patients at a high risk of recurrence of CSDH.
Figure
Reference
-
1. Amagasaki K, Takusagawa Y, Kanehashi K, Abe S, Watanabe S, Shono N, et al. Supratentorial acute subdural haematoma during microvascular decompression surgery: report of three cases. J Surg Case Rep. 2017; Feb. 2017(2):rjx004.
Article2. Anfossi G, Trovati M, Mularoni E, Massucco P, Calcamuggi G, Emanuelli G. Influence of propranolol on platelet aggregation and thromboxane B2 production from platelet-rich plasma and whole blood. Prostaglandins Leukot Essent Fatty Acids. 1989; Apr. 36(1):1–7.
Article3. Baglo T, Pouplard C, Valentin JB, Guery EA, Gruel Y, Vayne C. Acquired platelet defect associated with gabapentin treatment: a case-report. Platelets. 2020; Aug. 1-4.
Article4. Ban SP, Hwang G, Byoun HS, Kim T, Lee SU, Bang JS, et al. Middle meningeal artery embolization for chronic subdural hematoma. Radiology. 2018; Mar. 286(3):992–9.
Article5. Chon KH, Lee JM, Koh EJ, Choi HY. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir (Wien). 2012; Sep. 154(9):1541–8.
Article6. Fukuhara T, Gotoh M, Asari S, Ohmoto T, Akioka T. The relationship between brain surface elastance and brain reexpansion after evacuation of chronic subdural hematoma. Surg Neurol. 1996; Jun. 45(6):570–4.
Article7. Haldrup M, Ketharanathan B, Debrabant B, Schwartz OS, Mikkelsen R, Fugleholm K, et al. Embolization of the middle meningeal artery in patients with chronic subdural hematoma-a systematic review and meta-analysis. Acta Neurochir (Wien). 2020; Apr. 162(4):777–84.
Article8. Hanakita J, Kondo A. Serious complications of microvascular decompression operations for trigeminal neuralgia and hemifacial spasm. Neurosurgery. 1988; Feb. 22(2):348–52.
Article9. Hashimoto T, Ohashi T, Watanabe D, Koyama S, Namatame H, Izawa H, et al. Usefulness of embolization of the middle meningeal artery for refractory chronic subdural hematomas. Surg Neurol Int. 2013; Aug. 4:104.
Article10. Jackson SP. The growing complexity of platelet aggregation. Blood. 2007; Jun. 109(12):5087–95.
Article11. Jung YG, Jung NY, Kim E. Independent predictors for recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2015; Apr. 57(4):266–70.
Article12. Kasuya H, Kuroi Y, Yokosako S, Koseki H, Tani S. Intraoperative and postoperative bleeding in microvascular decompression for trigeminal neuralgia. World Neurosurg. 2018; Oct. 118:e123–8.
Article13. Ko BS, Lee JK, Seo BR, Moon SJ, Kim JH, Kim SH. Clinical analysis of risk factors related to recurrent chronic subdural hematoma. J Korean Neurosurg Soc. 2008; Jan. 43(1):11–5.
Article14. Lee MH, Jee TK, Lee JA, Park K. Postoperative complications of microvascular decompression for hemifacial spasm: lessons from experience of 2040 cases. Neurosurg Rev. 2016; Jan. 39(1):151–8. discussion 158.
Article15. Li N, Zhao W, Pu C, Shen J. Delayed hemorrhage following microvascular decompression. Three case reports. Neurol Med Chir (Tokyo). 2007; Apr. 47(4):186–8.16. Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001; Aug. 41(8):371–81.
Article17. Nagahori T, Nishijima M, Takaku A. Histological study of the outer membrane of chronic subdural hematoma: possible mechanism for expansion of hematoma cavity. No Shinkei Geka. 1993; Aug. 21(8):697–701.18. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001; Aug. 95(2):256–62.
Article19. Nakaguchi H, Tanishima T, Yoshimasu N. Relationship between drainage catheter location and postoperative recurrence of chronic subdural hematoma after burr-hole irrigation and closed-system drainage. J Neurosurg. 2000; Nov. 93(5):791–5.
Article20. Schwarz F, Loos F, Dunisch P, Sakr Y, Safatli DA, Kalff R, et al. Risk factors for reoperation after initial burr hole trephination in chronic subdural hematomas. Clin Neurol Neurosurg. 2015; Nov. 138:66–71.
Article21. Takahashi Y, Ohkura A, Sugita Y, Sugita S, Miyagi J, Shigemori M. Postoperative chronic subdural hematoma following craniotomy--four case reports. Neurol Med Chir (Tokyo). 1995; Feb. 35(2):78–81.22. Tanaka T, Kaimori M. Histological study of vascular structure between the dura mater and the outer membrane in chronic subdural hematoma in an adult. No Shinkei Geka. 1999; May. 27(5):431–6.23. Yakufujian M, Higuchi Y, Wakita S, Horiguchi , Ikegami S, Iwadate Y. Welling-up of cerebrospinal fluid is a sign of remote supratentorial hemorrhage during microvascular decompression: a case report. Egypt J Neurosurg. 2020; Apr. 35(11):1–4.
Article24. Yang AI, Balser DS, Mikheev A, Offen S, Huang JH, Babb J, et al. Cerebral atrophy is associated with development of chronic subdural haematoma. Brain Inj. 2012; 26(13-14):1731–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Middle Meningeal Embolization to Prevent Recurrent Spontaneous Chronic Subdural Hemorrhage
- Two Cases of Arachnoid Cyst of the Middle Cranial Fossa with Chronic Subdural Hematoma
- Cerebellar Hemorrhage after Burr Hole Drainage of Supratentorial Chronic Subdural Hematoma
- Helical coils augment embolization of the middle meningeal artery for treatment of chronic subdural hematoma: A technical note
- Middle Meningeal Artery Embolization in Recurrent Chronic Subdural Hematoma Combined with Arachnoid Cyst