Blood Res.
2021 Jun;56(2):61-64. 10.5045/br.2021.2021011.
Association of hypercoagulation with severe acute respiratory syndrome coronavirus 2 infection
- Affiliations
-
- 1Sri Ramachandra Medical College and Research Institute, Chennai, India
- 2MVJ Medical College and Research Hospital, Hoskote, India
- 3Sathyabama Institute of Science and Technology, Chennai, India
- 4Department of Zoology, Guru Ghasidas Vishwavidyalaya, Bilaspur, India
- KMID: 2517001
- DOI: http://doi.org/10.5045/br.2021.2021011
Abstract
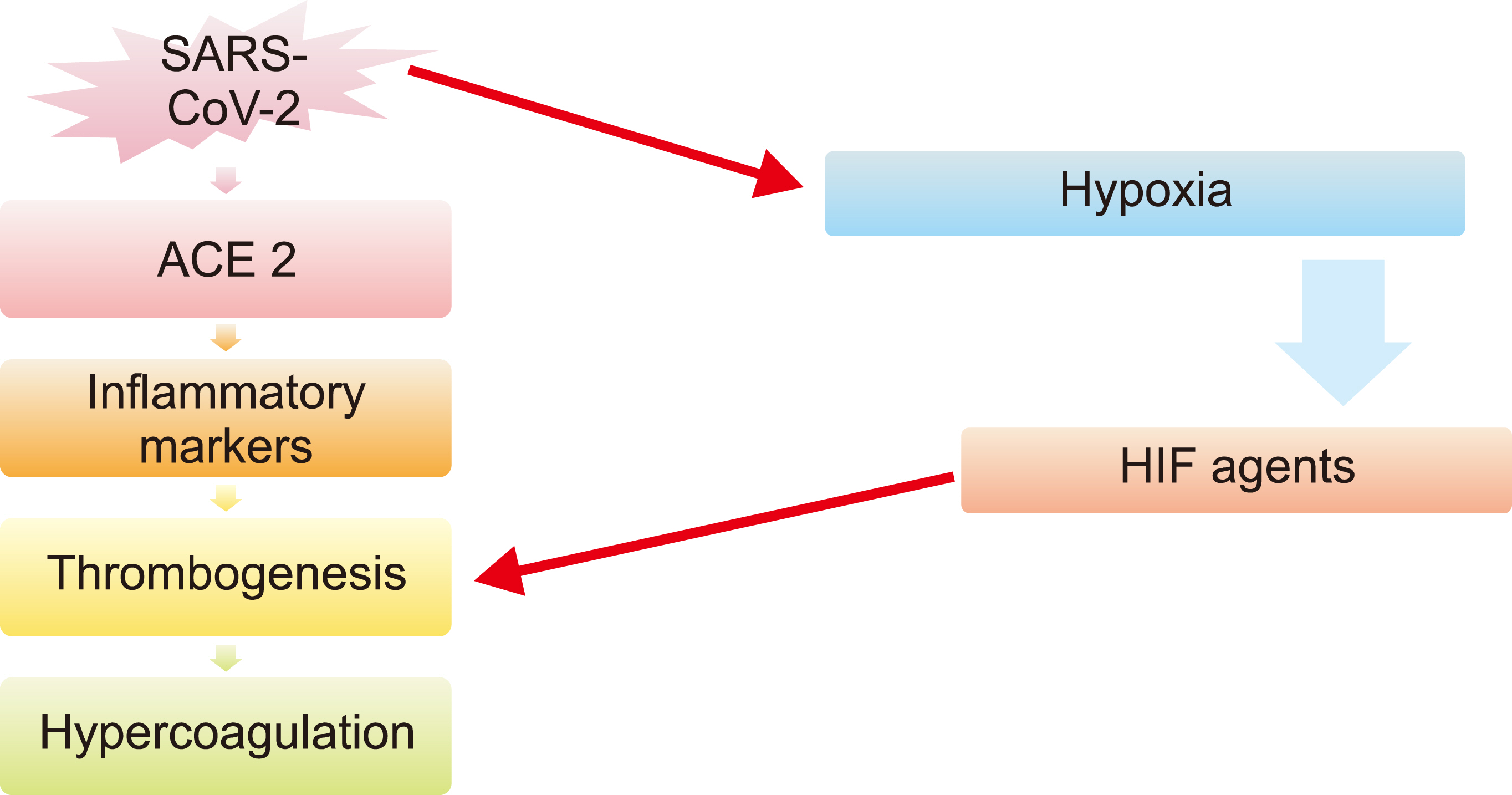
- The coronavirus disease 2019 (COVID-19) pandemic has emerged as a major threat to all healthcare systems across the globe, and it was declared a public health emergency of international concern by the World Health Organization (WHO). The novel coronavirus affects the respiratory system, producing symptoms such as fever, cough, dyspnea, and pneumonia. The association between COVID-19 and coagulation has been previously reported. Due to several inflammatory changes that occur in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections such as alterations in the levels of clotting factors, platelet activation leads to thrombus formation in coronary and cerebral vessels, leading to myocardial infarction and cerebrovascular accidents, respectively. Unfortunately, the progression of hypercoagulability in COVID-19 is rapid in patients with and without comorbidities. Hence, the proper monitoring of thrombotic complications in patients with COVID-19 is essential to avoid further complications. The implementation of guidelines for antithrombotic treatments based on the presentation of the disease is recommended. This review discusses the symptoms and mechanisms of upregulated coagulation in patients with COVID-19.
Keyword
Figure
Reference
-
1. Jin Y, Yang H, Ji W, et al. 2020; Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 12:372. DOI: 10.3390/v12040372. PMID: 32230900. PMCID: PMC7232198.
Article2. Mills S. 2020; COVID-19, public health measures, legal considerations: a medical perspective. Judic Rev. 25:71–9. DOI: 10.1080/10854681.2020.1760575.
Article3. Sohrabi C, Alsafi Z, O'Neill N, et al. 2020; World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 76:71–6. DOI: 10.1016/j.ijsu.2020.02.034. PMID: 32112977. PMCID: PMC7105032.
Article4. Prompetchara E, Ketloy C, Palaga T. 2020; Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 38:1–9. DOI: 10.12932/AP-200220-0772. PMID: 32105090.
Article5. Weiss SR, Leibowitz JL. 2011; Coronavirus pathogenesis. Adv Virus Res. 81:85–164. DOI: 10.1016/B978-0-12-385885-6.00009-2. PMID: 22094080. PMCID: PMC7149603.
Article6. Lam TT, Jia N, Zhang YW, et al. 2020; Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature. 583:282–5. DOI: 10.1038/s41586-020-2169-0. PMID: 32218527.7. Karia R, Gupta I, Khandait H, Yadav A, Yadav A. 2020; COVID-19 and its modes of transmission. SN Compr Clin Med. 1–4. DOI: 10.1007/s42399-020-00498-4. PMID: 32904860. PMCID: PMC7461745.
Article8. Abassi ZA, Skorecki K, Heyman SN, Kinaneh S, Armaly Z. 2020; Covid-19 infection and mortality: a physiologist's perspective enlightening clinical features and plausible interventional strategies. Am J Physiol Lung Cell Mol Physiol. 318:L1020–2. DOI: 10.1152/ajplung.00097.2020. PMID: 32207983. PMCID: PMC7200872.
Article9. Fu Y, Cheng Y, Wu Y. 2020; Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential thera-peutic tools. Virol Sin. 35:266–71. DOI: 10.1007/s12250-020-00207-4. PMID: 32125642. PMCID: PMC7090474.
Article10. Huang C, Wang Y, Li X, et al. 2020; Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 395:497–506. DOI: 10.1016/S0140-6736(20)30183-5. PMID: 31986264. PMCID: PMC7159299.
Article11. Qin C, Zhou L, Hu Z, et al. 2020; Clinical characteristics and outcomes of COVID-19 patients with a history of stroke in Wuhan, China. Stroke. 51:2219–23. DOI: 10.1161/STROKEAHA.120.030365. PMID: 32466735. PMCID: PMC7282412.
Article12. Zhu H, Rhee JW, Cheng P, et al. 2020; Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response. Curr Cardiol Rep. 22:32. DOI: 10.1007/s11886-020-01292-3. PMID: 32318865. PMCID: PMC7171437.
Article13. Al-Samkari H, Karp Leaf RS, Dzik WH, et al. 2020; COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 136:489–500. DOI: 10.1182/blood.2020006520. PMID: 32492712. PMCID: PMC7378457.
Article14. Hess DC, Eldahshan W, Rutkowski E. 2020; COVID-19-related stroke. Transl Stroke Res. 11:322–5. DOI: 10.1007/s12975-020-00818-9. PMID: 32378030. PMCID: PMC7202903.
Article15. Xu P, Zhou Q, Xu J. 2020; Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 99:1205–8. DOI: 10.1007/s00277-020-04019-0. PMID: 32296910. PMCID: PMC7156897.
Article16. Colling ME, Kanthi Y. 2020; COVID-19-associated coagulopathy: an exploration of mechanisms. Vasc Med. 25:471–8. DOI: 10.1177/1358863X20932640. PMID: 32558620. PMCID: PMC7306998.
Article17. Lippi G, Plebani M, Henry BM. 2020; Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 506:145–8. DOI: 10.1016/j.cca.2020.03.022. PMID: 32178975. PMCID: PMC7102663.
Article18. Wang J, Hajizadeh N, Moore EE, et al. 2020; Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 18:1752–5. DOI: 10.1111/jth.14828. PMID: 32267998. PMCID: PMC7262152.
Article19. Goeijenbier M, van Wissen M, van de Weg C, et al. 2012; Review: viral infections and mechanisms of thrombosis and bleeding. J Med Virol. 84:1680–96. DOI: 10.1002/jmv.23354. PMID: 22930518. PMCID: PMC7166625.
Article20. Minasyan H, Flachsbart F. 2019; Blood coagulation: a powerful bactericidal mechanism of human innate immunity. Int Rev Immunol. 38:3–17. DOI: 10.1080/08830185.2018.1533009. PMID: 30633597.
Article21. Levi M, van der Poll T. 2017; Coagulation and sepsis. Thromb Res. 149:38–44. DOI: 10.1016/j.thromres.2016.11.007. PMID: 27886531.
Article22. Umapathi T, Kor AC, Venketasubramanian N, et al. 2004; Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol. 251:1227–31. DOI: 10.1007/s00415-004-0519-8. PMID: 15503102. PMCID: PMC7088071.
Article23. Dalakas MC, Clark WM. 2003; Strokes, thromboembolic events, and IVIg: rare incidents blemish an excellent safety record. Neurology. 60:1736–7. DOI: 10.1212/01.WNL.0000074394.15882.83. PMID: 12796522.
Article24. Okuda D, Flaster M, Frey J, Sivakumar K. 2003; Arterial thrombosis induced by IVIg and its treatment with tPA. Neurology. 60:1825–6. DOI: 10.1212/01.WNL.0000068334.04500.08. PMID: 12796540.
Article25. Han H, Yang L, Liu R, et al. 2020; Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 58:1116–20. DOI: 10.1515/cclm-2020-0188. PMID: 32172226.
Article26. Guo T, Fan Y, Chen M, et al. 2020; Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5:811–8. DOI: 10.1001/jamacardio.2020.1017. PMID: 32219356. PMCID: PMC7101506.
Article27. Klok FA, Kruip MJHA, van der Meer NJM, et al. 2020; Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 191:145–7. DOI: 10.1016/j.thromres.2020.04.013. PMID: 32291094. PMCID: PMC7146714.
Article28. Gupta N, Zhao YY, Evans CE. 2019; The stimulation of thrombosis by hypoxia. Thromb Res. 181:77–83. DOI: 10.1016/j.thromres.2019.07.013. PMID: 31376606.
Article29. Milbrandt EB, Reade MC, Lee M, et al. 2009; Prevalence and significance of coagulation abnormalities in community-acquired pneumonia. Mol Med. 15:438–45. DOI: 10.2119/molmed.2009.00091. PMID: 19753144. PMCID: PMC2743205.
Article30. Zhou F, Yu T, Du R, et al. 2020; Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 395:1054–62. DOI: 10.1016/S0140-6736(20)30566-3. PMID: 32171076. PMCID: PMC7270627.
Article31. Avula A, Nalleballe K, Narula N, et al. 2020; COVID-19 presenting as stroke. Brain Behav Immun. 87:115–9. DOI: 10.1016/j.bbi.2020.04.077. PMID: 32360439. PMCID: PMC7187846.
Article32. Mao L, Jin H, Wang M, et al. 2020; Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 77:683–90. DOI: 10.1001/jamaneurol.2020.1127. PMID: 32275288. PMCID: PMC7149362.
Article33. Tripodi A. 2011; D-dimer testing in laboratory practice. Clin Chem. 57:1256–62. DOI: 10.1373/clinchem.2011.166249. PMID: 21719689.
Article34. Al-Ani F, Chehade S, Lazo-Langner A. 2020; Thrombosis risk associated with COVID-19 infection. A scoping review. Thromb Res. 192:152–60. DOI: 10.1016/j.thromres.2020.05.039. PMID: 32485418. PMCID: PMC7255332.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coronavirus Disease 2019-Liver InjuryLiterature Review and Guidelines Based on the Recommendations of Hepatological Societies
- Epidemiology, Virology, and Clinical Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; Coronavirus Disease-19)
- Severe asthma exacerbation associated with COVID-19 in children: A case report
- Lessons Learned from SARS-CoV and MERS-CoV: Preparation for SARS-CoV-2 induced COVID-19
- An Unexpected Outbreak of Middle East Respiratory Syndrome Coronavirus Infection in the Republic of Korea, 2015