J Korean Med Sci.
2021 Jun;36(23):e171. 10.3346/jkms.2021.36.e171.
First Organ Donation after Circulatory Death Following Withdrawal of Life-sustaining Treatment in Korea: a Case Report
- Affiliations
-
- 1Transplantation Center, Korea University Anam Hospital, Seoul, Korea
- 2Department of Critical Care Medicine & Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 3Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 4Korea Organ and Tissue Donation Agency, Seoul, Korea
- 5Division of Acute Care Surgery, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2516682
- DOI: http://doi.org/10.3346/jkms.2021.36.e171
Abstract
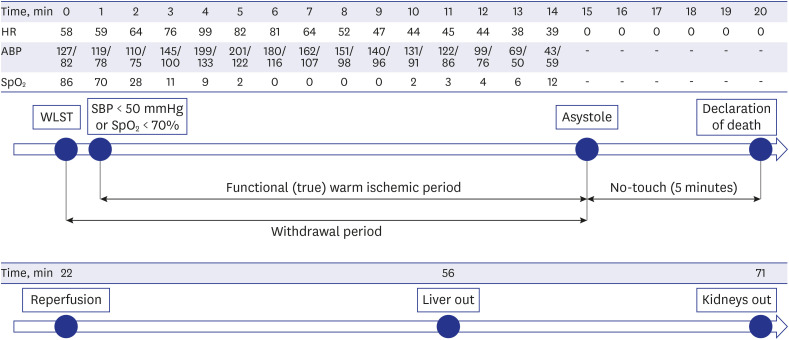
- In February 2018, the Withdrawal of the Life-sustaining Treatment (WLST) Decision Act was legalized in Korea. Donation after circulatory death (DCD) after WLST was classified as DCD category III. We report the first case of successful organ donation after WLST in Korea. A 52-year-old male who experienced cerebral hemorrhage was a potential brain-dead donor with donation consent. During the first brain death examination, Babinski reflex was present, which disappeared two days later. Then, electroencephalography was performed five times at intervals of 2 to 3 days, according to the recommendation of a neurologist. The patient was transferred to the OR at 19:30 July 3, 2020. At 20:00, an intensive care unit specialist performed extubation and discontinued vasopressors. Oxygen saturation fell to < 70% in 1 minute, which signaled the beginning of functional warm ischemia. At 20:15, asystole was confirmed; after 5 minutes of “no-touch time,” circulatory death was declared. Organ procurement surgery was initiated, with surgeons performing the recipient surgery ready in the adjacent OR. Through the first successful DCD case, we expected that DCD will be actively implemented in Korea, saving the lives of patient waiting for transplantation and resolving the imbalance between organ receipt and donation.
Figure
Cited by 2 articles
-
The first use of hypothermic machine perfusion in Korea to recover a procured kidney graft and prevent prolonged cold ischemic time: a case report
Young-Heun Shin, Taerim Ko, John Hee Park, Won-Bae Chang
Korean J Transplant. 2023;37(2):129-134. doi: 10.4285/kjt.23.0017.Recent Trends in the Withdrawal of Life-Sustaining Treatment in Patients with Acute Cerebrovascular Disease : 2017–2021
Seung Hwan Kim, Ji Hwan Jang, Young Zoon Kim, Kyu Hong Kim, Taek Min Nam
J Korean Neurosurg Soc. 2024;67(1):73-83. doi: 10.3340/jkns.2023.0074.
Reference
-
1. Manara AR, Murphy PG, O'Callaghan G. Donation after circulatory death. Br J Anaesth. 2012; 108(Suppl 1):i108–i121. PMID: 22194426.
Article2. Truog RD, Miller FG, Halpern SD. The dead-donor rule and the future of organ donation. N Engl J Med. 2013; 369(14):1287–1289. PMID: 24088088.
Article3. Lomero M, Gardiner D, Coll E, Haase-Kromwijk B, Procaccio F, Immer F, et al. Donation after circulatory death today: an updated overview of the European landscape. Transpl Int. 2020; 33(1):76–88. PMID: 31482628.
Article4. International registry in organ donation and transplantation (IRODaT). Newsletter 2019. Updated 2019. Accessed March 4, 2021. https://www.irodat.org/img/database/pdf/NEWSLETTER2019-June.pdf.5. Korean Network for Organ Sharing (KONOS). KONOS waiting list in quarterly statistics data. Updated 2019. Accessed March 4, 2021. https://www.konos.go.kr.6. Kim JM, Kim SJ. The use of non-heart beating donors to expand the donor pool. J Korean Soc Transplant. 2010; 24(3):165–172.
Article7. National Life Insurance Management Agency. One year of life-sustaining treatment decision system implementation, progress and status of operation. Updated 2019. Accessed March 4, 2021. https://www.lst.go.kr/comm/referenceDetail.do?pgNo=1&cate=&searchOption=0&searchText=&bno=946.8. Fugate JE, Stadtler M, Rabinstein AA, Wijdicks EF. Variability in donation after cardiac death protocols: a national survey. Transplantation. 2011; 91(4):386–389. PMID: 21127460.
Article9. Lomero M, Gardiner D, Coll E, Haase-Kromwijk B, Procaccio F, Immer F, et al. Donation after circulatory death today: an updated overview of the European landscape. Transpl Int. 2020; 33(1):76–88. PMID: 31482628.
Article10. DeVita MA. The death watch: certifying death using cardiac criteria. Prog Transplant. 2001; 11(1):58–66. PMID: 11357558.
Article11. Sheth KN, Nutter T, Stein DM, Scalea TM, Bernat JL. Autoresuscitation after asystole in patients being considered for organ donation. Crit Care Med. 2012; 40(1):158–161. PMID: 21926577.
Article12. Ethics Committee, American College of Critical Care Medicine. Society of Critical Care Medicine. Recommendations for nonheartbeating organ donation. A position paper by the Ethics Committee, American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. 2001; 29(9):1826–1831. PMID: 11546995.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organ donation after controlled circulatory death (Maastricht classification III) following the withdrawal of life-sustaining treatment in Korea: a suggested guideline
- Factors Influencing Withdrawal of Life-Sustaining Treatment in Tertiary General Hospital Workers -Knowledge and Attitude of Organ Donation and Transplantation, Awareness of Death, Knowledge and Perception of Hospice Palliative Care-
- The first donation after circulatory death following withdrawal of life-sustaining treatment in Korea
- Withdraw life sustaining treatment and organ donation
- The Relationship among Attitudes toward the Withdrawal of Life-sustaining Treatment, Death Anxiety, and Death Acceptance among Hospitalized Elderly Cancer Patients